Acute oropharyngeal puncture wounds are relatively uncommon occurrences in general practice but are potentially life-threatening events if not recognised (Griffiths et al, 2000). In cats and dogs, they can be caused by a variety of foreign bodies such as wood, metal, bones, sewing needles and fish-hooks (White and Lane, 1988; Griffiths, et al, 2000). In dogs, the most common presentation is associated with carrying, chewing or retrieving wooden sticks (Hallstrom, 1970; White and Lane, 1988; Doran, et al, 2008; Anderson, 2017). More severe injuries often occur when an owner throws a stick that embeds in the ground and the dog runs onto the protruding end with an open mouth (Bray, 2019). Medium to large breeds of dog appear to be over-represented among dogs with puncture wounds caused by sticks, and a relationship between large breeds and low head carriage at the time of stick retrieval is believed to be a possible cause for these cases (White and Lane, 1988; Griffiths et al, 2000). While more commonly seen in dogs, a case of a wooden oropharyngeal foreign body has been reported in a Bengal cat (Bright et al, 2002).
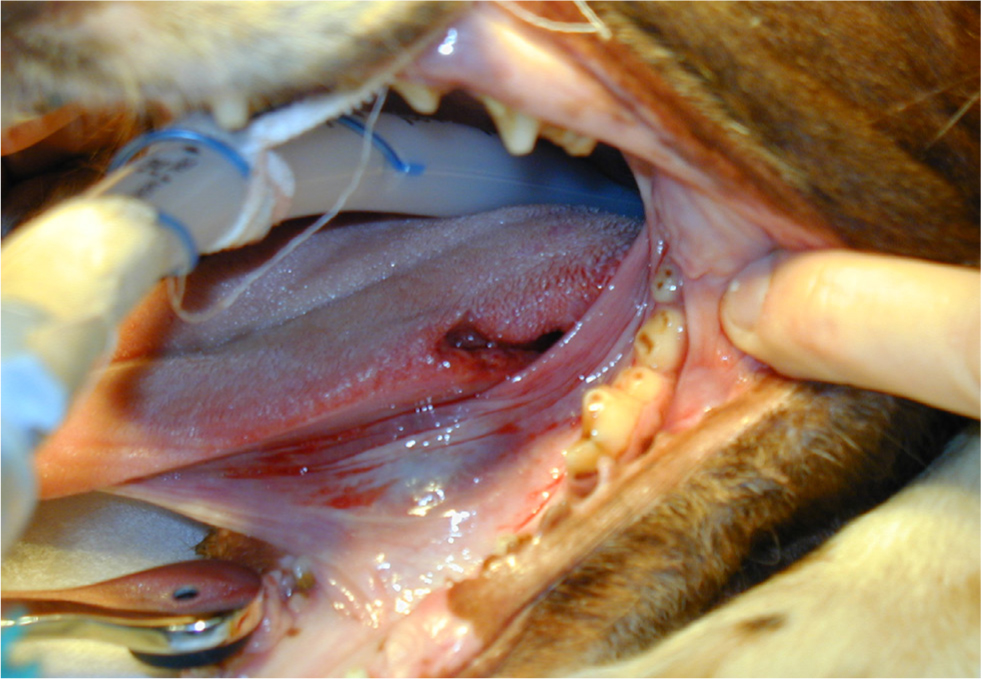
Two presentations of oropharyngeal injury are typically seen clinically; the acute and chronic stages (Griffiths et al, 2000; Doran et al, 2008). Acute injury is defined as an injury that is presented within seven days of the traumatic event, while chronic cases are those presenting after this time (White and Lane, 1988). This review will focus mainly on the acute phase (Figure 1), and how an aggressive and thorough approach can help avoid death or development of chronic discharging sinuses.
History and physical examination
Owners may recognise a specific event leading to the injury, such as their dog running for or retrieving a stick (Robinson et al, 2014). Alternatively, owners may be out of sight from the event and the presenting signs might raise suspicion of an oropharyngeal stick injury. In one study, only 12% of cases were presented to a vet within seven days of injury despite 48% of all the cases having a known history of oropharyngeal penetrating trauma (Griffiths et al, 2000).
Symptoms will vary depending on the type and extent of the injury caused by different sized objects. Presenting signs in acute cases are often a combination of cervical pain, pain on flexion of the neck, gagging, hypersalivation, blood-tinged saliva, dysphagia and depression (Doran et al, 2008; Robinson et al, 2014; Anderson, 2017).
Less frequently, oropharyngeal stick injuries can affect the central nervous system or retrobulbar space. These animals may show a wide range of clinical signs such as tetraparesis, changes in mentation and exophthalmos (O'Reilly et al, 2002; Rayward, 2002; McKenzie et al, 2017; Bosma et al, 2021).
An initial primary survey should be performed to assess the airway, breathing, circulation and neurological status of the patient (Reineke et al, 2014). Oxygen therapy may be indicated where pharyngeal swelling or mediastinal emphysema causes dyspnoea (Reineke et al, 2014). In cases with severe pharyngeal swelling or laryngeal trauma, a temporary tracheostomy tube may be required (White and Lane, 1988). Aggressive intravenous fluid therapy may also be indicated to correct hypovolaemia (Doran et al, 2008). If a contaminated wound has been identified, antibiotic prophylaxis is indicated before surgery (Anderson, 2017; Fossum et al, 2018). In the absence of bacterial culture and sensitivity tests, antibiotic choice is made on the likely bacterial contamination present. Staphylococcus aureus, Streptococcus spp. and Escherichia coli are the most common commensal bacteria of the canine oropharynx (Clapper and Meade, 1963; Quinn et al, 2001). Clostridium spp. are among the common soil-borne bacteria that pose a risk for wound infections in traumatised tissues (Neu and Gootz, 1996; Quinn et al, 2001; Doran et al, 2008). A combination of intravenous amoxycillin-clavulanate and metronidazole is commonly used in cases of oropharyngeal stick injury (Doran et al, 2008).
A thorough oral examination is often difficult to perform in a conscious healthy patient; it is even more challenging in cases of oropharyngeal stick injuries because of the pain and discomfort related to this condition. Urgent assessment under general anaesthesia is indicated to allow a detailed oropharyngeal examination (Reiter and Soltero-Rivera, 2017; Fossum, 2018).
Assessment of the oropharynx
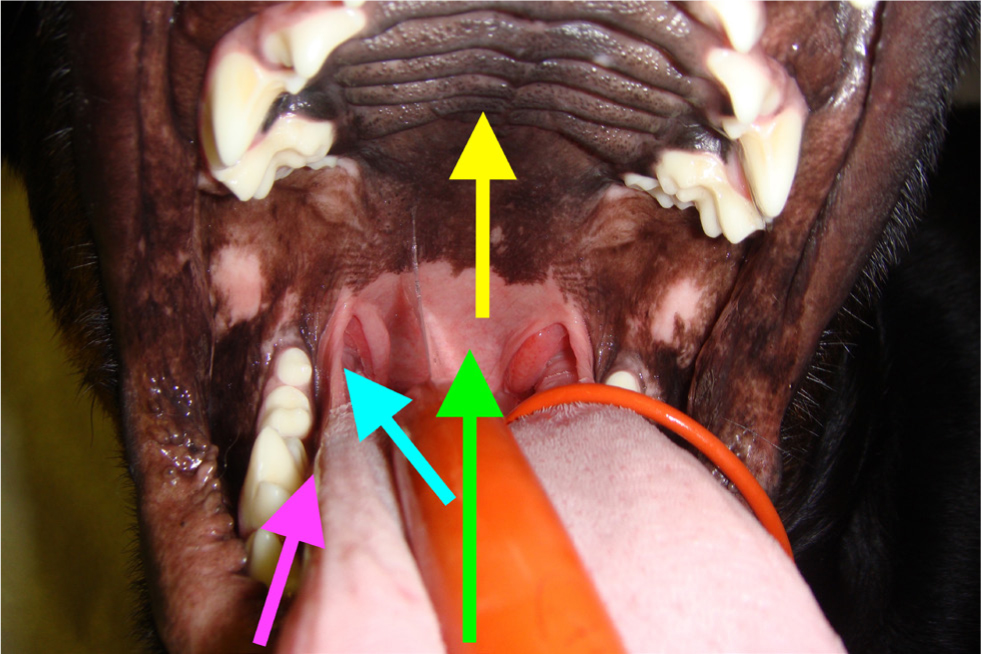
Following the induction of anesthesia and intubation, a thorough inspection of the oral cavity and pharynx must be performed (White and Lane, 1988; Fossum, 2018). As the time from initial injury increases, the chances of finding an oral wound decrease because the oral mucosa heals rapidly. Equipment such as long bladed laryngoscopes, tongue depressors and a good light source can significantly improve the oral examination (Doran et al, 2008) (Figure 2).

Speculated trajectories of penetrating oropharyngeal foreign bodies include the sublingual gutter, lateral pharyngeal wall, tonsillar regions, and the rostral and dorsal pharynx (Griffiths et al, 2000; White and Lane, 1988) (Figure 3). Initial inspection of both sides of the tongue and the sublingual area involves pulling the tongue laterally, forward and dorsally (Doran et al, 2008; Reiter and Soltero-Rivera, 2017). The blade of the laryngoscope can be used to probe tissue, displace it and identify areas of trauma (Griffiths et al, 2000; Doran et al, 2008). Additionally, a blunt probe or spey hook can be useful to retract the soft palate rostrally. The tonsillar, pharyngeal and perilaryngeal mucosa, and the oral palatal surfaces should then be inspected (Doran et al, 2008). A full examination should be performed as multiple wounds may be present; for example, when an object penetrates the soft palate with a dorsal trajectory, it is common to see injuries to the dorsal nasopharynx that might be obscured by the soft palate (Figure 4).

Diagnostic imaging
Radiography
Orthogonal radiographs of the pharynx, cervical region and thorax should be obtained (Anderson, 2017; Fossum, 2018). Wooden foreign bodies may or may not be seen on radiography (Doran et al, 2008; Fossum, 2018). Once wood is embedded within muscle and fascia, it often absorbs surrounding water and becomes isopaque relative to the surrounding tissues, making it invisible on plain radiography (Griffiths et al, 2000). A common finding in acute oropharyngeal injuries is the presence of cervical emphysema (Griffiths et al, 2000; Doran et al, 2008) (Figure 5). Cervical emphysema is defined as free gas within the cervical soft tissues, outside the lumen of the oesophagus or the trachea (Doran et al, 2008). This is an indication for surgical exploration of the neck (Doran et al, 2008). Gas extending down the fascial planes of the neck, subcutaneously and within the mediastinum is taken as an indicator of likely oesophageal injury rather than pharyngeal (White and Lane, 1988; Huck and Kyles, 2017) (Figure 6). Not all cases with confirmed penetrating injuries will show changes on radiography and false negatives are possible (Griffiths et al, 2000; Robinson et al, 2014).


Ultrasonography
Ultrasonography can be used to show hyperechoic linear material with shadowing; however, wooden material may not be readily identified (Fossum, 2018). Therefore, ultrasonography is not commonly used in the acute patient since subcutaneous emphysema can mask small foreign bodies (Peeters, 2010).
Endoscopy/Sigmoidoscopy
If endoscopy is available, the oesophageal lumen can be evaluated (White and Lane, 1988; Huck and Kyles, 2017). By passing the endoscope to the level of the cardia, assessment of the mucosa can be made while the scope is withdrawn (Doran et al, 2008). Evaluation of the upper oesophageal sphincter dorsal to the larynx poses a challenge because of poor visualisation at this location (Griffiths et al, 2000). In one study, four out of six oesophageal tears were missed using flexible endoscopy (Griffiths et al, 2000). It was suggested this was a result of the tendency towards red out from the cricopharyngeus muscle and because insufflation is not effective in this region. Therefore, if oesophageal injury is suspected, assessment of the dorsal oesophageal wall at the level of the cricopharyngeus muscle is important (Griffiths et al, 2000). Evaluation of this area is best done with a rigid endoscope (Robinson et al, 2014). These can be used to explore tracts, lavage and remove debris.
Advanced imaging
Advanced imaging, such as computed tomography and magnetic resonance imaging, have not been evaluated for their use in acute oropharyngeal injury. Computed tomography and magnetic resonance imaging have been shown to be useful in chronic cases (Dobromylskyj et al, 2008; Nicholson et al, 2008; Anderson, 2017). Computed tomography can be useful for identifying wooden foreign bodies because of its removal of superimposition and cross-sectional nature when compared to radiography (Lamb et al, 2017).
Surgical treatment
In dogs with simple, acute, rostral oropharyngeal penetrations with no radiographic abnormalities, an oral approach is used to manage the wound (Doran et al, 2008). Wounds should be probed and explored to assess the depth of penetration and to remove any residual foreign material present (Griffiths et al, 2000; Doran et al, 2008; Fossum, 2018). The pharynx should be packed before copious lavage with lactated ringers' solution to minimise any residual contamination and dislodge any remaining foreign material (White and Lane, 1988; Anderson, 2017). The decision to close a wound will depend on the viability of the tissue, the chronicity of the wound and the amount of drainage that is anticipated (Fossum, 2018). Superficial sublingual wounds or those of the soft palate may be left open to granulate (Doran et al, 2008). Larger deeper pharyngeal wounds may require closure and drainage is established (Fossum, 2018).
Surgical exploration via a ventral cervical midline approach is indicated for dogs with caudal pharyngeal punctures, confirmed.
Postoperative considerations
Supportive care will need to continue in the postoperative period including analgesia, antibiosis, fluid therapy and nutrition (Doran et al, 2008; Fossum, 2018). All patients should be closely monitored for signs of pain or wound dehiscence (Fossum, 2018). Cases where pneumomediastinum or pneumothorax are identified require oesophageal punctures or where cervical emphysema is identified on radiography (Doran et al, 2008; Anderson, 2017; Fossum, 2018). Early surgical exploration allows removal of foreign material, repair of pharyngeal or oesophageal tears, lavage to reduce contamination and the establishment of adequate drainage (White and Lane, 1988; Griffiths et al, 2000; Doran et al, 2008; Nicholson et al, 2008).
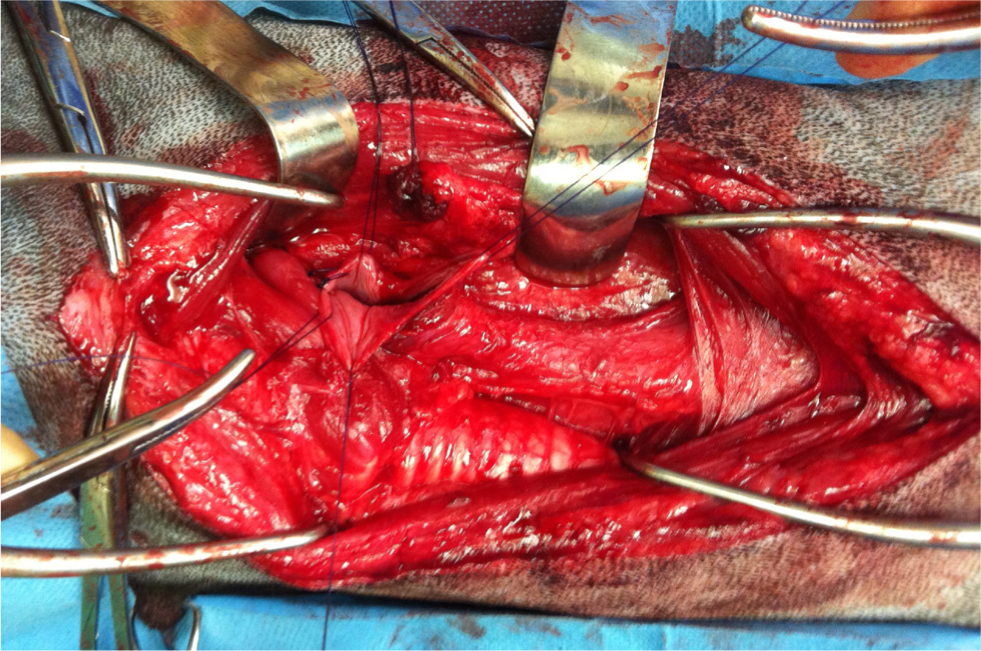
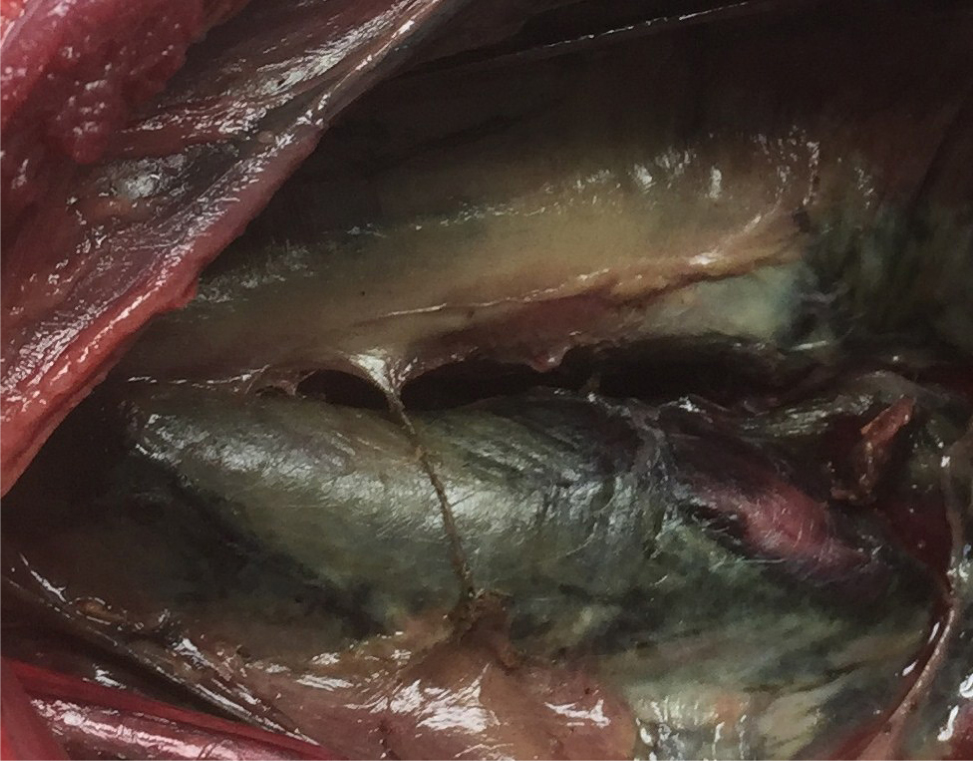
Once anaesthetised, the animal is placed in dorsal recumbency, and a large surgical clip and routine skin preparation is performed (Figure 7). Surgery can be aided by placing a sterile probe within the oral wound to help identify tracts in surgery (Griffiths et al, 2000). A skin incision is made from the cricoid cartilage extending caudally for two-thirds of the distance to the manubrium (Doran et al, 2008; Huck and Kyles, 2017). Ensure that the recurrent laryngeal nerve is not disrupted during dissection (Anderson, 2017). The paired sternohyoid muscles should be identified, bluntly separated and retracted off the midline (Doran et al, 2008; Fossum, 2018) (Figure 7). The trachea and oesophagus are retracted as required (Doran et al, 2008) (Figures 8 and 9). In cases where extensive bruising, exudates or fibrin is present, identification of the oesophagus is aided by an assistant passing an oesophageal stethoscope or an orogastric tube into the oesophagus orally (Fossum, 2018). Blunt dissection of fascial tissues allows examination of the cervical and retropharyngeal region (Doran et al, 2008). Any foreign material is removed and the region is copiously lavaged with lactated Ringer's solution and suctioned to reduce contamination and remove exudates (Doran et al, 2008; Huck and Kyles, 2017).

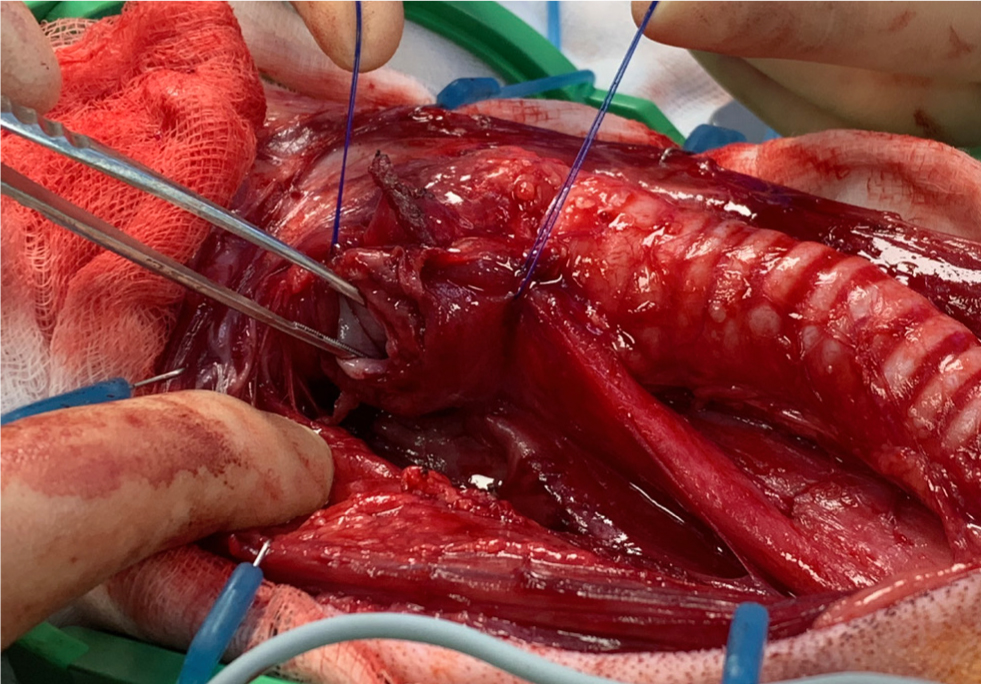
Oesophageal surgery differs from the rest of the gastrointestinal tract, and it is associated with a higher prevalence of incisional dehiscence. Factors such as a lack of mucosa, a segmental blood supply, lack of omentum, tension at the surgical site and constant movement from swallowing and respiration all contribute to the high complication rate (Huck and Kyles, 2017). Oesophageal lacerations should be minimally debrided and a single, or double-layer interrupted pattern is used to close (Griffiths et al, 2000; Huck and Kyles, 2017; Fossum, 2018). Oesophageal repair may be supported using a pedicle flap created from local muscle. Muscles such as the sternothyroid, sternohyoid and longus colli can be used depending on the location of the lesion (Huck and Kyles, 2017). Omentum can be used to support caudal thoracic oesophageal wounds (Huck and Kyles, 2017).
Swab or tissue samples can be obtained after lavage for culture and sensitivity. Antimicrobial therapy can then be modified based on these results (Anderson, 2017). Placement of a surgical drain is indicated to reduce dead space and any residual contamination. Active closed suction drains are more suitable than passive drains in this area, as they do not require a dependent exit point or repeat bandaging (Anderson, 2017). Drains are placed within the cervical soft tissues, dorsal to the sternohyoid muscles (Anderson, 2017; Fossum 2018) (Figure 10).

Oropharyngeal bypass can be performed if deemed necessary (Doran et al, 2008; Fossum, 2018). Gastrotomy tube placement under endoscopic guidance is recommended for postoperative nutritional support and to provide medications (White and Lane, 1988; Doran et al, 2008; Fossum et al, 2018). Alternatively, a surgical flank approach can be used (Davidson, 2017) (Figure 11). repeat imaging to ensure there is no progression or evidence of mediastinitis (Doran et al, 2008; Fossum, 2018). Surgical drains should be monitored, and outputs should be recorded. Drains are removed when fluid recovery falls to an acceptable level (less than 0.5 ml/kg/day) (Doran et al, 2008). Gastrostomy tubes should be left in situ for a minimum of 10 days to allow adequate adhesions to form between the stomach and body wall (Davidson, 2017). Gastrostomy tubes should be left in until enteral feeding is no longer required (Davidson, 2017). Doran et al (2008) fed cases on day 10 postoperatively, and if there was no evidence of dysphagia or regurgitation, the tubes were removed on day 11.

Prognosis
The prognosis of oropharyngeal stick injurys is variable and cases with injury confined to the oropharyngeal region have a better prognosis than those involving the oesophagus (Doran et al, 2008). In dogs where all injuries are identified in the acute phase and treated promptly the prognosis is fair (White and Lane, 1988; Griffiths et al, 2000; Doran et al, 2008; Robinson et al, 2014). It is essential that oesophageal tears are identified promptly and treated aggressively. The poor prognosis reported in cases of oesophageal perforation is said to be associated with progressive cellulitis and subsequent respiratory compromise, mediastinitis, pneumomediastinum, pneumothorax and septic shock (White and Lane, 1988; Doran et al, 2008).
Chronic presentations
Chronic cases rarely exhibit signs of systemic disease, and the presenting complaints are usually discharging sinuses, chronic abscessation, cervical swellings or dysphagia secondary to the presence of foreign material (White and Lane, 1988). In many cases, transoral inspection for the initial site of injury is rarely rewarding (Anderson, 2017). Advanced imaging followed by exploration and excision of abscesses and tracts is usually undertaken (Griffiths et al, 2000; Nicholson et al, 2008) (Figure 12). Identification of a foreign body and complete resolution of clinical signs is variable.
Conclusions
Acute oropharyngeal injury is a relatively uncommon presentation in first-opinion practice, but is potentially life threatening. The literature shows a benefit from an aggressive and thorough approach to these injuries on initial presentation. Multiple methods can be used to manage these injuries, including endoscopic debridement and cervical exploratory surgery. If the indications for surgical exploration are present, it is important to proceed rapidly or offer prompt referral. Cervical exploration via a ventral midline approach remains the best option for managing oesophageal perforation. This exploration prevents associated acute complications that can be fatal and prevents chronic sinuses forming from residual foreign material.
KEY POINTS
- Acute oropharyngeal injury is uncommon in first-opinion practice but is potentially life threatening.
- There are multiple ways these injuries can be treated, from debridement and lavage through to cervical exploratory surgery.
- Wounds associated with oropharyngeal injuries are most likely contaminated, therefore antibiotic prophylaxis should be considered.
- Concern over dorsal pharyngeal or oesophageal injury warrants surgical exploration of the cervical region.
- Early exploration of acute oropharyngeal injury prevents associated complications and avoids the development of chronic abscesses.


