The term brachycephalic ocular syndrome (BOS) is used to describe the bilateral eye problems, associated with combinations of poor conformation and other factors, including:
- Shallow orbit causing a ‘physiologic’ exophthalmos
- Exoptropia
- Lagophthalmos
- Macropalpebral fissure
- Medial lower lid entropion
- Caruncular trichiasis
- Nasal fold trichiasis
- Involution of the medial canthus
- Poor corneal sensation
- Poor tear film (qualitative and quantitative deficiencies).
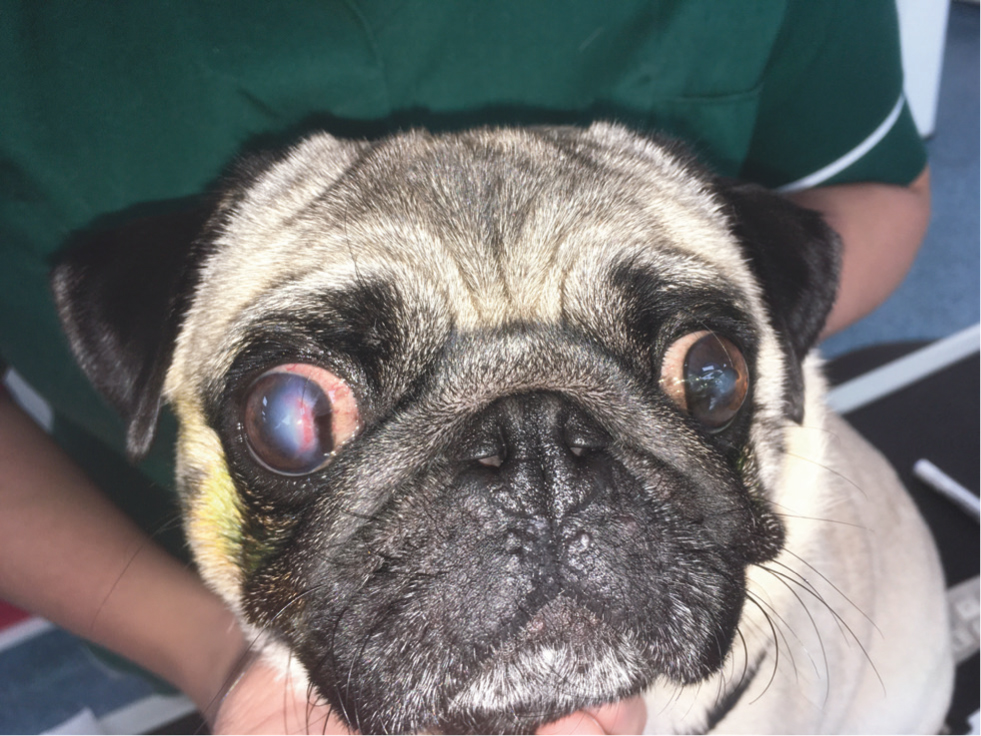
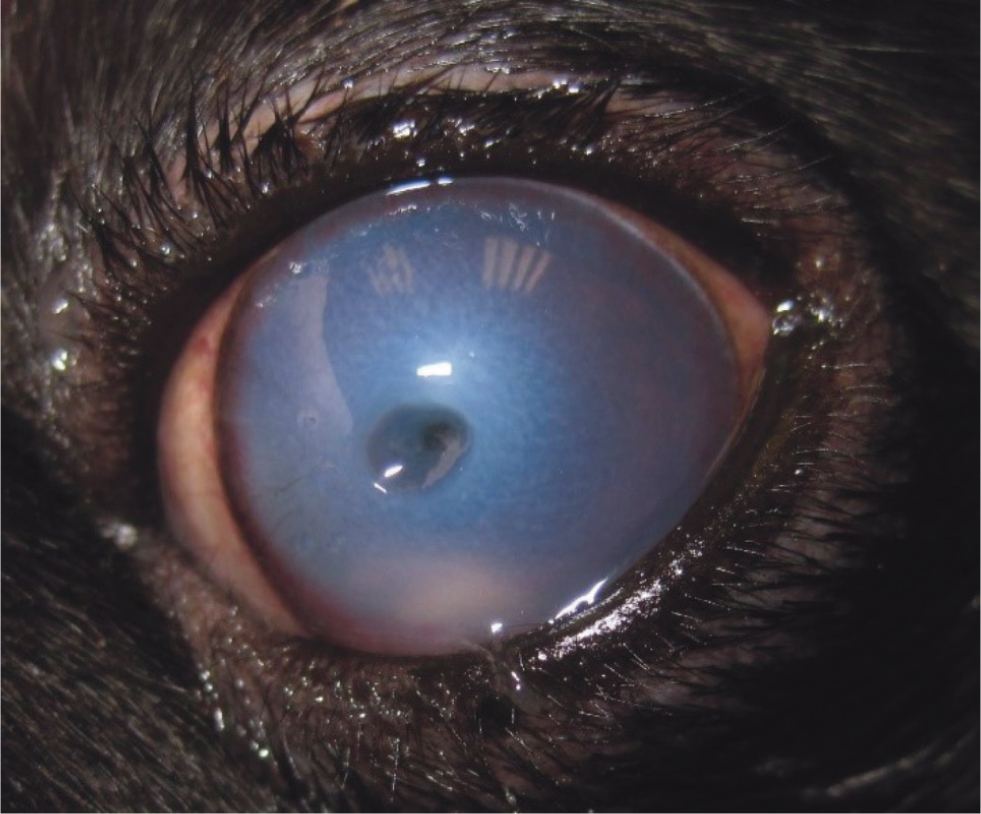
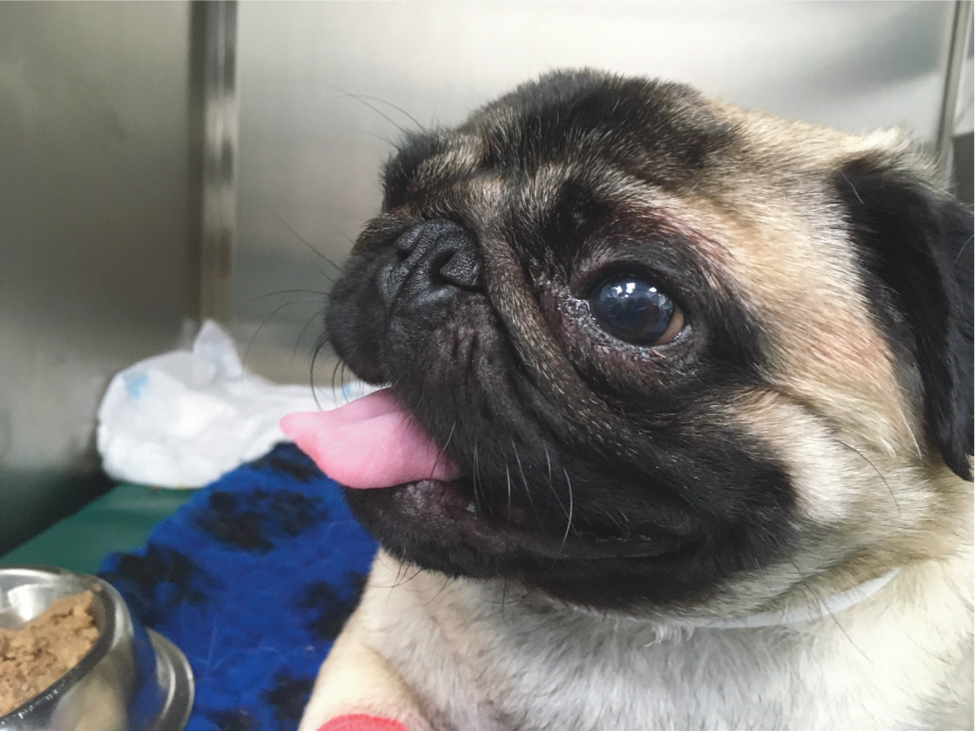
Small brachycephalic breeds such as the Pug, French Bulldog, Shih Tzu and Pekingese oft en present with these features (Carrington et al, 1989; Krohne, 2008; Stades and Van Der Woerdt, 2013). Although it is recognised as a term by many ophthalmologists, BOS has not been officially described as a distinct entity and is sometimes referred to as ‘so-called’ BOS. Affected dogs oft en present with poor corneal health (Carrington et al, 1989; Krohne, 2008; Stades and Van Der Woerdt, 2013) (Figure 1).
BOS does not affect every brachycephalic breed, for example, the Boxer's conformation is not usually associated with all the findings described above. Brachycephalic cats such as Persians may also have ocular disease resulting from their conformation, the specifics of which are outside the scope of this article.
The small brachycephalic dog breeds are currently very popular. As an example, figures from The Kennel Club (2020) show that in the 10 years between 2010 and 2019 there was a 1527% increase in French Bulldog registrations.
In addition to their entertaining personalities, the neonatal appearance of brachycephalic breeds may be at least part of the reason these dogs are found attractive (Packer et al, 2017). Babyish features such as an enlarged forehead, eyes and head size relative to the trunk have an innate appeal (Sternglanz et al, 1977). This facial morphology may increase the frequency of eye disease. Ophthalmological disease is the most prevalent group-level disease in Pugs (16.25%), with corneal disorder being the second most prevalent diagnosis-level disorder (8.72%) (O'Neill et al, 2016). Client education about the problems associated with these breeds, especially before purchase, is important.
Why do ocular problems develop?
The cornea, tears and eyelids are a functional unit. A good analogy would be the windscreen of a car, which relies on wipers and washer water and additives to stay clear and functional. There are multiple factors affecting the close relationships in this unit, which contribute to the issues seen in BOS.
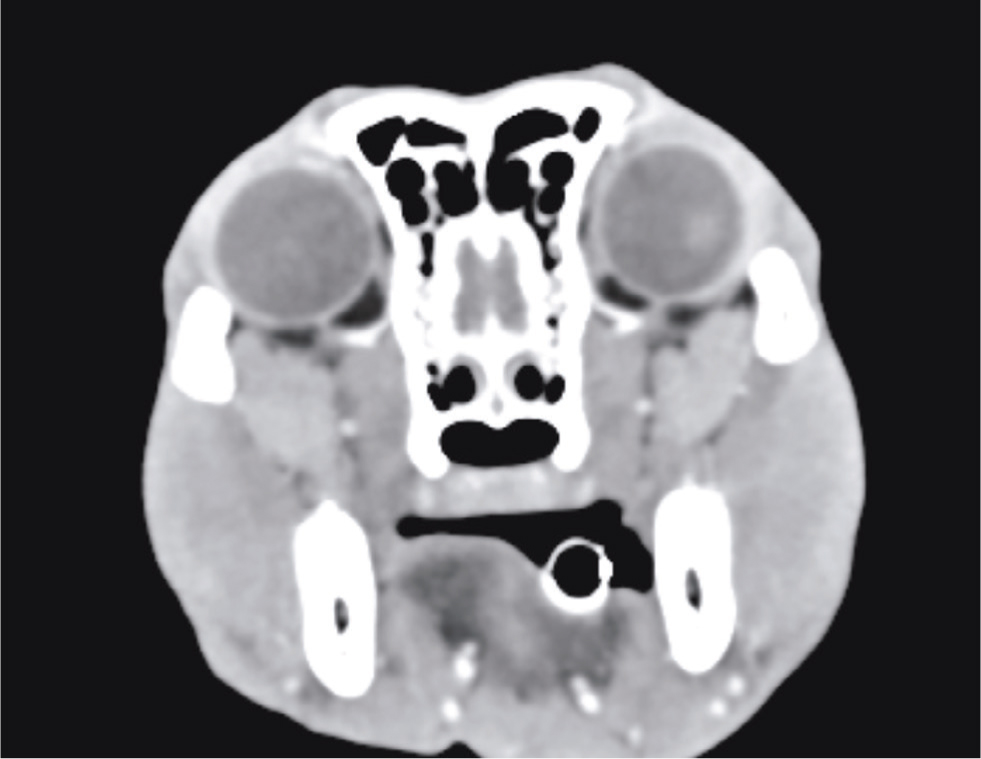
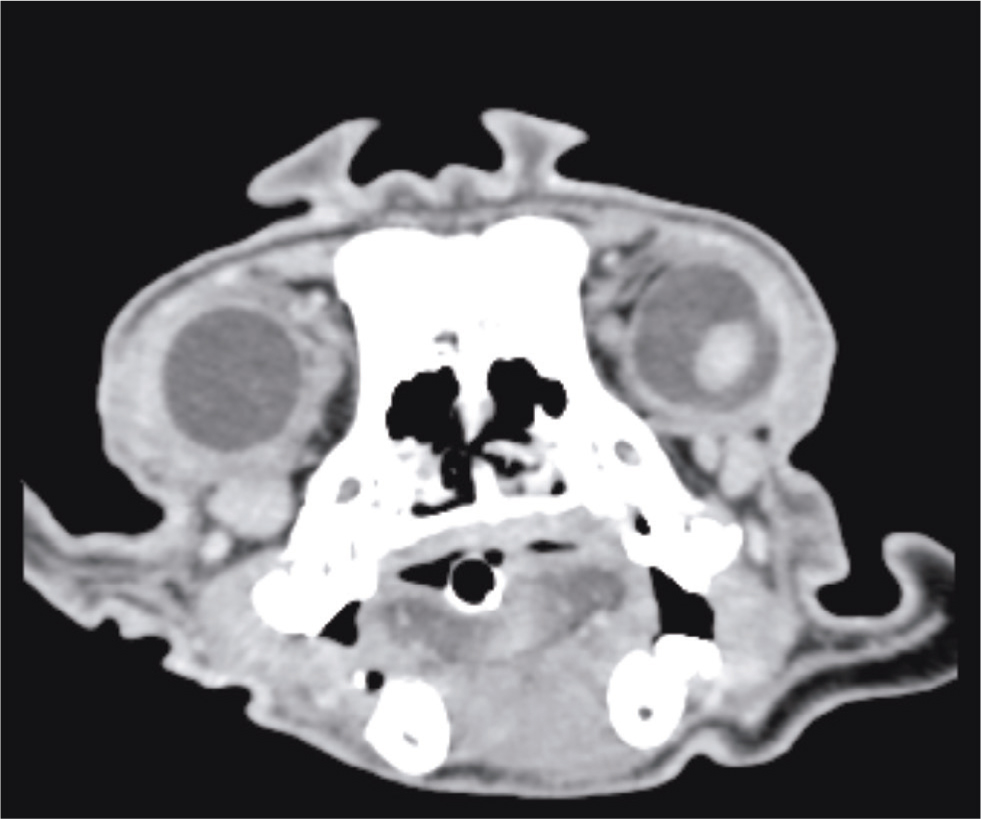
Skull conformation
The small brachycephalic breeds oft en have orbits so shallow the globe has barely any bony protection (physiologic exophthalmos). Short craniofacial ratios are a predisposing factor for corneal ulceration (Packer et al, 2015) (Figures 2 and 3). Exotropia (an outward strabismus) is not an uncommon finding.
Eyelid conformation
The eyelids are attached to the skull via the canthal tendons and the abnormal position of the globe relative to the skull means that the lids are held in a position that leads to medial entropion. Two surveys of Pugs have reported incidences of medial entropion of 94.1% and 100% (Krecny et al, 2015; Maini et al, 2019). Trichiasis, whether caused by entropion or other causes, can be a painful condition and may cause corneal ulceration if left untreated.
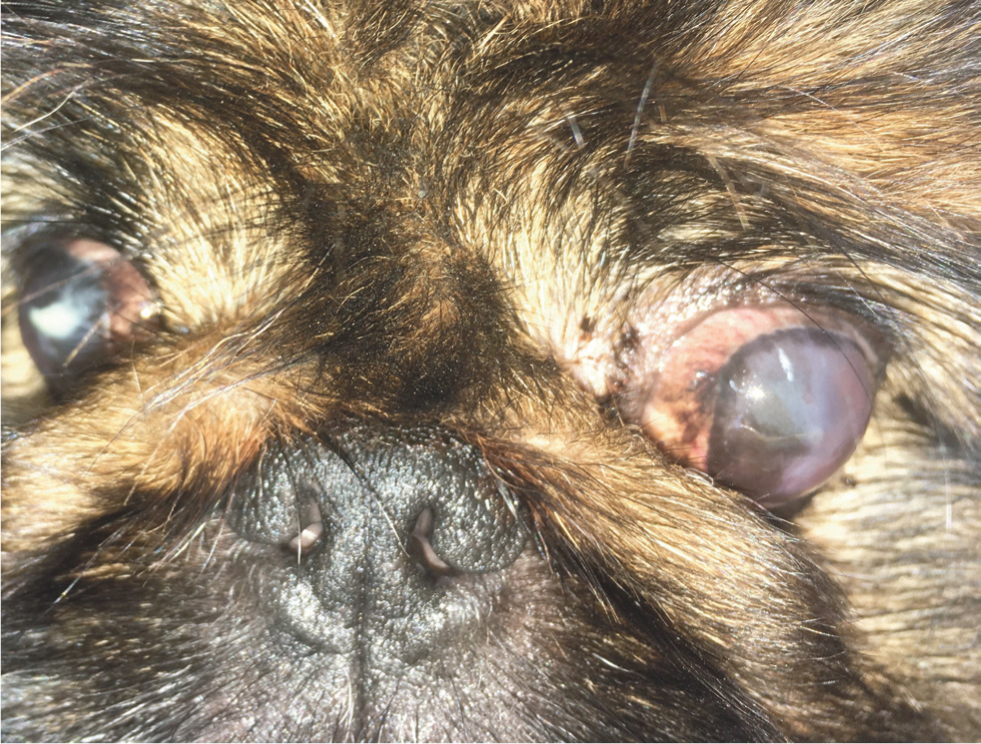
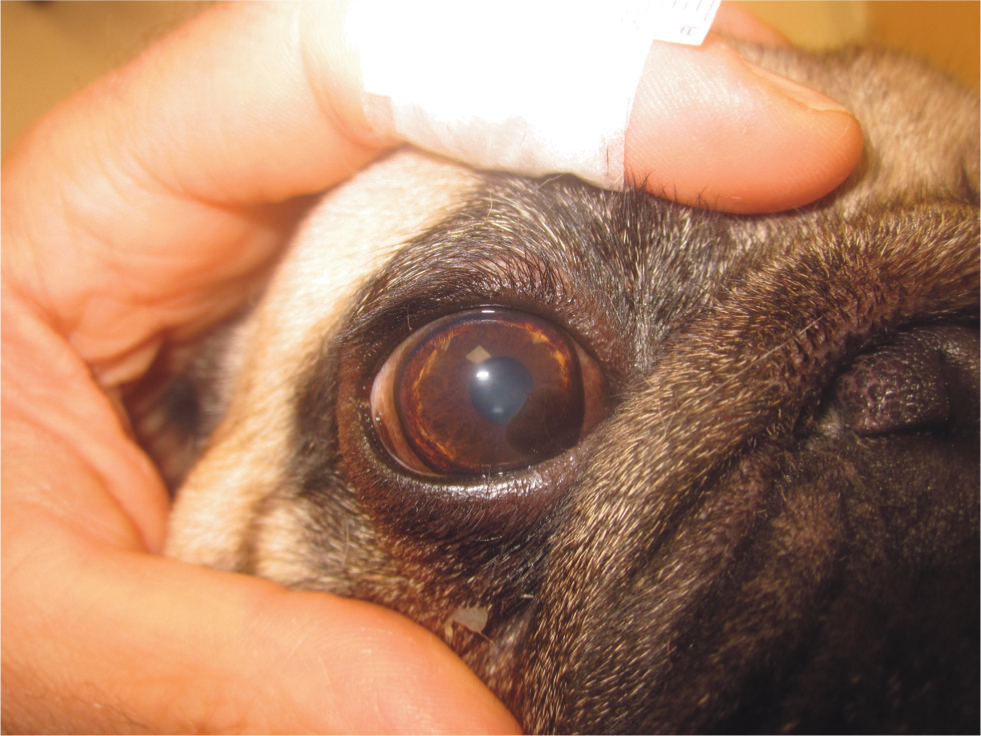
Small breeds generally have small palpebral fissure widths; the Shih Tzu and Pekingese are reported to have relatively larger palpebral fissure widths compared to other small breeds (these were the only two small brachycephalic breeds included in this study) (Stades et al, 1993). Pugs with a smaller relative fissure width (palpebral fissure width:cranial length) have a reduced probability of corneal ulceration (Packer et al, 2015). Increasing visible sclera is a risk factor for corneal ulceration in brachycephalic dogs (Packer et al, 2015), related to both eyelid conformation and orbital depth (Figure 4). It has been suggested that the corneal exposure brought on by larger palpebral fissure and physiologic exophthalmos may result in tear film abnormalities in the central cornea, predisposing damage and bacterial contamination (Iwashita et al, 2020).

Nasal fold
Dogs with nasal folds are nearly five times more likely to be affected by corneal ulcers than those without (Packer et al, 2015). In some breeds, such as the Pekingese and Pug, the nasal fold is large and hairy, often causing direct trichiasis from the skin to the cornea (Figure 5). In other breeds there may not be direct contact but nasal folds can lead to crowding of the medial canthal area, reflecting other potential factors such as degree of brachycephaly rather than being a risk factor in their own right.
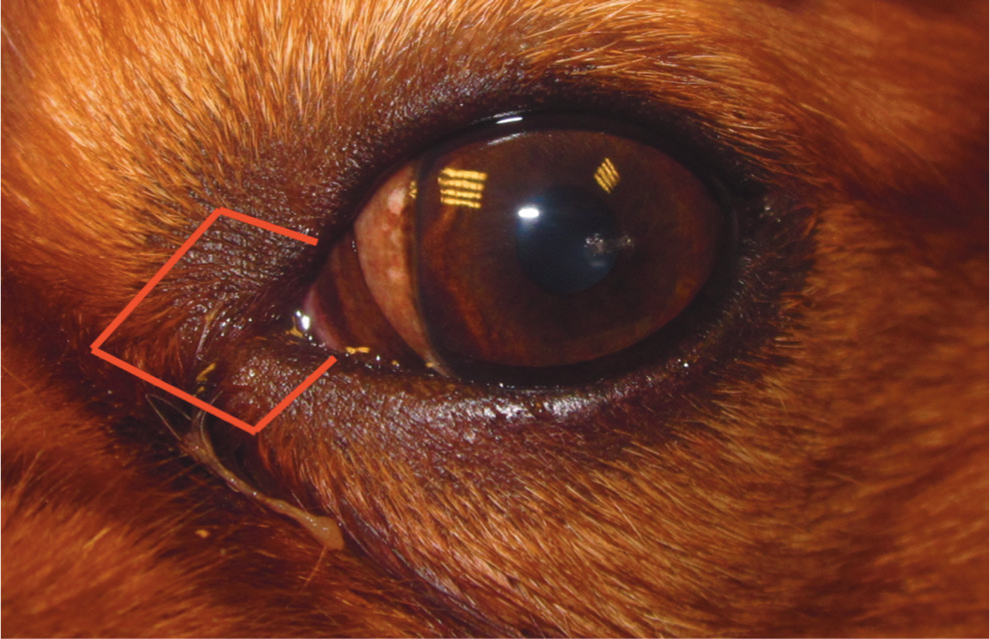
Caruncular trichiasis
In addition to hairs contacting the cornea from eyelids and nasal folds, brachycephalic breeds may have trichiasis from caruncular hair. These hairs may be incidental but may disturb the tear film, wick tears away from the cornea and potentially abrade the cornea, contributing to corneal damage. In older dogs, previously tolerated, insignificant caruncular hairs are only likely to become problematic if there have been other changes for example, in the tear film quality or quantity.
Corneal sensation
Brachycephalic dogs have reduced corneal sensitivity compared to mesocephalic and dolicocephalic dogs, meaning they fail to respond to corneal exposure or foreign material sitting on the ocular surface with blinking or reflex tearing (Barrett et al, 1991; Bolzanni et al, 2020). Reduced corneal nerve fibre densities have been demonstrated in brachycephalic dogs, compared to mesocephalic, but this difference was not significant (Kafarnik et al, 2008).
Qualitative and quantitative tear film deficiencies
The tear film is a complex structure with several roles in maintaining corneal health (Willcox et al, 2017). It is classically considered a tri-laminar structure consisting of an outer lipid layer (secreted by the meibomian glands, preventing evaporation of the underlying layers and overflow of the tear film onto the eyelids), the middle aqueous layer (primarily secreted from the lacrimal gland and the gland of the nictitating membrane) and an inner mucus layer (primarily but not exclusively secreted by conjunctival goblet cells stabilising the tear film and facilitating tear spreading) (Gum and MacKay, 2013). This classical view is a simplification of reality, the aqueous and mucin layers are now considered a single mucoaqueous layer (Willcox et al, 2017). There is a complex interface between the tear film and cornea at the glycocalyx, which holds the tear film in place. This interaction being dependent on both tear film quality and cornea ‘wettability’ (King-Smith et al, 2018).
Aqueous tear secretion is lower in brachycephalic dogs (Bolzanni et al, 2020) and they have poorer quality tear films (Labelle et al, 2013; Palella Gómez et al, 2020). Kerato-conjunctivitis sicca in dogs is an immune-mediated disease in a large percentage of cases (Giuliano, 2013), which many of brachycephalic breeds are predisposed to (Kaswan and Salisbury, 1990; Sanchez et al, 2007). For example, the Cavalier King Charles Spaniel has been quoted as having a relative risk of kerato-conjunctivitis sicca 11.5 times that of the general canine population, with the Shih Tzu being 6.2 times, the Pug 5.2 and Pekingese 4 times more likely (Kaswan and Salisbury, 1990).
Several techniques are available for the assessment of the tear film. The Schirmer tear test I is the most common quantitative tear film assessment, being performed without the application of topical anaesthesia, the test is a measure of residual tears in the conjunctival sac, basal tear productions and reflex tearing in response to the test strip being placed (Williams, 2005). Quoted normal Schirmer tear test I values vary between 18.64±4.47 mm/min and 23.90±5.12 mm/min (Bolzanni et al, 2020; Featherstone and Heinrich, 2013). Tear film break-up time, usually examined using fluorescein, gives a good indication of the quality of the tears (Guillon, 1998; King-Smith et al, 2018; Romkes et al, 2014; Wolffsohn et al, 2017). The fluorescein tear film break-up time is the time for a break in the tear film to be noted when the eyelids are prevented from blinking following application of fluorescein, using magnification and cobalt blue light for illumination. The normal fluorescein tear film break-up time in dogs has been quoted as 19.7±5 seconds, less than 5 seconds is considered significant (Moore, 1990). Clinically, disrupted corneal reflections or mucoid strands may indicate a qualitative tear film issue.
Blink efficiency
The abnormal position of the globe relative to the skull means that the lids are in a position that prohibits efficient blinking and tear film distribution (Figure 6). Poor distribution of tears over the cornea may increase the vulnerability of the central cornea to exposure. In humans, incomplete blinks have been demonstrated to reduce the tear film break-up time, although the blink rate did not (Wang et al, 2018). Some brachycephalic dogs are unable to close their eyes completely (lagophthalmos) and sleep with them partially open.

Ectopic cilia and distichiasis
Ectopic cilia and distichiasis are common in Pugs (Krecny et al, 2015), Shih Tzus and Pekingese (Stades and Van Der Woerdt, 2013). Both conditions may act as exacerbating factors in BOS, contributing to corneal ulceration by direct trauma to the cornea and/or disturbance of the tear film. Like caruncular trichiasis, distichiasis is often an incidental finding and, in older dogs, is only likely to become problematic if there have been other changes, for example in the tear film quality or quantity.
Ocular conditions associated with brachycephalic ocular syndrome
Corneal ulceration
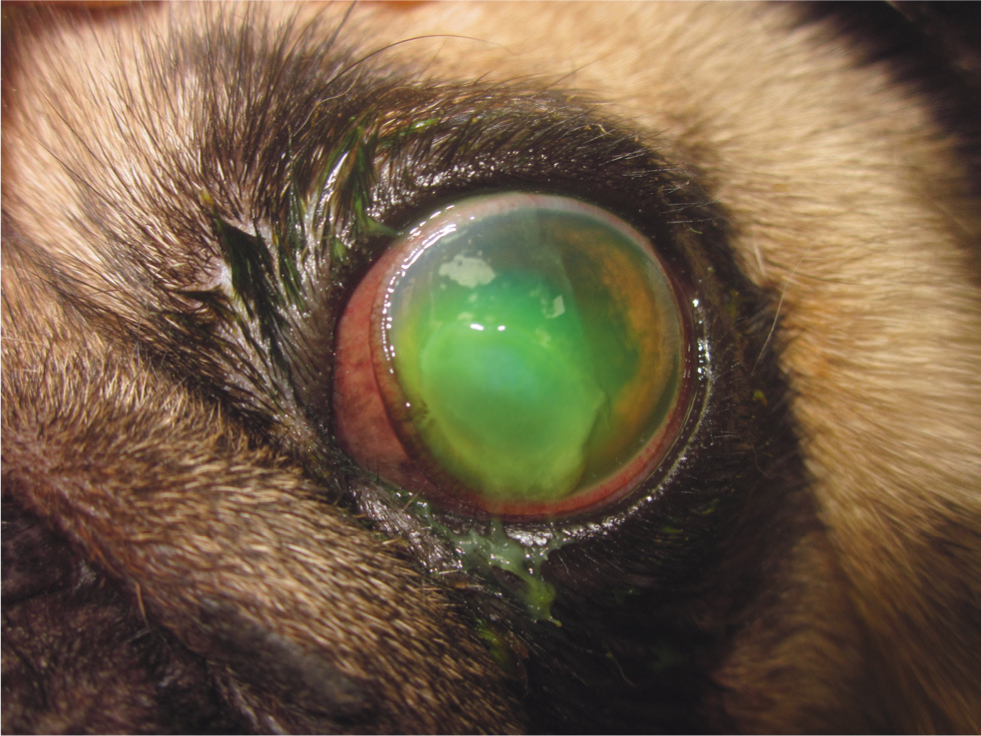
Brachycephalic breeds have been reported to be up to 20 times more likely to be affected by corneal ulceration than non-brachycephalic breeds (Packer et al, 2015). Ulcers can rapidly deteriorate, potentially to the point of corneal rupture, if appropriate treatment is not given and the underlying causes are not identified and corrected (Figure 7). Corneal ulcers in brachycephalic breeds are more likely to be deeper compared to non-brachycephalic breeds (Iwashita et al, 2020). There are breed differences, for example the French Bulldog tends to be affected by superficial ulceration whereas Pugs, Shih Tzus and Pekingese are more frequently affected by deep ulceration (Iwashita et al, 2020). This may be because French Bulldogs generally have a smaller relative palpebral fissure width, or it may reflect the many different factors contributing to BOS.
Corneal pigmentation
Corneal pigmentation is regarded as a symptom, developing as a result of irritating stimuli, such as chronic abrasion/exposure (as is the case in BOS), as part of wound healing or kerato-conjunctivitis sicca (Labelle et al, 2013). Owners often do not notice corneal pigmentation. The incidence of corneal pigmentation in Pugs is high, with a prevalence of 82.4% in Pugs being recorded in one study (Labelle et al, 2013) and 91.9% in another (Maini et al, 2019) (Figures 8 and 9).
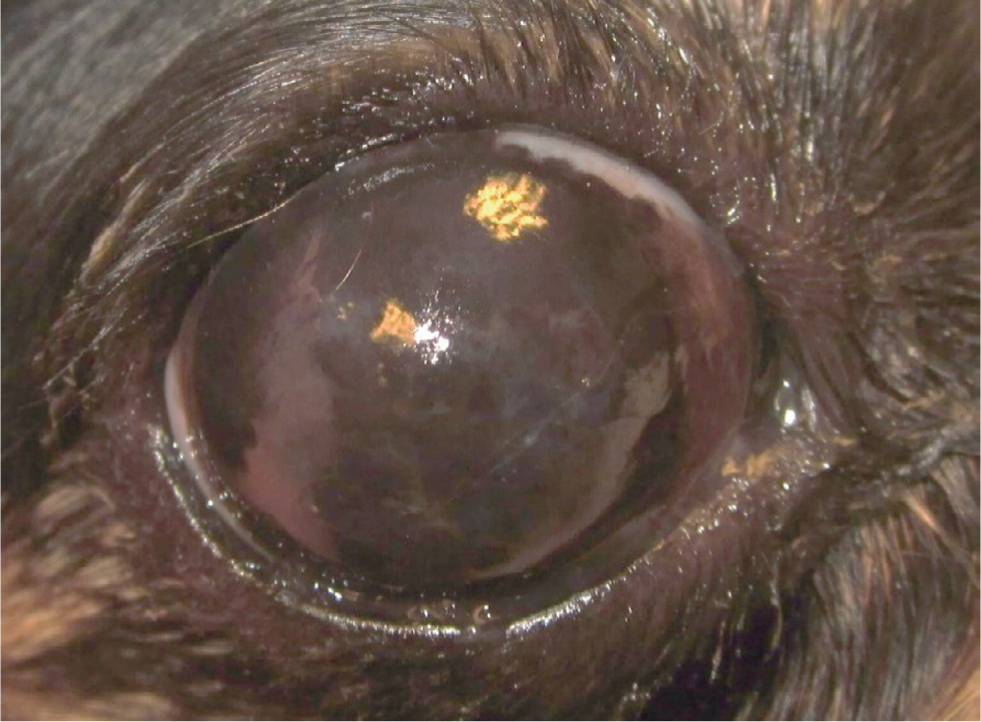
The exact risk factors for corneal pigmentation are uncertain. For example, in Pugs, associations have been suggested between corneal pigmentation and medial, lower lid entropion (Maini et al, 2019), the presence of serous ocular discharge, sex (spayed female pugs are less likely to have pigmentation) and coat colour (fawn pugs are more likely to have more severe corneal pigmentation) (Labelle et al, 2013). Corneal pigmentation maybe a genetic disease in Pugs modified by features of BOS, such as entropion and poor tear film, rather than caused by them per se (Labelle et al, 2013).
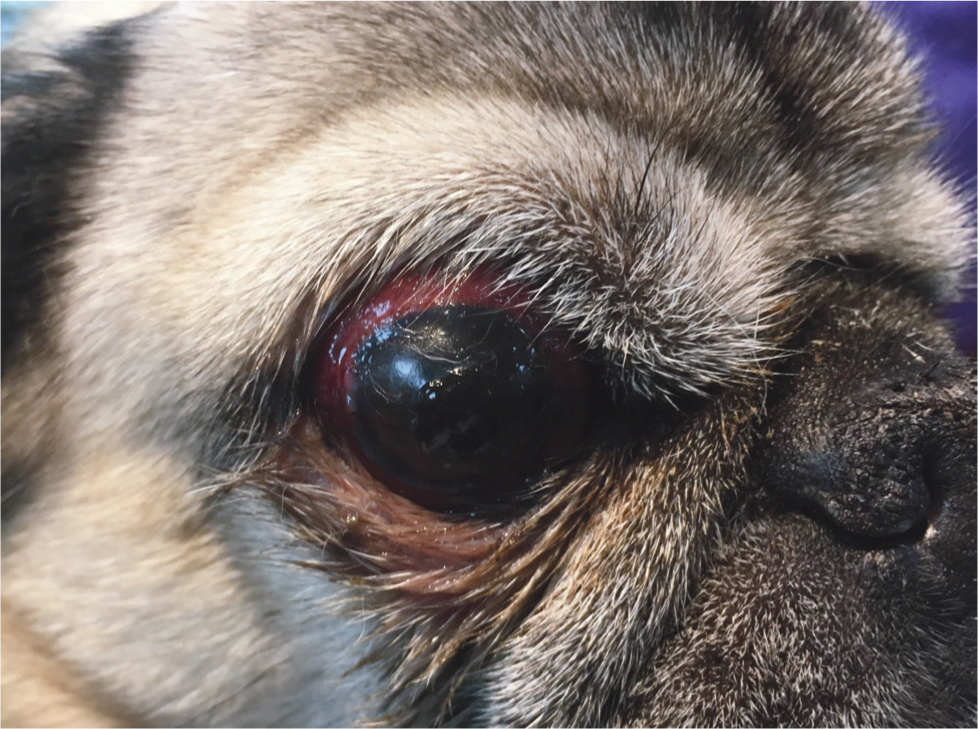
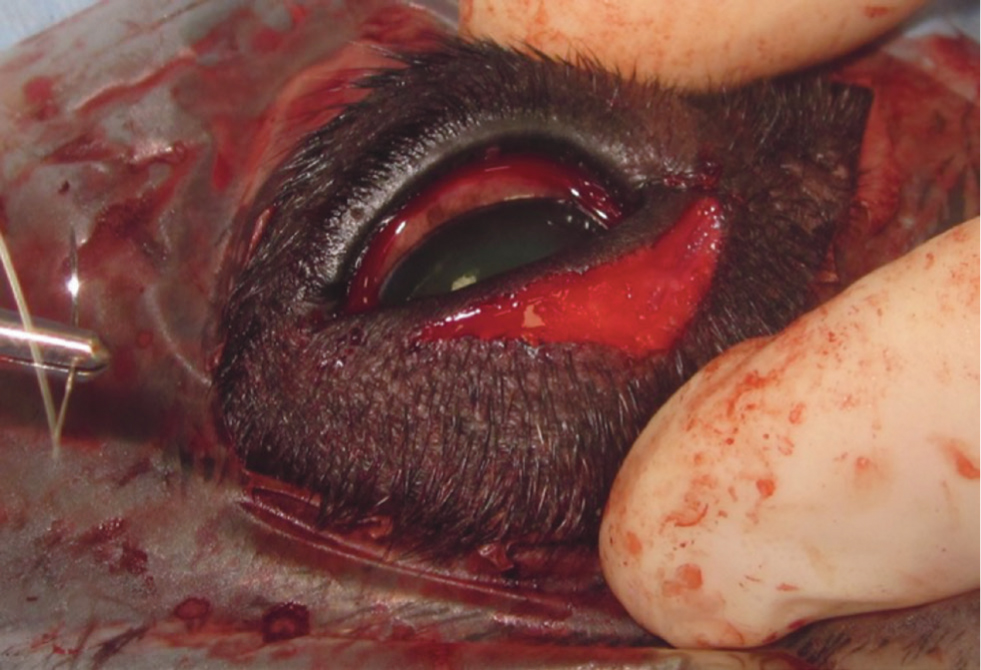
Globe proptosis
The shallow orbits and minimal bony protection of brachycephalic breeds' eyes and their relatively wide palpebral fissures means they are at a higher risk of globe proptosis (Gilger et al, 1995; Stades et al, 1993), often during minor fights with other dogs or inappropriate handling (Figure 10).
Epiphora
The medial canthal anatomy and lower lid entropion can displace the lower nasolacrimal punctae and narrow the canalicular lumen causing epiphora. Tear spillage may be exacerbated by trichiasis (Grahn and Sandmeyer, 2013).
Treatment options for brachycephalic ocular syndrome
The goal in treating BOS should be the elimination of as many of the abnormalities as possible, to improve corneal health. As well as treatment of any corneal disease that may be the reason for presentation, surgery to correct eyelid anatomy, as well as ongoing medical efforts to improve the tear film, are required. In dogs with signs of the development of poor corneal health, there is an argument for early intervention to try and prevent more serious ocular disease occurring.
Surgical management options
The main surgical option available for the management of BOS is the medial canthoplasty. Medial canthoplasty reduces the size of the palpebral fissure, reducing the risks associated with corneal exposure and globe proptosis, as well as addressing medial, lower lid entropion and medial canthal involution. Various techniques have been described (Jensen, 1979; Stades and Boevé, 1993; Van Der Woerdt, 2004; Yi et al, 2006; Saito et al, 2010). Simple excision of a diamond of skin, caruncular tissue and medial eyelid margins at the medial canthus, with loosening of the medial canthal tendon and gentle undermining of the surrounding facial skin, is effective (Figures 11 and 12). Closure is two-layered with a figure-of-8 suture at the lid margin. Long-term owner satisfaction following medial canthoplasty is good (Yi et al, 2006).

Medial canthal tendonotomy is a modification of the medial canthoplasty, the medial canthal tendon is sectioned with minimal excision of medial canthal skin, allowing the lids to sit in a more natural position relative to the cornea, reducing medial canthal involution and entropion (Saito et al, 2010).
The Hotz-Celsus procedure is useful for correcting medial lower lid entropion (Figure 13). This often needs to be performed in combination with other procedures, such as medial canthoplasty (Figures 14 and 15). Stabilisation of the lid using a tongue depressor, specialised lid plate or with your finger (carefully, to avoid cutting it) can make creating the incisions easier.

Nasal fold excision or reduction may be beneficial, by resolving nasal fold trichiasis and reducing crowding at the medial canthus. Medial canthoplasty reduces the likelihood of nasal fold hairs touching the cornea, meaning nasal fold excision is not always necessary.
To attain precise lid apposition fine (6/0) sutures should be placed using magnification. Suture removal can be difficult in small brachycephalic dogs and absorbable sutures maybe appropriate. Care must be taken to ensure none of the sutures contact the cornea, risking ulceration. Lid surgery can be performed at the same time as corneal repair, if clinically appropriate.
Ectopic cilia maybe removed en-bloc via the palpebral surface. Various methods for the treatment of distichiasis are available including repeat plucking, electrocautery, cryosurgery and sharp surgery. There are limitations to all the techniques and where there is doubt about the significance of distichiasis, it is advisable to assess the response to simple plucking of the hairs initially. Any surgery for distichiasis will damage the meibomian glands and have an effect on tear film quality (Carrington et al, 1989; Palella Gómez et al, 2020).
Conformation altering surgery performed on Kennel Club registered dogs should be reported to the Kennel Club. This can be done online at https://www.thekennelclub.org.uk/forms/form-6-veterinary. The level of reporting by owners far exceeds that done by veterinary surgeons and is something veterinary surgeons should get into the habit of doing.
Medical management options
Ciclosporin is the licensed drug (Optimmune) for aqueous deficiency, acting via immune-modulatory and direct lacrimogenic effects (Giuliano, 2013; Herring, 2013). It also improves tear quality by increasing conjunctival goblet cell numbers (Moore et al, 2001). A reduction in corneal vascularisation and pigmentation in kerato-conjunctivitis sicca cases has been reported over several months use (Salisbury et al, 1990; Morgan and Abrams, 1991; Rankin, 2013), it may be useful in maintaining corneal clarity following corneal surgery and anecdotally may reduce or slow the progression of corneal pigmentation.
Tacrolimus may be of use in kerato-conjunctivitis sicca cases with very low Schirmer tear test I results, refractory to ciclosporin (Berdoulay et al, 2005) and is anecdotally reported to be better at limiting corneal pigmentation long term.
Ongoing lubrication of brachycephalic corneas is advisable. Hyaluronate is an attractive tear supplement given its thixotropic properties and retention times (Herring, 2013), many preservative-free preparations are available. Hyaluronate may have a protective effect on the corneal epithelium by reducing epithelial cell disruption and maintenance of the mucus layer (McDonald et al, 2002). ‘Crosslinking’ of the hyaluronate molecules has been suggested as advantageous (Williams et al, 2017; Wirostko et al, 2014; Williams and Mann, 2014; 2013).
Treatment of brachycephalic ocular syndrome associated corneal disease
Many cases of BOS are presented with corneal ulceration, so an understanding of the appropriate initial medical management of corneal ulceration and the surgical options available is important. All corneal ulcers in brachycephalic dogs should be considered complex cases and treated carefully with regular re-examinations, as there is a possibility of rapid deterioration.
Medical management
Where possible, culture, sensitivity and cytology should be performed on all corneal ulcers in brachycephalic dogs. Bacterial morphology on cytology can be used to guide antibiotic choice pending culture and can screen for fungal elements. Cocci (Staphylococcus or Streptococcus) and Pseudomonas are the most commonly isolated bacteria from bacterial keratitis cases (Wang et al, 2008). Bacterial toxins and proteinases, as well as host inflammatory mediators, proteinases and toxins can cause rapid stromal loss (keratomalacia) (Ollivier et al, 2007). Not every ulcer is infected and antibiotic usage in these cases is prophylactic rather than therapeutic.
Topical anti-proteinases such as serum, N-acetyl-cysteine, ethylenediamine tetraacetic acid or tetracyclines should be used in cases with melting corneal ulcers (Ollivier et al, 2007). Serum need not be harvested from the patient, as serum donated from another dog may be preferable to struggling to collect it from a brachycephalic patient with a fragile eye and respiratory compromise. Intensive frequent application of topical medications, potentially with hospitalisation, is indicated for cases of corneal melting (Figure 16). Ocular lubricants should also be used.
Analgesia should be provided (such as systemic non-steroidal anti-inflammatories). Cycloplegic drugs should be used if there is miosis caused by reflex uveitis. Ongoing use of topical atropine can reduce tear production and cyclopentolate may be a preferable drug (Costa et al, 2016). Topical non-steroidal anti-inflammatories, steroids and the use of local anaesthetics for non-diagnostic purposes should all be avoided in cases of corneal ulceration.
Corneal cross-linking, a relatively new technique finding use in veterinary ophthalmology, may be increasingly used in the management of stromal corneal ulcerations. The procedure can sterilise the cornea as well as cross-link the corneal collagen, providing strength (Pot et al, 2014).
Superficial epithelial ulcers in brachycephalic breeds need to be treated with care, to avoid corneal melting. Addressing any causative eyelid and tear film issue is the key to successful treatment. Keratotomy (including diamond burr debridement) procedures should generally be avoided.
Surgical management
Corneal ulcers deeper than 50% corneal depth usually need a corneal grafting procedure, for example a conjunctival graft, corneo-conjunctival transposition, collagen (Dorbandt et al, 2015) or amnion graft (Costa et al, 2019). Both partial thickness (lamellar) and full thickness (penetrating) keratoplasties (corneal transplants) can be performed (Lacerda et al, 2017). Following corneal grafting procedures scarring, corneal pigmentation and the graft itself may reduce corneal clarity, especially in pugs (Cebrian et al, 2021). Enucleation may have to be considered in cases where repair is not possible or where corneal repair would be complex, with a poor visual potential such as a perforated eye with no dazzle reflex or consensual pupillary light reflex to the contralateral eye.
Surgical options for the removal of corneal pigmentation including corneal cryo-surgery (Azoulay, 2014), diamond burr debridement (Gradilone et al, 2012) and superficial keratectomy (Gilger et al, 2007) have been described. Recurrence of pigmentation is likely and any surgically induced ulcerations must be appropriately managed.
Conclusions
Eyelid and skull conformation, tear film deficiencies, poor corneal sensation, incomplete and inefficient blinking and aggravating factors such as distichiasis contribute to the ocular surface problems commonly seen in small brachycephalic dogs. Globe proptosis is also more likely in small brachycephalic breeds. Successful management of BOS requires correction of the underlying causes by both surgical and medical means. Medial canthoplasty is the primary surgical option for the correction of the eyelid abnormalities associated with BOS, with or without additional procedures such as a Hotz-Celsus procedure or nasal fold resection. Appropriate management of any associated corneal disease is also required. In dogs with signs of poor corneal health and developing pigment, there is an argument for early intervention to try to prevent more serious ocular surface disease occurring.
KEY POINTS:
- The term brachycephalic ocular syndrome is commonly used to describe the eye problems associated with small brachycephalic breeds. Their conformation, tear film deficiencies and abnormal eyelashes (distichiasis and ectopic cilia) contribute to this syndrome.
- Corneal ulceration, corneal pigmentation and globe proptosis are commonly associated with brachycephalic ocular syndrome.
- Medial canthoplasty with ongoing tear film support is the main treatment of brachycephalic ocular syndrome. Abnormal eyelashes should be removed if deemed significant.
- Corneal ulceration in the small brachycephalic breeds can rapidly deteriorate and prompt aggressive medical management is required, or surgical repair if the ulcer is deep. Management of the eyelid conformation, poor tear film and abnormal eyelashes should not be neglected.


