There are three types of hypertension, or high blood pressure, in cats: primary (idiopathic), secondary and situational (previously referred to as ‘white coat’ hypertension). Secondary hypertension, which develops in association with an underlying disease process or because of a medication or toxin, is the most common type of hypertension in cats (Taylor et al, 2017; Acierno et al, 2018). The conditions typically associated with hypertension occur with increasing prevalence in older cats; therefore, the prevalence of secondary hypertension also increases with advancing age (Bijsmans et al, 2015; Conroy et al, 2018). The most common cause of hypertension in cats is chronic kidney disease (Maggio et al, 2000; Elliott et al, 2001; Sansom et al, 2004; Conroy et al, 2018). Other conditions associated with high rates of hypertension include hyperthyroidism (Elliott et al, 2001; Conroy et al, 2018), acute kidney injury (Cole et al, 2017) and hyperaldosteronism (although this condition is uncommon). Pheochromocytoma and Cushing's syndrome (Henry et al, 1993; Valentin et al, 2014) can also cause hypertension, but both are rare in this species. Cats with diabetes mellitus can be documented to have concurrent hypertension, but it is not clear that it occurs with a higher frequency than in the general cat population (Al-Ghazlat et al, 2011). Documentation of any of these conditions should prompt blood pressure measurement; details on performing these measurements and when to do so are covered elsewhere (Caney, 2021).
Systemic hypertension is usually diagnosed based on the measurement of systolic blood pressure. If a high definition oscillometric machine is used for blood pressure measurement, then diastolic and mean arterial blood pressure values will also be obtained. Doppler machines are more commonly used in primary care and referral practice (Figure 1), which only provide measurement of systolic blood pressure, but this measurement is considered to be most reliable in cats. As systolic blood pressure rises, the risk of target organ damage increases. Target organs are typically those with a rich arteriolar supply, including the eyes, brain, heart and kidneys. Although the exact point at which systolic blood pressure is high enough to cause damage to these organs will vary between individuals, chronic sustained elevations in systolic blood pressure, typically above 170–180mmHg, put cats at high risk for such damage occurring (Maggio et al, 2000; Mathur et al, 2002; Sansom et al, 2004). The classification system for interpretating feline blood pressure provided by the American College of Veterinary Internal Medicine therefore has four categories of systolic blood pressure measurement, detailing the risk of target organ damage (Table 1) (Acierno et al, 2018).
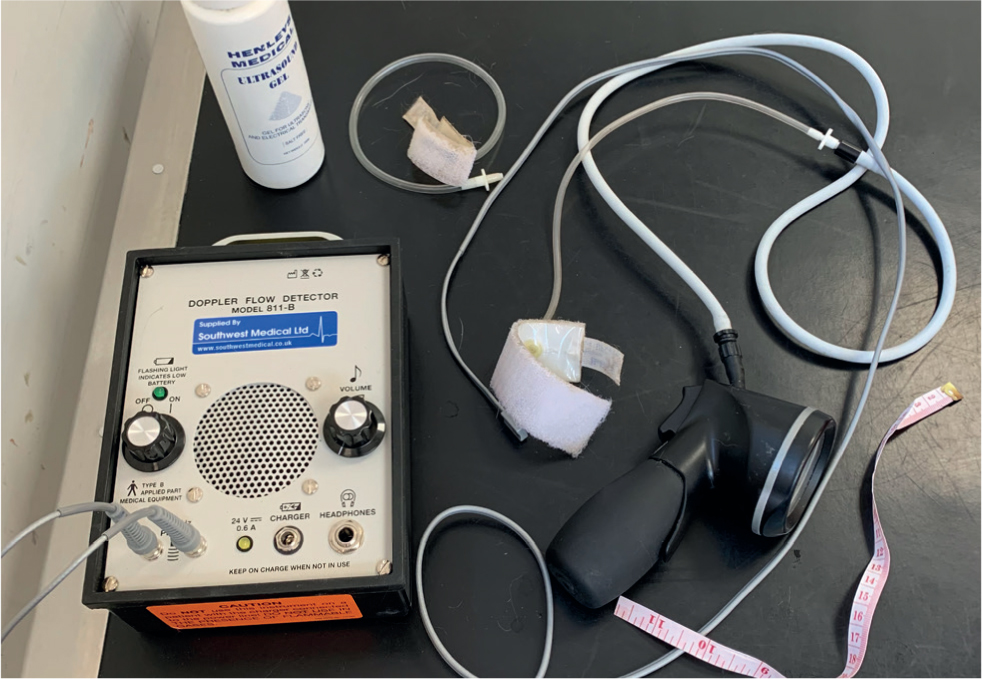
Table 1. The categories for systolic blood pressure interpretation in cats and dogs as outlined by the American College of Veterinary Internal Medicine consensus statement
| Category | Systolic blood pressure (mmHg) | Risk of target organ damage |
|---|---|---|
| Normotensive | 140 | Minimal |
| Prehypertensive | 140–159 | Low |
| Hypertensive | 160–179 | Moderate |
| Severely hypertensive | >180 | High |
When to instigate treatment
The aim of treatment is to reverse or ideally prevent target organ damage from occurring, therefore treatment of cats with moderate to high risk of target organ damage is recommended. Clinicians may worry that documentation of systolic blood pressure >160mmHg might be a result of situational hypertension, especially in a stressed cat. The following steps can be considered to aid in differentiating between situational and true hypertension:
- Allow the cat a short period of time to acclimatise in the clinic before blood pressure measurement (Figure 2)
- Make blood pressure measurement as calm as possible by performing it in a quiet room, ideally with the owner present.
- Obtain five similar consecutive readings and take an average of these. If average systolic blood pressure >160mmHg, perform a fundic examination to check for evidence of target organ damage.
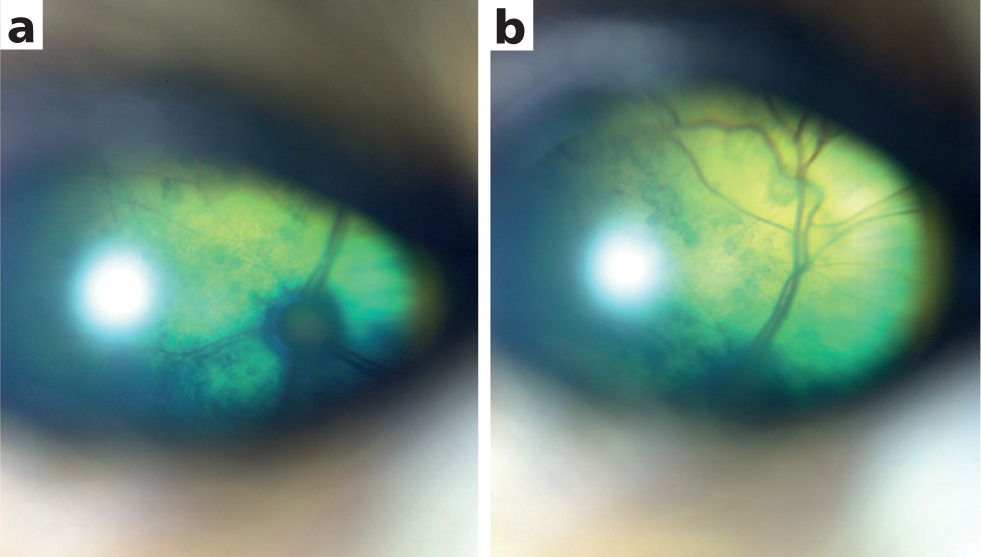
- Treatment should be initiated in all cats with evidence of ocular target organ damage (Figure 3a and 3b) (Carter, 2018)
- If there is no evidence of ocular target organ damage, recheck systolic blood pressure on another day, ideally within the next 2 weeks. Start treatment if average systolic blood pressure is still >160mmHg.

The prevalence of secondary hypertension in association with its common underlying conditions means that the likelihood of a cat having true hypertension, rather than situational hypertension, is high. Therefore, it is reasonable to err on the side of caution and initiate treatment in all cats suspected of secondary hypertension with repeatable systolic blood pressure measurements >160mmHg. If a cat is occasionally experiencing situational hypertension, the risk of hypotension with treatment is low and is likely to be outweighed by the benefit of preventing target organ damage in all cases with definitive secondary hypertension.
Treatment options
In the UK, there are two licensed medications for the treatment of feline hypertension: amlodipine and telmisartan. One of these medications should be selected as the first-line treatment for each individual case. A summary of both medications is shown in Table 2.
Table 2. A summary of dosing and monitoring information for the licenced medications available to treat feline hypertension in the UK
| Amlodipine | Telmisartan | |
|---|---|---|
| Licenced formulation | Amodip® 1.25mg chewable tablets for cats (Ceva Animal Health Ltd) | Semintra 10mg/kg oral solution for cats (Boehringer Ingelheim Animal Health UK Ltd) |
| Recommended starting dose | 0.125–0.25mg/kg/dayDose asCats 2.5–5.0kg: half a tablet every 24 hoursCats 5.1–10kg: one tablet every 24 hours | 2mg/kg every 24 hours |
| Recommended monitoring | After 14 days the dose may be doubled or increased up to 0.5mg/kg every 24 hours if systolic blood pressure response is not yet adequate | Reduce dose if needed after 4 weeks in 0.5mg/kg increments to target systolic blood pressure 120–140mmHg |
| Warning for clients | Pregnant women should avoid contact with angiotensin II receptor blockers. |
Amlodipine
Amlodipine is a calcium channel antagonist, acting on the long-acting type (L-type) calcium channels that are mostly found in vascular smooth muscle. Administration of amlodipine blocks activation of these channels with action potentials and therefore prevents an influx of calcium needed to cause muscle contraction. Its action is therefore greater in more severely hypertensive patients where the vascular smooth muscle is more constricted. Amlodipine was used for many years to treat feline hypertension before a cat-specific licensed formulation was produced, and numerous studies have found that a reduction in systolic blood pressure of 30–60mmHg can be expected (Maggio et al, 2000; Elliott et al, 2001; Snyder et al, 2001; Mathur et al, 2002). Additionally, studies have demonstrated the utility of amlodipine to successfully treat target organ damage, such as the reversal of blindness in cats with hypertension-induced retinal detachment (Maggio et al, 2000), cessation of seizures in cats with hypertensive encephalopathy (Kwiatkowska et al, 2019) and reduction of urine protein:creatinine ratio (Jepson et al, 2007).
A chewable licensed form of amlodipine (Table 2) was evaluated in a European multicentre prospective, double-blinded, placebo-controlled, parallel group study by Huhtinen et al (2015). Enrolled cats (n =77) had persistent systolic blood pressure ≥165mmHg but <200mmHg, although some cats with systolic blood pressure >200mmHg could be included if the attending veterinarian was happy to do so. Cats with ocular or neurological signs of target organ damage were excluded owing to the placebo-controlled study design. Cats were randomly assigned to take amlodipine 0.125mg/kg orally every 24 hours or a placebo for 28 days, with a dose increase aft er 14 days if required. Subsequently, all cats were treated with amlodipine for up to 3 months. Less than a third of cats had idiopathic hypertension, with the majority having chronic kidney disease or hyperthyroidism. Amlodipine was shown to be successful in treating hypertension, with 63% of cats achieving systolic blood pressure <150mmHg or a reduction in systolic blood pressure of ≥15% by 28 days, compared to 18% of cats receiving a placebo. Adverse effects were uncommon and there was no difference in these between groups. No cats were documented to develop hypotension, despite the fact that 15.6% of the cases were also receiving an angiotensin converting enzyme inhibitor during the study. Palatability for taking the tablet was high, at 80% in the amlodipine group.
Plasma amlodipine concentrations are directly related to the oral dose of amlodipine administered. The dose required by an individual cat to successfully control their hypertension can vary, but cats with a higher systolic blood pressure at diagnosis require a higher amlodipine dose to achieve adequate control of their systolic blood pressure. A study of 100 hypertensive cats treated with amlodipine found that cats with systolic blood pressure >200mmHg were more likely to require a dose of 1.25mg every 24 hours to reduce their systolic blood pressure to <160mmHg, compared to cats with systolic blood pressure <200mmHg, where a dose of 0.625mg every 24 hours was usually sufficient (Bijsmans et al, 2016).
Telmisartan
Telmisartan is an angiotensin II receptor blocker. As part of the renin-angiotensin-aldosterone system, angiotensin II binds to two receptors, AT 1 and AT 2. Activation of the AT 1 receptor is associated with a number of undesirable effects in chronic kidney disease, including vasoconstriction, proteinuria, glomerular hypertrophy, fibrosis and aldosterone release, whereas activation of the AT 2 receptor is associated with potentially beneficial effects in chronic kidney disease, including vasodilation, vascular protection and anti-fibrosis (Ni et al, 2020). As an angiotensin II receptor blocker, telmisartan preferentially blocks the AT 1 receptor. This prevents constriction of the efferent arteriole in the glomerulus, thereby reducing glomerular pressure and proteinuria, and results in a lowering of systemic blood pressure. The renin-angiotensin-aldosterone system is still not completely understood and recent work has shown that there are a number of additional angiotensin peptides whose actions may complement those of angiotensin II at the AT2 receptor, and the concentrations of which can be affected by telmisartan in cats (Huh et al, 2021). However, further work is required to understand the actions of these additional peptides and the full benefits of treatment with telmisartan.
Telmisartan has been shown to effectively lower blood pressure in awake healthy cats with surgically implanted pressure sensing telemetry devices and to prevent changes in systolic blood pressure induced by administration of angiotensin I boluses (Jenkins et al, 2015). The effects of telmisartan administered in this setting were also shown to still be present aft er 24 hours. In contrast, benazepril was less effective and its effects were much more short-lived. For this reason, and based on anecdotal use in the clinic, the use of benazepril for treatment of feline hypertension is no longer recommended.
Telmisartan has also been evaluated in two large prospective randomised, double-blinded, placebo-controlled clinical trials; one performed in the USA by Coleman et al (2019) and one in Europe by Glaus et al (2019). The initial dosing regime was slightly different between the two studies, but otherwise the study design was analogous, with a 28 day placebo-controlled phased followed by an extended phase of telmisartan use. Both studies included over 200 cats with persistent systolic blood pressure of 160–200mmHg and no evidence of ocular target organ damage. In the European study, hypertension was idiopathic in just under 60% of cats and secondary to chronic kidney disease, hyperthyroidism or both these comorbidities in the remaining cats (Glaus et al, 2019). In the American study, hypertension was idiopathic in approximately 30% of cases and secondary to chronic kidney disease, hyperthyroidism or both these comorbidities in the remaining cats (Coleman et al, 2019). Coleman et al (2019) administered telmisartan orally at 1.5mg/kg every 12 hours for 14 days, followed by 2mg/kg every 24 hours for 14 days. Glaus et al (2019) administered telmisartan orally at 2mg/kg every 24 hours for 28 days. Across the two studies, 52–53% cats in the telmisartan groups achieved an systolic blood pressure of <150mmHg or a reduction of ≥15% in systolic blood pressure by 28 days, which was significantly more than in the placebo groups, where 28% of cats achieved the same result. The incidence of serious adverse effects was similar between telmisartan and placebo treated groups, and was therefore likely caused by comorbid conditions in these older cat populations. In one of the studies, multiple days of vomiting occurred more frequently in the cats receiving telmisartan, but did not necessitate cessation of medication (Coleman et al, 2019). Hypotension occurred in 1–2% of cats. A possible concern when initiating treatment with an angiotensin II receptor blocker is the potential for serum creatinine to increase because of a reduction in glomerular filtration rate with the change in glomerular pressures. This should be monitored for, and treatment should never be initiated in dehydrated cats. However, no significant changes in creatinine were seen in the cats in both studies mentioned above.
The use of telmisartan for more severe hypertension and in cats with evidence of target organ damage is less well reported. One case report of a cat with severe systemic idiopathic hypertension, demonstrated successful resolution of systolic blood pressure from 220–230mmHg with 2mg/kg telmisartan following a need to stop amlodipine as a result of the development of gingival hyperplasia, and failure of 0.7mg/kg benazepril every 24 hours to control systolic blood pressure as monotherapy (Desmet and van der Meer, 2017). No studies have reported on the use of telmisartan in cats with ocular target organ damage, although telmisartan at 1mg/kg every 24 hours has been shown to significantly reduce proteinuria in International Renal Interest Society stage 2–4 cats with urine protein:creatinine ratio >0.2 for 18 months (study end point) (Sent et al, 2015).
The placebo effect
One thing to note from these placebo-controlled trials is that there was a placebo effect seen in all three studies, with 18–28% of cats achieving systolic blood pressure <150mmHg or a reduction in systolic blood pressure of ≥15% by 28 days, despite all cats having to demonstrate persistently elevated systolic blood pressure on two separate clinic visits before starting medication. This emphasises two things; first, that cats are likely to acclimatise to repeated blood pressure measurements and that repeated visits to establish the need for antihypertensive medication are advised if no evidence of target organ damage is present. Second, that rates of hypotension are very low with both of these medications, even if administered to cats that may have had reduction in their systolic blood pressure without pharmaceutical intervention.
Does treating hypertension increase survival time?
There is no study demonstrating that treating cats with hypertension extends their survival time, but this is likely owing to the lack of a control population, such as a group of cats that were not treated for their hypertension. Unexpectedly, studies have failed to demonstrate an association between how well controlled systolic blood pressure is and survival time in hypertensive cats (Littman, 1994; Elliott et al, 2001; Syme et al, 2006; Jepson et al, 2007), but the use of antihypertensive treatments in these studies may have masked the effect of hypertension on survival time. Survival is strongly associated with the urine protein:creatinine ratio at diagnosis, and treatment of hypertension significantly reduces urine protein:creatinine ratio (Jepson et al, 2007), emphasising the importance of treating hypertension to prevent target organ damage.
Combining medications
Data from a small number of cats (n=10) receiving amlodipine for hypertension and telmisartan for management of proteinuria suggested that combination therapy is well tolerated (Sent et al, 2015). Anecdotally, compliance in administering medications is likely to decrease with polypharmacy, therefore efforts should be made to use one medication to its full effect before introducing a second medication. In the rare event that a cat's hypertension cannot be controlled with either amlodipine or telmisartan alone, a combination of these medications should be trialled and the cat carefully re-examined to monitor for adverse effects, including increases in serum creatinine and development of hypotension.
Conclusions
Secondary hypertension is common in older cats, especially in cats with chronic kidney disease and/or hyperthyroidism. Both amlodipine and telmisartan are licensed in the UK for treating feline hypertension and both drugs have been evaluated in prospective randomised, placebo-controlled clinical trials in hypertensive cats with systolic blood pressure from 160–200mmHg that did not have evidence of target organ damage. Initial reductions of 20–30mmHg can be expected with either medication and cats should be re-evaluated after 14 days, with dose adjustments made as required. No studies have compared the performance of one drug against the other. At present, there are more data in the literature to support the use of amlodipine when evidence of target organ damage or severe hypertension (systolic blood pressure >200mmHg) is present. It is very uncommon for a cat to require polypharmacy to successfully control hypertension.
KEY POINTS
- The aim of treatment is to manage or ideally prevent hypertensive target organ damage.
- There are two licensed options for treatment of feline hypertension: amlodipine and telmisartan.
- Either amlodipine or telmisartan should be selected as the first-line treatment.
- The need for polypharmacy to management feline hypertension is rare.
- Cats should be re-evaluated after 2 weeks and dose adjustments made as needed.


