The main objective when treating vertebral fractures and luxations is to provide an environment in which damaged neural tissues can recover their optimal function (Jeffery, 2010). Pharmacological and non-pharmacological therapies address primary injury in spinal cord damage and minimise the effects of secondary injury. The timing and efficacy of treatment of primary and secondary injury significantly affect the prognosis of a neurotrauma patient (DiFazio and Fletcher, 2013).
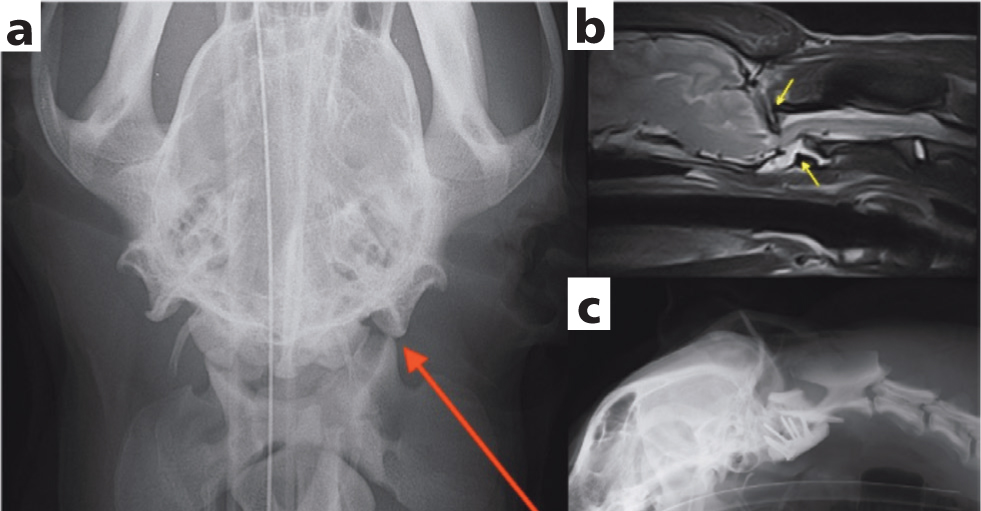
The critical factors in determining whether conservative or surgical therapy is the most appropriate hinges on the spinal cord compression and spinal ‘instability’. This is based on a three-compartment model (Figure 12 in Vertebral fractions and luxations part 1: diagnosis and prognosis, 10.12968/coan.2020.0027), whereby if two or more of the compartments (dorsal, middle or ventral) are affected (including ligaments), the column is considered unstable and requires stabilisation (Figure 1) (Jeffery, 2010). The three compartments consist of:
Dorsal compartment
- Articular processes
- Lateral pedicles
- Dorsal laminae
- Interarcuate ligaments
- Dorsal spinous processes
Middle compartment
- Dorsal ¼ of the vertebral body and disc
- Dorsal longitudinal ligament
Ventral compartment
- Ventral ¾ of the vertebral body and disc
- Ventral longitudinal ligament.
Decompression and vertebral stabilisation remain the therapeutic options of choice for the primary spinal cord injury caused by unstable and/or compressive vertebral fracture or luxation (Olby, 2010). The treatment for secondary injuries, such as spinal cord ischaemia, is to maintain blood pressure and oxygenation, in order to maintain spinal cord perfusion (Olby, 2010).
Conservative management and steroids
Minimal neurological deficits, medically manageable spinal pain and lack of spinal instability in cases of vertebral fractures and luxations usually do not require surgical intervention and can be occasionally treated conservatively with cage rest (4–6 weeks) and pain management (Hawthorne et al, 1999; Bagley, 2000; Schmidli et al, 2019). However, precise assessment of the injury via advanced imaging needs to be performed (Selcer et al, 1991; Jeffery, 2010; Schmidli et al, 2019).
High-dose methylprednisolone sodium succinate (Kube and Olby, 2008; Olby et al, 2016), which is the therapy of choice for free radical-induced injury and an established treatment for acute spinal cord injuries in human medicine, is falling out of favour because studies have shown little therapeutic benefit and severe adverse effects (Kube and Olby, 2008; Olby et al, 2016, Fehlings et al, 2017). This is the same for any steroid use in general. The evidence of deleterious effects of steroids continues to accumulate (Jeffery, 2010). Other substances tested, including N-acetylcysteine, dimethyl sulfoxide and eta-aminocaproic acid, have also failed to show benefit in dogs (Olby, 2010).
Surgical treatment goals and techniques
Decompression and appropriate stabilisation of the vertebral column are the main objective of surgical vertebral fracture and luxation management, as this allows spinal cord and fracture healing, and fibrosis of the luxations (Olby et al, 2003; Jeffery, 2010).
Compression of the spinal cord in cases of vertebral fractures can be caused by haematoma, traumatic disc extrusion or by displaced bone fragments (Jeffery, 2010; Olby, 1999, 2010). Those compressive lesions are, similarly to more common causes of spinal cord compression (such as intervertebral disc extrusions), addressed by decompressive surgical procedures, such as ventral slot or laminectomy, hemilaminectomy or mini-hemilaminectomy (Olby, 1999; Olby et al, 2003). Sparing the intact articular facets and avoiding further destabilisation are the caveats of decompressions in vertebral fracture and luxation cases (Walter et al, 1986; Jaumard et al, 2011).
The nature of the spinal cord compression, the extent of the injury and the case-specific landmarks are given by diagnostic imaging (ideally computed tomography), which helps with the surgical planning as well (Selcer et al, 1991; Hettlich et al, 2010; Gallastegui et al, 2019). Surgical planning and surgery itself prevent further damage to the spinal cord and provide an adequate environment for healing (Selcer et al, 1991; Shores, 1992; Olby, 1999; 2010). The main considerations in vertebral fracture stabilisation are localisation, determining the surgical approach (usually a ventral approach in cervical and a dorsal approach in thoracolumbar injuries), the nature of the fracture (for example, displaced fragments requiring reduction) and selection of the implants in terms of the necessary type, number, placement (unilateral or bilateral), insertion angles, maximum bone purchase and implant corridor. Consideration of all these factors will result in an individually tailored surgical plan for the patient. The extent of the implantation depends on the type of injury (luxation or fracture) and degree of instability (Blass and Seim, 1984; Selcer et al, 1991; Bruce et al, 2008; Krauss et al, 2012; Schmidli et al, 2019). For an inherently stable fracture or luxation one adjacent vertebra, cranially and caudally, may be sufficient. In cases of unstable fracture or luxation, it might be necessary to include two vertebrae from each side (Selcer et al, 1991; Jeffery, 2010). Detailed description of all available techniques is beyond the scope of this review, but this article provides a general overview.
For cervical, thoracolumbar and lumbosacral injuries composite fixation with monocortical screws or bicortical pins and polymethylmethacrylate (Blass and Seim, 1984; Garcia et al, 1994; Dewey et al, 2013), or adequate plating techniques, (Shores, 1992; Sturges et al, 2016) are the most common. For thoracolumbar spine stabilisations external skeletal fixation, spinal stapling or LUBRA plating technique had been described (Walker et al, 2002; Lanz et al, 2003; Voss and Montavon, 2004; Wheeler et al, 2007; Krauss et al, 2012), but clinical evidence of effectiveness and possible complications (such as implant infection in cases of external skeletal fixation, or implant loosening) for those techniques is sparse.
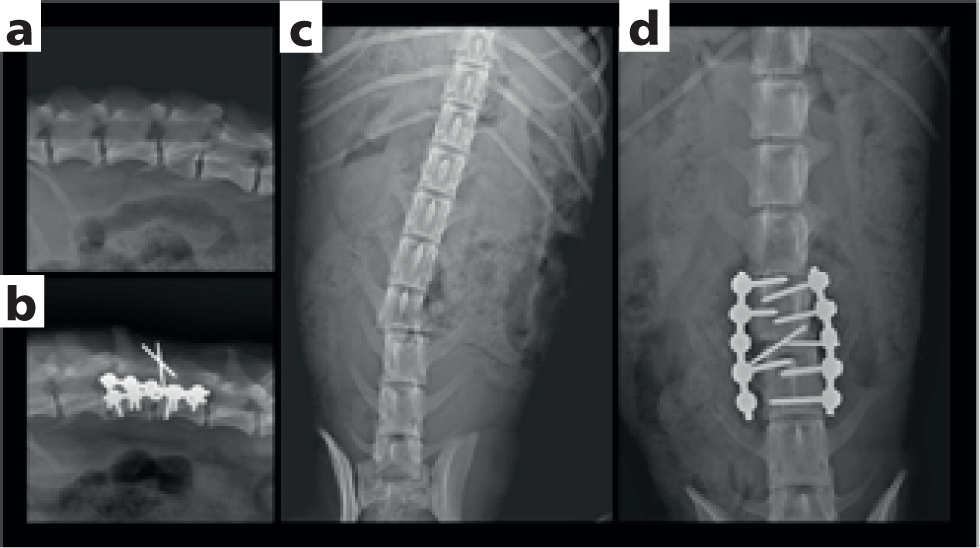
Screw and polymethylmethacrylate stabilisation (Figure 2) involves screws being placed to the bone near the vertebral endplates, to obtain the best bone purchase. Two to four screws can be placed into each vertebral body, as necessary, depending on the size of the bone and the degree of instability (Garcia et al, 1994). Polymethylmethacrylate pin constructs (Figures 2 and 3) give greater insertion freedom in areas of challenging anatomy, such as the cranial thoracic spine where rib heads obscure part of the lamina (Blass and Seim, 1984). Protrusion from the bone should be approximately 10–15 mm in screws and 15–20 mm in pins, to sufficiently incorporate to the polymethylmethacrylate bone cement which should be at least 1–1.5 cm thick (Garcia et al, 1994). An excessive amount of cement may be detrimental, especially in the cervical spine stabilisations, as it may cause a pressure to the oesophagus or trachea, resulting in swallowing difficulties and hypoventilation respectively, among other potential risks (Hawthorne et al, 1999; Beal et al, 2001).

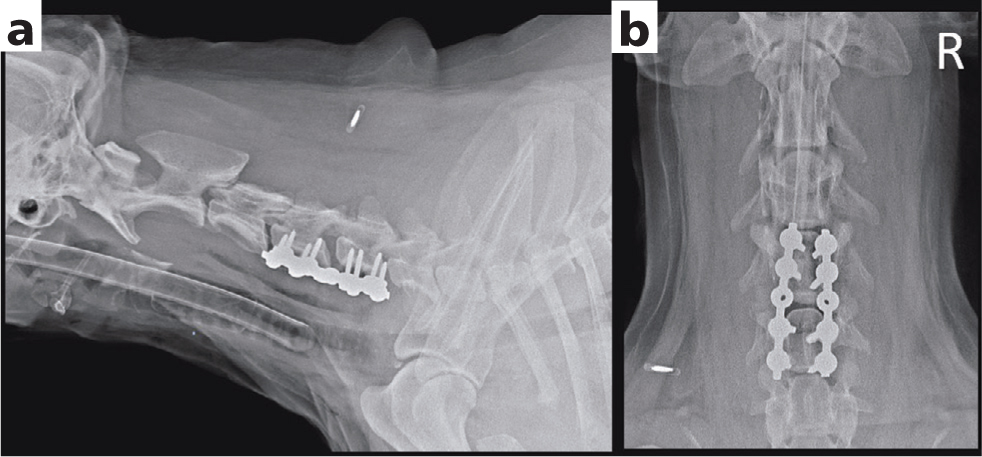
Plates in vertebral fracture and luxation cases can be placed in vertebral body or dorsal spinal processes. Commonly used plates are locking plates, such as locking compression plates (Sturges et al, 2016) or string-of-pearls plates (Nel et al, 2017) (Figures 1 and 4). Implant profile is much decreased, compared to the screw/pin and polymethylmethacrylate fixation, which can be beneficial in areas with a lack of muscle, subcutaneous and cutaneous tissues, or where extensive implants can cause undesirable compression of the important surrounding structures, for example the trachea, oesophagus or major vessels and nerves in cervical region (Figure 4). The advantage of the locking plating system is based on tight bone plate contact not being necessary, compared to the now obsolete traditional plates, meaning that the straight plate can be placed over the uneven vertebral column surface (Sturges et al, 2016). Both locking plate types have fixed screw trajectory to ensure proper engagement of the locking mechanism (Walter et al, 1986; Sturges et al, 2016; Nel et al, 2017). Presurgical plating planning prevents inadvertent screw placement to the intervertebral disc space or to the vertebral canal. Locking compression plates, as well as string-of-pearls plates, can be contoured to adjust to the fixed area. However, the least possible amount of contouring is advised to engage the locking mechanism. If required, two parallel or bilateral plates can be placed.
External skeletal fixation or Kirschner–Ehmer apparatus can be considered in cases of thoracolumbar injuries, where rapid and uncomplicated recovery is expected, such as vertebral luxation in a juvenile animal (Walker et al, 2002; Lanz et al, 2003; Grasmueck and Steffen, 2004; Wheeler et al, 2007), or in cases of pathological fractures resulting from osteomyelitis (Arzi et al, 2010; Brocal et al, 2019). Closed, bilateral pin application (typically one pin per vertebra), with fluoroscopic guidance, may lead to better bone purchase and reduced injury to paravertebral muscles and vasculature, compared to the open approach (Wheeler et al, 2007). The advantage of external skeletal fixation hinges on the ability to remove implants without a second large surgery. However, an increased risk of infection needs to be carefully considered (Egger, 1991; Beever et al, 2017). External skeletal fixation requires excellent owner compliance because of the daily care needed around the implant. This may put limitations on postoperative rehabilitation.
Spinal stapling stabilisation and Lubra plating are techniques that use the dorsal spinal process in the fixation apparatus (Voss and Montavon, 2004; Krauss et al, 2012). In spinal stapling a K wire or Steinmann pin contour around dorsal spinal processes, act as an internal splint. Fixation of the pins is achieved by drilling small holes through the base of the spinous processes and tightening the pin with cerclage wire (Voss and Montavon, 2004; Krauss et al, 2012).
Outcomes of surgical management
With surgical treatment and intact nociception, good outcomes have been reported in 80-90% of patients with fractured or luxated vertebrae (Blass and Seim, 1984; Selcer et al, 1991; Krauss et al, 2012; Schmidli et al, 2019). However, fractures of the cervical vertebral column may be associated with an increased risk of perioperative mortality (Beal et al, 2001; Schmidli et al, 2019). In a study by Hawthorne et al (1999) the perioperative mortality rate reached 36%, whereas in a more recent study by Schmidli et al (2019), of axis only fractures, mortality connected to the surgery was lower (up to 10%). Despite the time spent in hospital being twice as long in the surgically treated group, the time for optimal neurological improvement was longer for medically treated animals in the Selcer et al (1991) study.
The timing of decompression has been contentious, but a critical meta-analysis of preclinical studies, human clinical trials and also veterinary studies of mainly intervertebral disc herniations, has concluded that prompt decompression improves outcome and is associated with improved survival rates (Hawthorne et al, 1999; Furlan et al, 2011). Nevertheless, it is critical when translating this finding to cases of vertebral fractures and luxations, to carefully consider the risks to life, as well as the risk of inducing a damaging reduction in blood pressure (which can worsen neural injuries) incurred through too hasty induction of anaesthesia (Jeffery 2010; DiFazio and Fletcher, 2013; Fehlings et al, 2017).
Surgical timing seems to influence the occurrence of progressive myelomalacia in dogs, especially when surgery is performed more than 12 hours after the loss of ambulation in cases of intervertebral disc extrusion. In the same study, treatment with corticosteroids was associated with an increased risk of progressive myelomalacia (Castel et al, 2017).
Main complications of surgery
Iatrogenic injury to the spinal cord, nerve roots, vascular supply or intervertebral disc are the main potential complications to consider while performing surgery (Bruce et al, 2008; Jeffery, 2010). Implant related complications include implant loosening and failure, as a result of inappropriate implant size or placement, poor bone holding properties or excess patient mobility (Blass and Seim, 1984; Selcer et al, 1991; Krauss et al, 2012). Infection of the surgical site also needs to be considered. While this is less likely to be caused by implant contamination, it can occur from a haematogenous spread of bacteria (Cabassu and Moissonnier, 2007). Appropriate use perioperative antimicrobials decrease the risk of contamination from the skin. Courses of therapeutic antimicrobials after a clean surgery are controversial (Shaffer et al, 2013). However, in cases of vertebral fractures and luxations, any lacerations or open wounds can justify the use of antibiotics. Samples for bacterial culture and sensitivity should be routinely taken before commencing the antimicrobial treatment.
In spite of meticulous dead space closure, seroma formation might still occur. Warm compresses and the passage of time are sufficient in the most cases. Repeated aspiration of seromas should be avoided because of the possibility of iatrogenic contamination (Selcer et al, 1991). Figure 4 details an example of inappropriate seroma management by a referring veterinary surgeon.
Required supportive care
Supportive care of an animal with vertebral fracture or luxation can be very intensive. It involves cautious changing of position every 4 hours, if the patient is recumbent, as well as preventing decubital ulcers (by providing extra padding or using water beds), using non-split mats, assisted feeding and urinary bladder management (Jeffery, 2010).
Urological sequelae to acute spinal cord injury (upper motor neuron or lower motor neuron bladder) pose significant complications, in both human and canine patients, and can impact the quality of life and long-term cost of treatment (Cook et al, 2019).
Disorders of bladder emptying can be managed by manual expression or by intermittent or indwelling catheterisation, although there are potential complications with each method (Jeffery, 2010). Incomplete emptying, which is often a complication of manual expression of ‘upper motor neuron’ bladders (Cook et al, 2019), and non-aseptic catheterisation both carry the risk of urinary tract infections, often associated with duration of bladder dysfunction (Bubenik and Hosgood, 2008). Indiscriminate use of prophylactic antibiotics in animals with indwelling catheters should be avoided (Bubenik et al, 2007).
Conclusions
Unstable and compressive vertebral fractures and luxations in dogs and cats require spinal stabilisation and decompression respectively. So far, no pharmacological strategies had been proven to be beneficial in such patients. Precise planning should proceed stabilisation surgeries and timing depends on safety of anaesthesia. Vertebral fracture or luxation dogs and cats with intact nociception generally have good outcomes after spinal surgeries. The main complications of the spinal stabilisations are neurological deterioration, implant loosening or failure, and infection. Urinary bladder management is of paramount importance as urological consequences to acute spinal cord injury pose significant complications to animals with fractured or luxated vertebrae.
KEY POINTS
- The aim of treatment for vertebral fractures and luxations is to prevent further damage to the spinal cord and provide an adequate environment for healing.
- Vertebral column instability is an indicator for stabilisation surgery.
- Surgical planning is necessary to evaluate surgical technique, as well as the selection of an appropriate implant type and size.
- Timing of surgery is dependant on the anaesthetic risk.


