Quality improvement is a popular theme in veterinary practice – but what does it really mean? What do practices actually need to do to achieve it? Batalden and Davidoff (2007) defined quality improvement as ‘the combined and unceasing efforts of everyone to make the changes that will lead to better patient outcomes (health), better system performance (care) and better professional development (learning)’. This definition is important as it emphasises both the continuous nature of quality improvement and the fact that, in order to work, it must involve the whole team.
Constantly reviewing the way care is delivered to patients and clients, what outcomes are obtained and learning from everything have always been the main drivers of veterinary practice. Quality improvement formalises these activities so that it is a well-thought out, continuous process. In the UK, all veterinary professionals who are regulated by the Royal College of Veterinary Surgeons (RCVS) are expected to ensure that clinical governance forms part of their professional activities (RCVS, 2024).
Following issues around inadequate care in human healthcare, Scally and Donaldson (1998) defined clinical governance as a framework through which organisations are accountable for continually improving the quality of their services and safeguarding high standards of clinical care by creating an environment where excellence in clinical care will flourish. ‘Clinical governance’ includes most of the important areas of running a practice – risk management, practice and team management, the client and patient experience, information, training and continuous professional development, clinical effectiveness and clinical audit.
Clinical effectiveness is a measure of how well a particular procedure achieves the desired outcome. It is where evidence-based medicine (doing the right things) and quality improvement (doing things properly) intersect. Clinical governance determines what veterinarians must do, whereas quality improvement is a systematic approach that uses tools to identify gaps, analyse data and make and test changes leading to continuous improvement.
The definition of quality
The second article in this series will discuss quality improvement tools. First, it is important to discuss what is meant by quality. The domains of quality in human healthcare have been adapted by RCVS Knowledge to fit the veterinary scenario (Figure 1). They consist of care that is:

Any quality improvement projects undertaken should aim to improve at least one of these domains of quality. When focusing on one area to improve, it is important to carefully balance the other domains – for example, using disposable drapes to improve efficiency may have a negative impact on sustainability (Vasanthakumar, 2021).
Getting the team on board
Keeping these principles at the heart of quality improvement can reassure all persons involved that the aim is to systematically improve care and outcomes and develop practice teams. There is no one set way to achieve quality improvement – for most practices, it will consist of a mixture of methods. For all practices, the first step is getting the team on board.
This will involve education on the principles of quality improvement and methods for the whole team. RCVS Knowledge has many useful resources for this part of the process, delivering the quality improvement message in many different formats to suit all learners. A mixture of articles, webinars and podcasts can be found in RVCS Knowledge's (2024a) quality improvement boxset. Once the whole team understands what quality improvement is, the next step is to think about the aims of quality improvement for that particular practice.
Determining where a practice needs improvement
It is vital that the whole team is able to discuss which areas will be considered. Encouraging the whole team to suggest small areas that might need improvement is a great first step. The team members who are working day-to-day will know what their personal areas of concern are. These are the small things that, if improved, would make a big difference; for example, moving a computer terminal to an easier-to-access location.
Once an area of practice which needs improvement, be it one small process (eg putting a cost estimate on client consent forms) or one whole area (eg patient safety in anaesthesia), has been identified, the first step is to measure what the current situation is and whether a perceived issue is an actual problem.
Once the current situation has been established, the team (or a subgroup of the team) need to decide if improvement is needed, exactly what improvement they want to see and by when. Aims should be SMART (Specific, Measureable, Attainable, Relevant and Timely). Once an aim has been decided, the team can share ideas to think about what changes can be made to make an improvement.
An improvement in one area might cause an issue in another area. Pronovost et al (2015) stated that ‘healthcare is a system of systems, and perturbing one element of the system without considering its impact on other elements of the system may result in a breakdown’. Therefore, it is important to consider what balancing measures, if any, may need to be implemented to minimise any problems. For example, if the receptionist who's new duty is checking consent forms for estimates at the end of the day now works in the afternoon to ensure they can liaise with more vets, jobs that may otherwise be performed in the morning may be neglected if not assigned to someone else.
It is important to learn from everything that happens in the practice, whether it is successful treatment, a poor outcome or a near miss. In order to do this, the event should be discussed by the team in a significant event audit meeting (Mosedale, 2017).
Changes made as a result of a quality improvement project may be successful and be adopted by the whole practice. They may need balancing measures, or they may need to be adapted and tested again. In some cases, they will be unsuccessful and will have to be abandoned.
Implementing quality improvement in practice
The next step is to consider how to implement quality improvement in the practice. The main methods a practice might want to consider when starting out in quality improvement are (Box 1):
Elements of a quality improvement framework
Communication
It is vital that the team are not only involved from the start, but that they are also aware of all the quality improvement activities occurring in the practice.
Regular team meetings or specific quality improvement meetings are an important part of the process to ensure everyone is aware of quality improvement projects and are able to contribute. In cases where face-to-face meetings are difficult, regular email updates to the team can be useful.
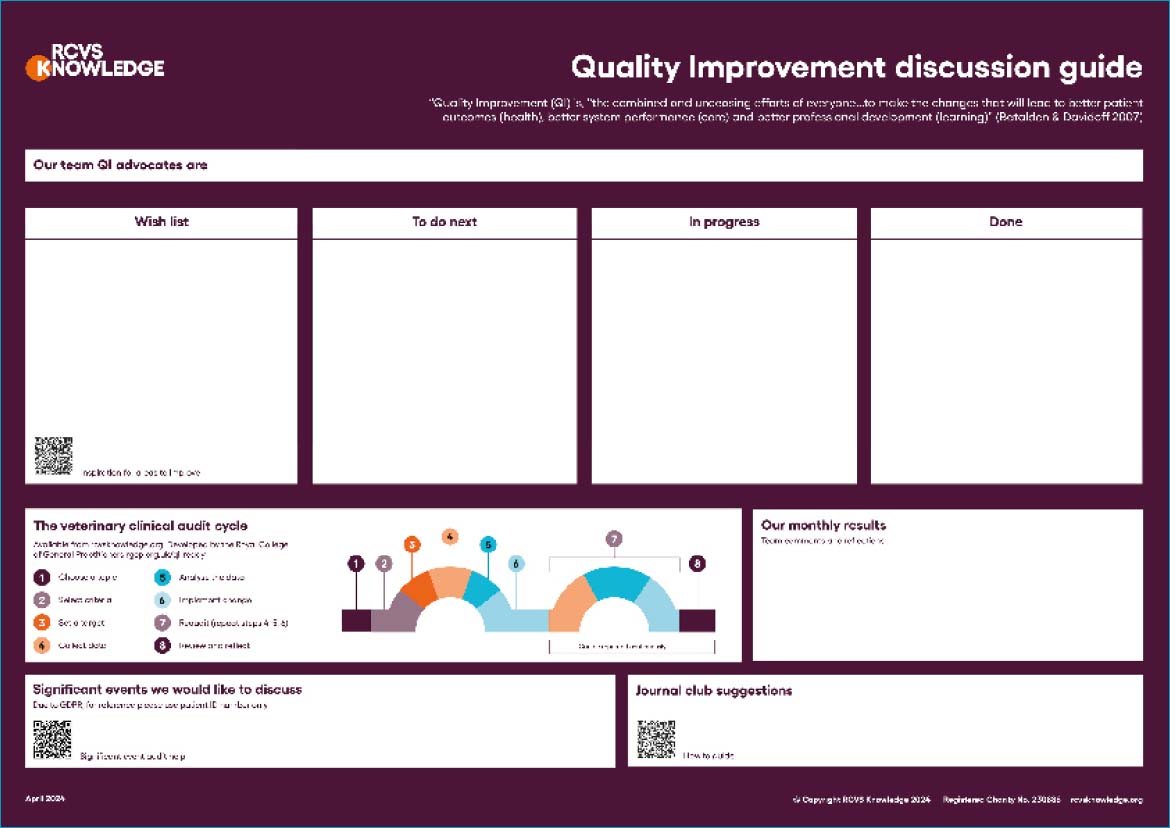
Practice quality improvement notice boards can be particularly useful when there are interim results from ongoing projects to share – for instance, monthly neutering complication figures. RCVS Knowledge have a downloadable poster which can be used to track progress throughout a quality improvement project (Figure 2) (RCVS Knowledge, 2022).
Feeding back information to the team from continuous professional development undertaken or from reports on cases referred to specialists is a great way to share learning. Journal clubs are a useful tool in bridging the gap between research and practice, and embedding evidence-based veterinary medicine into practice. They can stimulate debate between colleagues and can help with establishing practice guidelines. Journal clubs may be face-to-face or online. They may involve the whole team or just certain subject or interest areas. There is help with setting up journal clubs (RCVS Knowledge, 2020) and with critically appraising papers at the RCVS Knowledge evidence-based veterinary medicine toolkit (RCVS Knowledge, 2024b).
Having a structure of when and how meetings, continuous professional development sharing and journal clubs occur is an important basic part of a quality improvement framework.
Another key area of communication to reduce errors and from a patient safety perspective is to use closed-loop communication (Diaz and Dawson, 2020). This is where the person receiving an instruction (eg the amount of a drug to give to a patient) repeats the message back to ensure they have understood it correctly, and the first person confirms whether they are correct, closing the loop.
Communication at the start of the day, eg short huddles or prebriefs, can ensure the whole team is aware of the plans for the day and any potential safety issues. Communication after an error has occurred is also very important. After a serious patient safety incident like an anaesthetic death, stopping for five minutes for a ‘hot debrief ’ (Figure 3) to check that the team are OK and to have a first look at what could be improved, what went well, and any action points can be very useful and can help team members involved in the incident.
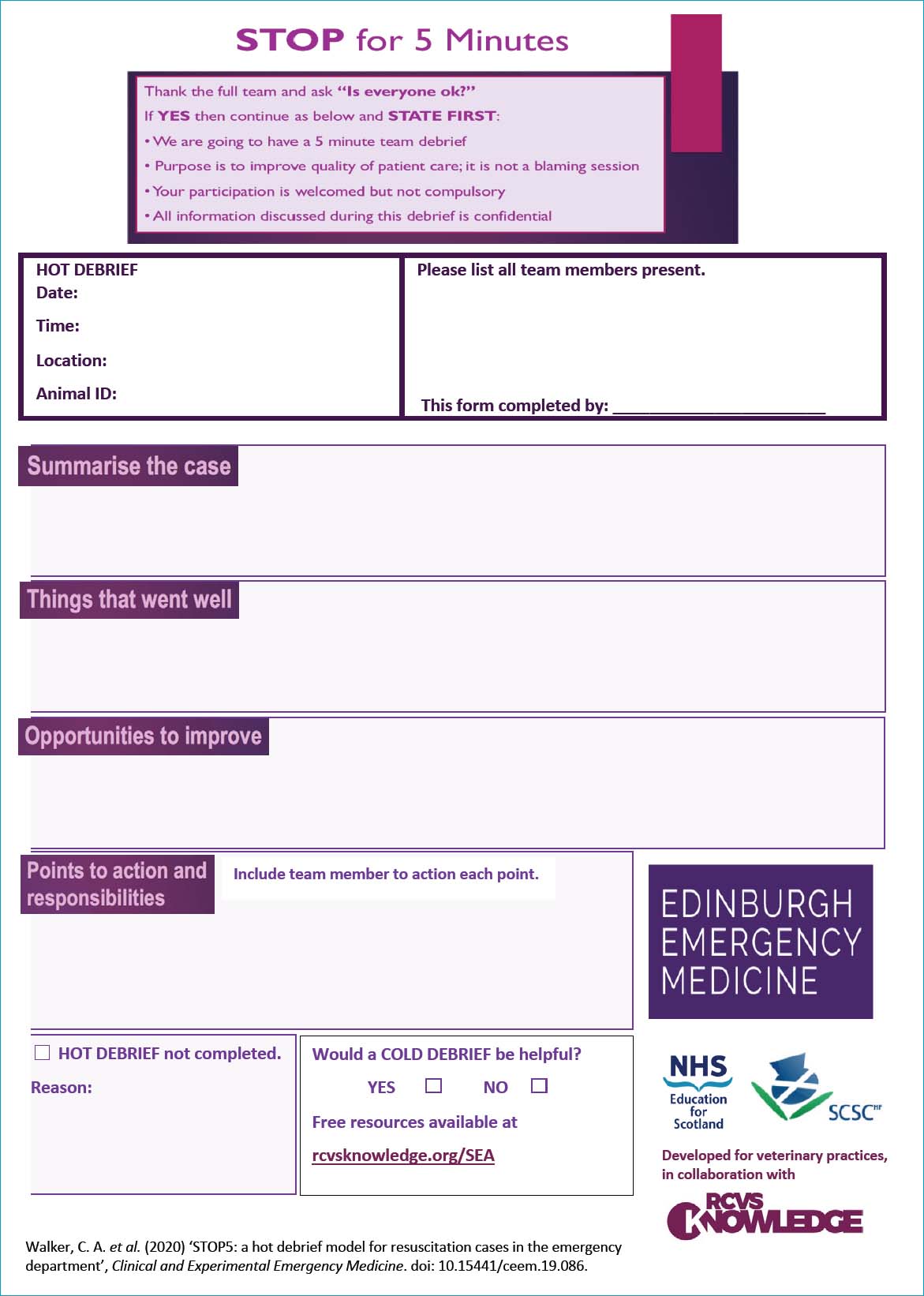
Later, when emotions are not running as high, it is good to have a more in-depth discussion of the incident. This ‘cold debrief ’ might be in a morbidity and mortality meeting for clinical events. Morbidity and mortality meetings are used to improve patient care by developing a culture of awareness of quality and encouraging clinical staff to identify harm, report problems and share lessons to prevent recurrence.
However, it is also useful to discuss less serious and non-clinical events that might affect the running of the practice or the care of patents. These ‘significant event audit’ meetings of the whole team, or at least representatives of all sectors of the practice, are to address systems issues identified, not to blame individuals.
While errors and near misses will commonly be discussed in significant event audit meetings, it is also valuable to discuss situations that have gone well. Procedures normally go well, and learning can be missed by just focusing on things that go wrong. This change in focus from safety I (looking at things that go wrong) to safety II (looking at things that go well) was introduced by Hollnagel et al (2015). At the significant event audit meetings, root cause analysis tools can be used to look for all the factors involved in an error. These tools will be discussed in more detail in the second part of this article.
Culture and quality improvement
It is vital for patient safety to be part of the practice's culture, where team members are listened to, errors are treated as learning opportunities and team members can speak up if they see a potential error. Encouraging the team to use a tool to express concerns can be a useful way to ensure that this happens. Probe, Alert, Challenge, Escalate (PACE) is one such model which leads a team member through a series of graded assertiveness questions and statements to express their concerns.
Culture can be defined as the ‘the way we do things round here’ (Braithwaite et al, 2017) and quality improvement can be seen as an effective methodology for improving practice culture and producing the right conditions for a happier, safer and more productive work environment (Mosedale and Turner, 2022).
Conclusions
Once the culture is in place and the whole practice understands quality and safety, have developed a united purpose and clear aims, and are communicating effectively, it is time to familiarise the team with different quality improvement methods and tools to see which will work best in each individual practice. Part 2 of this article series will discuss using quality improvement methods and tools, considering human factors and systems thinking, and the importance of learning from everything that happens in the practice.


