Laparoscopic surgery, also commonly referred to as minimally invasive surgery or ‘key-hole’ surgery, has been one of the fastest growing methods of modern surgery. In the last 10 years, it has awakened great interest among veterinarians owing to the reported advantages for patients; including, but not limited to, minimised surgical trauma, real therapeutic safety and faster recovery (Devitt et al, 2005; Culp et al, 2009). The modern age of laparoscopy in human medicine boomed in the late 1980s, although in veterinary medicine, the same paradigm shift to the minimally invasive approach in soft tissue surgery has yet to occur (Wildt and Lawler, 1985). Some evidence exists in veterinary patients to support the hypothesis that approaches like laparoscopy decrease the severity or incidence of surgical morbidities compared to open surgery (Davidson et al, 2004; Hancock et al, 2005). However, in veterinary medicine, the field of laparoscopy is still very much in its infancy, and further evidence-based randomised studies are required (Mayhew, 2011a).
Laparoscopy is the exploration of the interior of the abdominal cavity using an endoscope. Like most endoscopic procedures, it is accompanied by taking a biopsy of the organs explored. The main advantage of laparoscopy over exploratory laparotomy is the reduction of tissue trauma, which translates into a faster, less painful recovery and with less likelihood of complications during the postoperative period (Monnet and Twedt, 2003).
Laparoscopy and thoracoscopy both provide minimally invasive access to the abdominal and thoracic cavities respectively, allowing for the completion of diagnostic and curative procedures (Lansdowne et al, 2012a; b).
The purpose of this review is to present minimally invasive laparoscopic methods of biopsy in small animal practice as an objective, viable, fast, effective and favourable alternative in the diagnosis of abdominal and thoracic processes.
Laparoscopic procedures
From a technical point of view, laparoscopic exploration is especially interesting when clinicians require a direct, real and magnified view of the less accessible abdominal structures; such as exploration of the diaphragm, liver, gallbladder and hepatic portal, stomach, vascular structures of the roof of the abdomen and inguinal region (Tapia-Araya et al, 2015). Likewise, it is an interesting option for the evaluation of abdominal masses and neoplasia when other means of diagnosis, such as ultrasound or radiography, indicate its possible presence and we need a detailed study accompanied, in most cases, by a biopsy (Richter, 2001). It should be highlighted that laparoscopy with biopsy is a very effective and objective diagnostic method in abdominal processes with non-specific symptoms.
Though it should be noted that, despite the many advantages of laparoscopic exploration, obesity or increased abdominal fat tissue, sepsis, the presence of large masses or adhesions, acute abdominal bleeding and any other factor that prevents the correct visualisation of the abdomen can reduce the diagnostic power of the laparoscopic approach, and given such circumstances, may contraindicate its use (Mayhew, 2011b).
Laparoscopic biopsy
Laparoscopy allows clinicians to carry out an exploration of all the organs of the abdominal cavity and the affected tissue in particular; as well as to locate possible adjacent disease processes. The direct view of the abdominal cavity allows the localisation of lesions (Shamir et al, 2019).
There are many modalities available for collection of tissue samples, including laparoscopic and laparoscopic-assisted techniques which offer a minimally invasive approach for collection of biopsy samples from multiple abdominal and thoracic organs (Mayhew, 2009).
Biopsy increases the diagnostic capacity of laparoscopy, where the histopathological study of the biopsy can then provide an accurate diagnosis. The application of laparoscopy for the taking of biopsies gives a series of advantages:
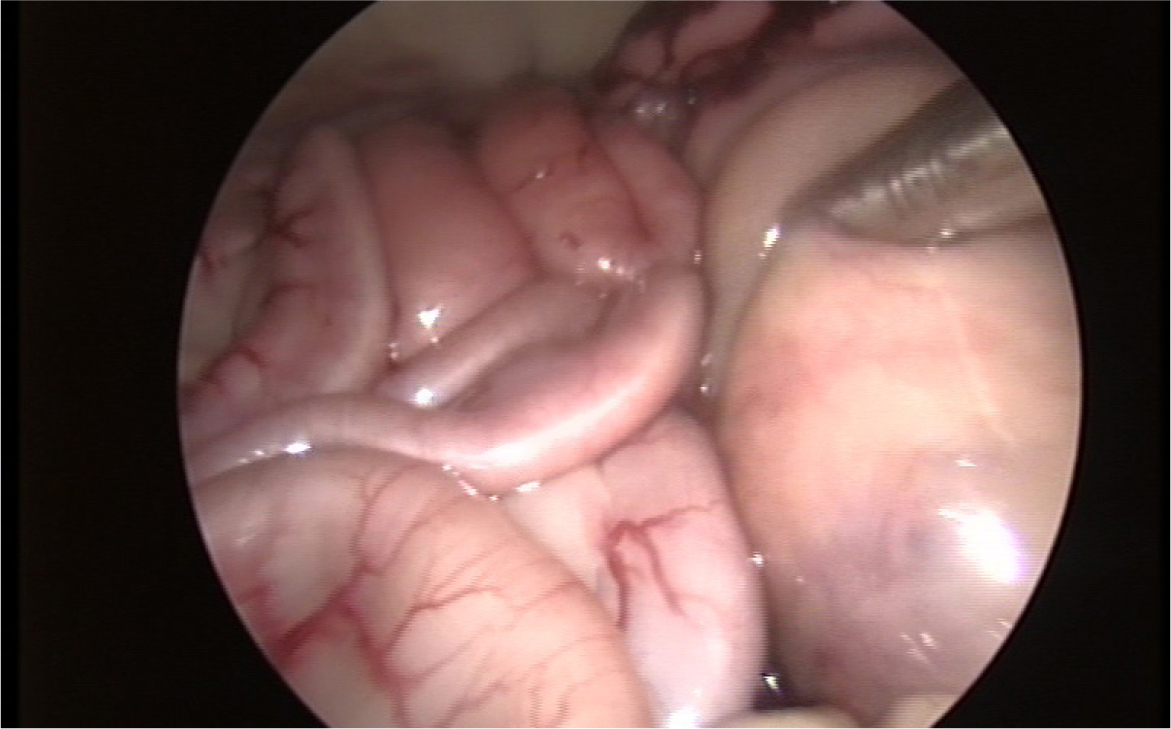
- When using a monitor, sampling is not an individual act, so several experts can evaluate the area to be biopsied at the same time. Laparoscopic images are real and recordable, with the advantage of being less interpretive and viewable a posteriori, both by the owner and by other colleagues, providing added value to the clinical act (Figure 1)
- It is a less aggressive technique than laparotomy, and so it improves postoperative recovery.

Hepatic biopsy:
The main indications for liver biopsy are alterations in liver function, neoplasia, tumour staging and alterations in the biliary tract. There are several techniques described for liver biopsy, but the most widely used are the Tru-cut needle and the fine needle aspiration; both of which are ultrasound-guided (Kemp et al, 2015). These techniques are especially useful when lesions or alterations in the thickness of the scar, that are difficult to identify under direct laparoscopic vision, are observed. However, in the face of abnormal liver tests in the presence of a homogeneous image of the liver, laparoscopic liver biopsy is a good alternative to conventional techniques (Rothuizen and Twedt, 2009).
Its main advantages are:
- The possibility of directing the biopsy towards a specific location or lesion
- The possibility of taking multiple biopsies
- The reduction of surgical complications, such as inadvertent puncture of other abdominal viscera
- Direct visual control of liver bleeding after biopsy.
Another interesting advantage is the size of the biopsy; laparoscopic forceps biopsy offers a larger size, surpassing the Tru-cut® needle biopsy. To increase the diagnostic sensitivity of the procedure, taking 4–8 biopsies is recommended (Fernandez et al, 2017).
Being one of the most common uses of diagnostic laparoscopy in the small animal clinic, a further advantage of needle biopsy with visual control over biopsy using blind techniques is the ability to observe the surface texture, the liver's colour and to select a specific puncture site (Petre et al, 2012).
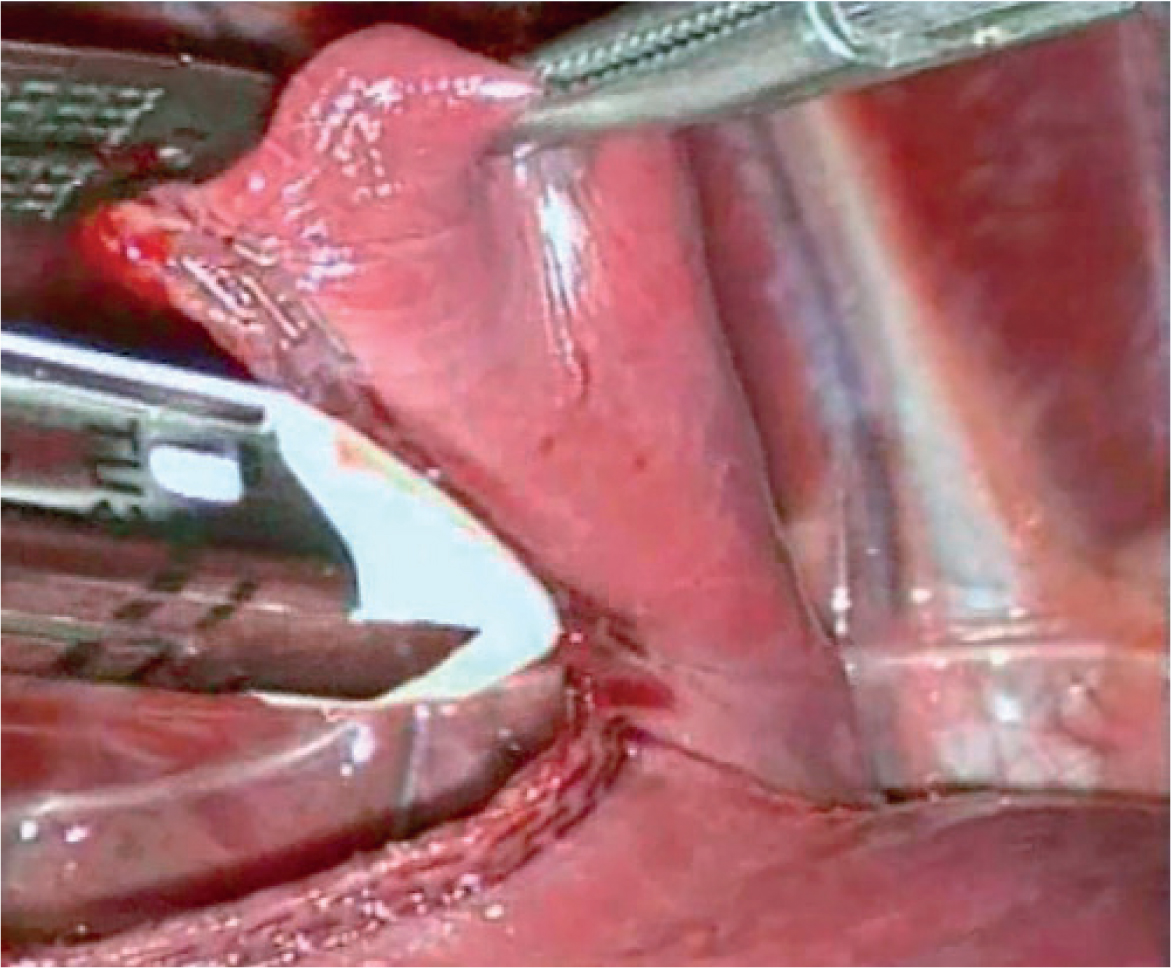
The standard instrument for laparoscopic liver biopsy is 5 mm cup forceps, used in conjunction with monopolar coagulation that may be used if bleeding from the biopsy site exceeds 3 minutes. Diagnostic accuracy of the 3 mm laparoscopic cup biopsy forceps has been described, and despite yielding smaller sample sizes, has a similar level of histologic diagnostic accuracy to the 5 mm instrument (Kimbrell et al, 2018).
Other laparoscopic instruments described are vascular sealants, both advanced bipolar and ultrasonic, although these have the disadvantage of biopsy margins being of poorer quality. The use of any source of diathermy also reduces the fresh tissue of the piece, reducing its diagnostic sensitivity.
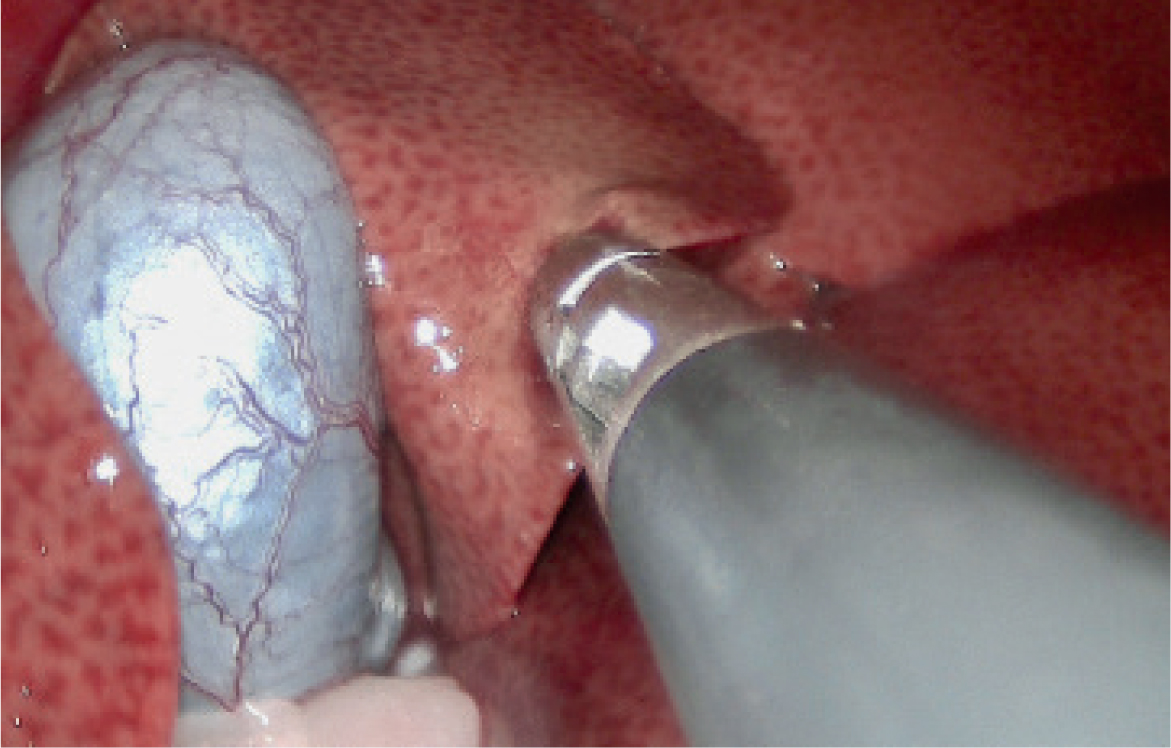
The laparoscopic procedure itself is relatively straightforward. An abdominal approach can be performed through two access portals, which allows not only the biopsy, but also the correct exploration of the entire abdominal cavity. The trocars are usually arranged on the midline, placing the portals on the periphery of the umbilical scar, according to the surgeon's preference. The standard size of the portals is 5 mm in diameter. Once the biopsy site has been selected, the forceps closes on it, causing the tissue to be cut (Figure 2). In the case of diffuse pathology, the biopsy is usually taken at the border of several liver lobes, as this is the most accessible place. Sometimes the piece is not completely detached from the liver, so it is necessary to rotate the tip of the instrument to tear the more fibrous tissue. It is important to handle the tissue with caution; given its friability, a larger portion than desired can detach, with the consequent bleeding. If the bleeding does not disappear by itself, the monopolar coagulation of the laparoscopic instrument itself can be used, or a small fragment of collagen sponge can be deposited on the bleeding site (McDevitt et al, 2016).
Pancreatic biopsy
Pancreatic biopsy is indicated when any non-suppurative pancreatitis, pseudocyst or pancreatic abscess, neoplasia or chronic pancreatitis is suspected. Especially useful in weak or old animals where rapid recovery is desired, laparoscopic pancreatic biopsy is an excellent method as it provides easy access to the right pancreatic lobe after identification of the descending duodenum (Cosford et al, 2010).
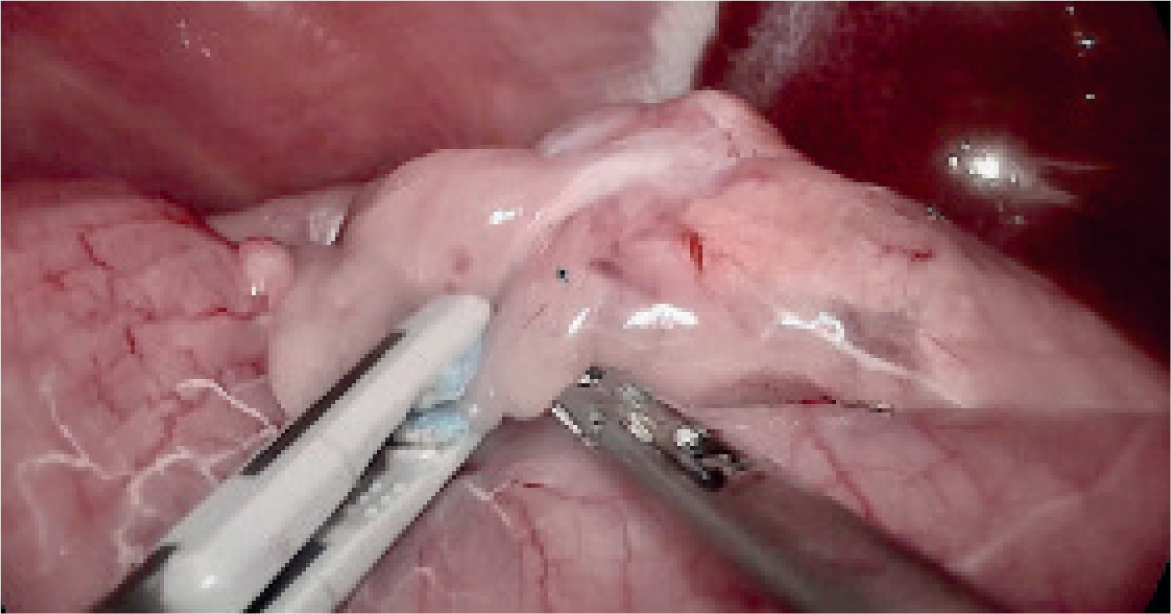
Another important advantage is the possibility of exploring both the pancreas and the extrahepatic bile ducts and hepatic portal, as well as the state of the peripheral abdominal viscera, such as the intestinal loops, in search of signs of peripheral inflammation. As described for liver biopsy, the approach to the abdomen through three access portals is preferable, as it allows comfortable handling of the viscera (Figure 3).
Laparoscopic procedures for pancreatic disease not only help the biopsy procedure, but also allow the operator to explore the pancreas and its relationship with the surrounding organs, such as the spleen and liver. Laparoscopic explorations allow for evaluation of the best puncture site, without any risk to the pancreatic ducts (Webb and Trott, 2008).
Pancreatic biopsy forceps are the standard instrument for its performance; although similar to the liver biopsy forceps, one of its jaws is inserted into the opposite, which increases the sealing capacity of the pancreatic tissue. To take the biopsy correctly, it is important to access the edge of the pancreatic lobe, generally the most exposed and accessible, thus avoiding trauma to the larger pancreatic ducts and extravasation of pancreatic enzymes. Once the biopsy point has been selected, the tissue is taken with the forceps, holding a few seconds before tearing the tissue, so that we increase its sealing. Post-biopsy bleeding is common, generally limited to no more than 3 minutes. Complications after pancreatic biopsy are infrequent, although a transient increase in pancreatic enzymes has been described, as well as the appearance of adhesions in the periphery of the viscus (Kim et al, 2014).
Splenic biopsy
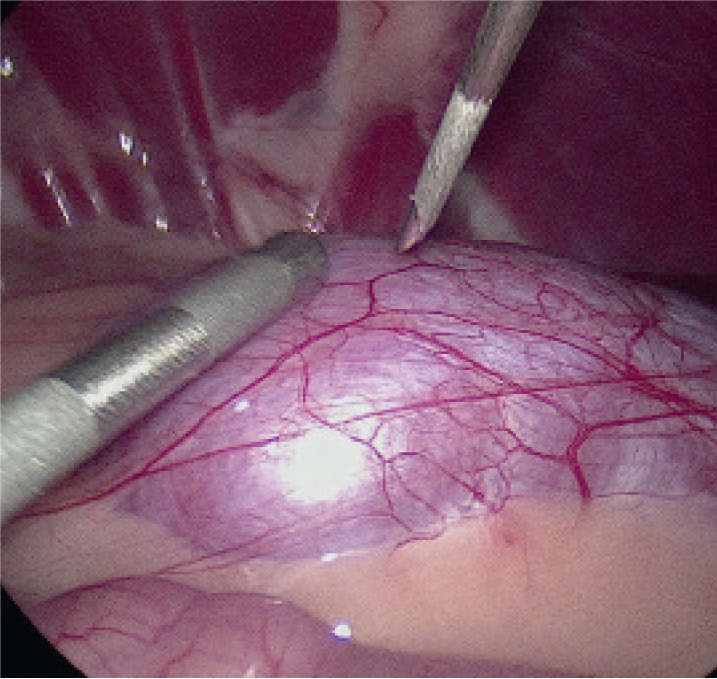
Splenic tissue samples can be taken by percutaneous needle aspiration for cytologic study, or by Tru-cut needle and cup forceps; although, histology is often preferred over cytology in certain clinical situations, for example when a tumour is suspected (Ballegeer et al, 2007). If the objective is only to sample the spleen, the laparoscopic approach can be performed using two 5 mm portals on the midline. When using cup forceps, the addition of a fragment of collagen sponge is usually recommended to ensure correct haemostasis. As the risk of morbidity related to the procedure is minimal, it is a good surgical option for geriatric or deteriorated patients (Figure 4). The use of vascular sealants using ultrasound (harmonics) has also been described with successful results for the collection of splenic tissue, although the sealants have been associated with a greater number of complications, such as peripheral inflammation and adhesions. Splenomegaly is the major indication for splenic biopsy. Guidance under direct visualisation makes this technique easy and safe, allowing direct observation of the spleen's appearance and making it possible to select the best place to take the biopsy (Radhakrishnan and Mayhew, 2013).
Renal biopsy
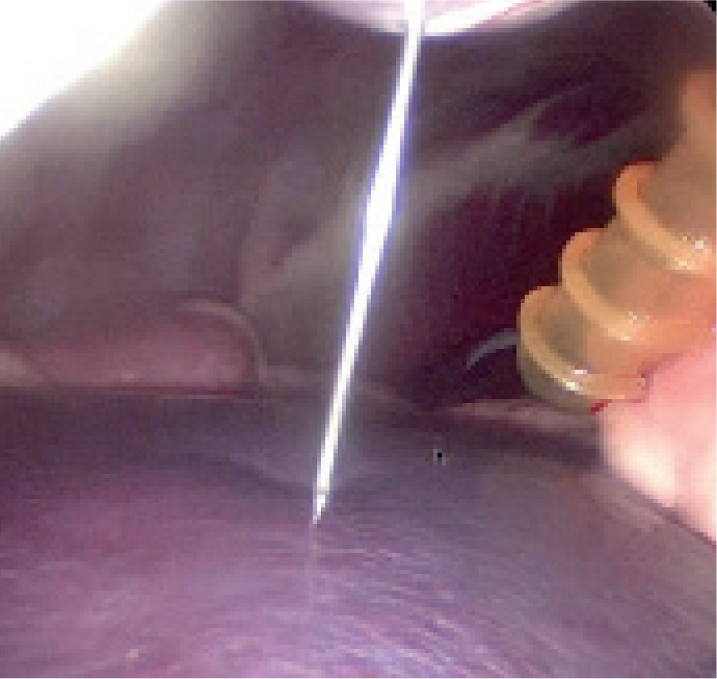
Renal biopsy may be required to establish a definitive diagnosis, determine the severity of a lesion and formulate an optimal treatment plan. Renal biopsy specimens can be collected via several methods. Percutaneous techniques are performed with ultrasound guidance in both dogs and cats, or blindly in cats (Rawlings et al, 2003). If ultrasound guidance is not available, the laparoscopic technique can be used in both cats and dogs (Figure 5).
The main advantage of laparoscopic renal biopsy over ultrasound-guided biopsy is the reduction in the morbidity of the procedure thanks to direct vision, which prevents inadvertent puncture of other abdominal viscera. The approach to the abdomen through two 5mm access portals is recommended, one for the optic and the another for an instrument to control bleeding. However, laparoscopic renal biopsy is not without potential complications; such as the excessive bleeding, puncture or laceration of large vessels such as the aorta and abdominal cavae, thus it is not recommended for patients in advanced stages of chronic kidney disease (Vaden, 2005).
There are several methods described for the approach to the kidney. The Tru-cut needle biopsy can be performed percutaneously by direct laparoscopic vision, preventing puncture of the renal hilum. Kidney biopsy using cup biopsy forceps, like liver biopsy, has recently been described as a safe method yielding a greater collection of glomeruli compared to needle biopsy (Park et al, 2017). As a drawback, it should be noted that the biopsies performed with the cup forceps do not reach the medullary tissue, while a needle can reach the renal cortex and medulla. Bleeding from the biopsy site usually subsides after 3 minutes, and any laparoscopic instrument can be used, even with the support of a swab or gauze to pressure the biopsy site and promote haemostasis (Park et al, 2017).
Laparoscopic techniques are useful for diagnosing primary renal disease, assessing the nature and severity of renal involvement in various systemic disorders; its use in obtaining renal biopsy specimens has several advantages over the blind technique (Figure 5). For example, direct visualisation of the kidney after biopsy and the possibility for the operator to observe the amount of haemorrhage (Nowicki et al, 2010). While complications can arise with any of these techniques, they are less frequent when an experienced operator uses the proper technique. Renal biopsy specimens must be processed and evaluated appropriately if consistent and accurate diagnoses are to be rendered.
Laparoscopy-assisted full-thickness intestinal biopsy
Full-thickness intestinal biopsy can be performed using a laparoscopically-assisted technique, allowing excellent visualisation of any intestinal section without the need for large abdominal incisions, which can delay recovery (Barry et al, 2017). To perform such a technique, the piece of intestinal tract to be biopsied is selected and exposed through one of the ports to partially exteriorize the viscera and complete the full-thickness biopsy in a conventional manner (Rawlings et al, 2002). After extracorporeal synthesis of the intestinal wall, the intestine is reintroduced into the abdomen and the abdominal wall is layered closed in the conventional manner (Figure 6).

It is also possible to perform this procedure purely laparoscopically, a technique that consists of opening the intestinal wall to explore the mucosa, recover foreign bodies that obstruct the intestinal lumen or perform a biopsy. The method is completed by suturing the intestinal incision. Since the procedure is performed within the intestines, the surgeon must take great care to avoid peritonitis. A retrieval bag should be used to remove masses or foreign bodies. Surgical knowledge of intracorporeal laparoscopic suturing is needed to reduce time and subsequent risk (Freeman, 2009).
Mesenteric and iliac lymph node biopsies
The laparoscopic approach to the mesenteric nodes allows the collection of biopsies of high diagnostic quality. Its topographic location in the abdomen is found by identifying the cecum and the root of the mesentery, where the cranial mesenteric lymphocenter is located (Figure 7). Direct laparoscopic vision can be used for percutaneous lymph node puncture, or laparoscopic instruments such as scissors and dissector can be used to obtain a lymph node fragment (Balsa and Culp, 2019).
Recently, bilateral excisional biopsy of the iliac lymph nodes, located at the bifurcation of the abdominal aorta at the external and internal iliac arteries has been successfully described, with a low rate of complications, using the ventral laparoscopic approach. Given that minimally invasive lymph node excision is safe, efficient and provides diagnostic quality biopsy specimens, a minimally invasive approach may improve owner acceptance of medial iliac lymph node biopsy as a staging procedure for different tumoral processes (Lim et al, 2017).
Lung biopsy
The diagnosis of pulmonary disease in small animals is a challenge for veterinarians, so it is necessary to obtain samples to establish a definitive diagnosis (Figure 8). Thoracoscopy is a minimally invasive surgical technique that allows the surgeon a direct exploration of the thoracic cavity and pleural space using a thoracoscope (Monnet, 2009). Tumoral resection can be carried out through tiny incisions (Adamiak et al, 2008). Diagnostic tissue percentage is comparable to that obtained by transthoracic needle puncture or transbronchial biopsy. Therefore, reliable diagnosis can be achieved without the need for more invasive techniques. Morbidity and postoperative recovery times are far lower than with thoracotomy (Mayhew et al, 2012) and it is considerably less painful, aiding a more rapid surgical recovery (Schmiedt, 2009.)
Lung biopsies should be taken with a pre-tied ligature loop or surgical staples to avoid air leakage. Advanced sealing devices have been assessed in cadaveric models. However, there are controversial results and no clinical safety study has been reported (Marvel and Monnet, 2013; Brückner et al, 2019). After the sample is taken, an air leak test should be performed.
If a neoplasm is suspected, lung and pleural biopsies should be taken without touching thoracic structures or walls, as portal site metastasis has been reported (Brisson et al, 2006). Pleural biopsies can be taken with biopsy forceps.
Video-assisted thoracoscopic surgery extirpation of the tracheobronchial lymph nodes has recently been described as a feasible and safe method, useful for obtaining more detailed staging on microscopic disease status in oncological patients (Steffey et al, 2015).
General complications
The intra-operative complications of laparoscopic surgery in veterinary medicine range between 2–35% and typically result from the introduction of Veress needle and trocars, or improper handling (Monnet, 2019), including drilling and viscera laceration, haemorrhage and subcutaneous emphysema, hence, 7–21% of laparoscopy surgeries require conversion to laparotomy (Monnet and Twedt, 2003; McClaran and Buote, 2009; Buote et al, 2011). In the postoperative period, where seroma may be observed at the entry site, anaemia and hypotension significantly increase the risk of complications, particularly in elderly and underweight patients (Maurin et al, 2020) where the risk of technical difficulty is increased. As indicated, the risk of complications depends on the experience of the surgical team, and more are seen in the learning stages (Oviedo-Peñata et al, 2020).
Summary
With more research into new techniques and instruments, laparoscopic surgical procedures can increasingly be used over conventional surgery, to perform numerous diagnostic and surgical procedures in small animal medicine. The use of laparoscopic biopsy can help to delineate the true cause of a patient's condition and thereby improve the success of subsequent therapeutic interve, minimising the adverse effects associated with conventional techniques. Furthermore, when applied by an experienced surgeon, laparoscopy can provide informative results with little to no complications.
KEY POINTS
- Minimally invasive surgery has multiple benefits: less surgical trauma, better recovery and shorter hospital stays.
- Laparoscopic biopsy is an established technique with proven excellent results.
- Biopsy increases the diagnostic capacity of laparoscopy.
- Laparoscopy is a less aggressive technique than laparotomy, so it facilitates postoperative recovery.


