The prevalence of chronic enteropathy in veterinary patients is not known, but is estimated to be 1–2% (Dandrieux, 2016) of referral cases with 20–30% of companion animal veterinary visits related to vomiting and/or diarrhoea (O'Neill et al, 2014). Diet modification can be an important aspect of patient management with the potential to improve clinical signs in ≥50–65% of cases (Jergens and Heilmann, 2022). Choosing diets for patients with chronic enteropathy must be based on a thorough nutritional assessment. Clinical signs and physical examination findings are used to localise the extent of the gastrointestinal tract involved. Diet selection will then consider changing the macronutrient content (level of protein, fat or fibre) or ingredient list (utilisation of hydrolysed or novel proteins). Multiple diet trials are often required to find the best diet, and it is important to note that many patients will show improvement with diet change even if the first diet trial is not successful (Jergens and Heilmann, 2022).
Perform a thorough nutritional assessment
Nutritional assessment starts with the collection of a detailed diet and medical history, a thorough physical examination and evaluation of diagnostic findings. For both dogs and cats, it is essential to identify all previous diets fed, treats, snacks and any other foods offered including those used to administer medications, as well as any potential food preferences (such as flavours and textures). Signalment, clinical signs including characterisation of gastroin-testinal symptoms (eg vomiting, diarrhoea) along with changes in body weight (including a time frame of any weight loss) are key details of a patient's history. Diet history forms are downloadable from the World Small Animal Veterinary Association and the American College of Veterinary Internal Medicine (Nutrition) (Box 1). Physical examination should include assessment of hydration, body condition score, muscle mass score, rectal exam and assessment of faecal quality, haircoat and skin quality, presence/absence of effusion or oedema and abdominal palpation for masses or intestinal thickening. Scoring indices are helpful for dogs to characterise the severity of the disease, such as the canine chronic enteropathy clinical activity index and the canine inflammatory bowel disease activity index (Jergens et al, 2003; Allenspach et al, 2007). Higher scores correlate with more significant inflammation and may indicate which patients need more intensive diagnostic evaluations sooner in the course of their illness (Jergens et al, 2003). A scoring system is also available for cats (the faecal chronic enteropathy clinical activity index) but, in the authors' experience, it may not be as helpful for assessing the severity of disease. Faecal scoring is also a helpful tool to assess the patient's current stool quality and monitor any changes that occur during medical and nutritional interventions (Purina, 2024).
Box 1.Diet history forms
- American College of Veterinary Internal Medicine (Nutrition): acvn.org/wp-content/uploads/2020/04/ACVN-Diet-History-Form-2020-FINAL_fillable.pdf
- World Small Animal Veterinary Association: wsava.org/wp-content/uploads/2020/01/Nutritional-Assessment-Checklist.pdf
Localise the disease process
Gastrointestinal signs commonly noted with chronic enteropathies include variable appetite, vomiting (recurrent and/or intermittent), diarrhoea (small intestinal, large intestinal or mixed) and weight loss. Additional signs may include regurgitation (possibly secondary to oesophagitis from recurrent vomiting), flatulence, abdominal pain, haematemesis, tenesmus, haematochezia, melena or constipation. Identifying the predominant clinical signs will help identify the location of the disease (Table 1). Decreased or variable appetite along with weight loss and vomiting is more likely to be associated with small intestinal or mixed bowel disease compared to solely large bowel disease, although some exceptions may apply such as with granulomatous colitis or megacolon. Tenesmus, urgency and increased frequency of defection along with mucous or frank blood in the stool is more often seen with large bowel disease (Tams, 1996; Hall and Day, 2017). Identifying the location of the affected area of the gastrointestinal tract will help identify key nutrients of concern (such as protein, fat, fibre, digestibility, cobalamin) and targeted nutrient levels (high vs low) for appropriate diet trials (Allenspach et al, 2007; 2016; Kathrani, 2021; Lenox, 2021).
Table 1. Small vs large bowel clinical signs
| Clinical sign | Small bowel | Large bowel |
|---|---|---|
| Appetite | Normal or decreased | Normal |
| Weight loss | Common | Uncommon |
| Vomiting | Often present | Rarely present |
| Defecation frequency | Normal | Increased |
| Defecation urgency | Normal | Increased |
| Tenesmus | Absent | Present |
| Mucous in stool | Uncommon | May be present |
| Haematochezia | If present, more often dark or tarry in colour | If present, more often frank blood |
| Stool volume (per bowel movement) | Normal to increased | Normal to decreased |
Diet trials for chronic enteropathy
Since 50–66% or more of patients with chronic enteropathy may respond to diet change, performing a trial on a new, carefully selected diet can be both an effective diagnostic and treatment intervention that may be implemented with low risk of adverse effects (Guilford et al, 2001; Allenspach et al, 2007; Volkmann et al, 2017). Diet change may accomplish complete remission of clinical signs for some patients if food-responsive enteropathy is present, or it can achieve longer remission rates for antimicrobial- or immunosuppressant-responsive enteropathies (Volkmann et al, 2017; Dandrieux and Mansfield, 2019). A clinical response is often seen within the first 2–3 weeks of exclusive feeding, unlike diet trials for dermatological concerns which commonly require 8–12 weeks to observe clinical improvement (Allenspach et al, 2016; Fischer et al, 2021).
Identify key nutrients of concern
To select an appropriate diet for a diet trial, the prior diet history and disease localisation should be taken into consideration. It is helpful to create a table to compare diets with the macronutrient data and the ingredient list (Table 2). Key nutrient levels to consider are protein, fat, digestible carbohydrate and fibre. Comparing nutrient levels and ingredients in commercial diets already fed to the animal can help establish what macronutrient levels and ingredients have already been tried without success. Diets fed should be compared using g/100 kcal, or on a dry matter basis (Box 2). With this information, the appropriate diet for a trial can then be chosen (Table 3). In some cases, the diet selected or formulated must accommodate more than one desired feature (eg novel protein, fibre-enriched and/or low fat) or address the patient's life stage (eg growth). Commercial products will carry labelling identifying which life stage a diet is appropriately formulated for. Laboratory testing should be evaluated to assess the possible need for additional dietary supplementation (eg cobalamin, folate, calcium, magnesium, fat-soluble vitamins). Owners have a choice of feeding a commercial therapeutic diet or a balanced, properly formulated home-prepared diet, and the benefits and limitations of each should be discussed with the owner.
Table 2. Example of diet history for a feline patient – macronutrient data, ingredient list and clinical signs
| Product | Protein g/100 kcal | Fat g/100 kcal | CHO g/100 kcal | Fibre g/100 kcal | Select ingredients | Signs |
|---|---|---|---|---|---|---|
| 9 Lives wet | 8.8 | 4.4 | 3.4 | 1 crude | Meat, whitefish, poultry | Large bowel diarrhoea, faecal score 7 |
| Royal Canin GI Fiber Response Dry | 8.0 | 3.9 | 10.0 | 2.9 TDF0.7 crude | Chicken, corn, wheat | No change |
| Royal Canin Sensitive Digestion | 8.1 | 5.1 | 6.5 | 1.5 TDF0.3 crude | Chicken, corn, wheat | No change |
| Purina EN canned | 11.8 | 4 | 3.9 | 1.6 TDF0.3 crude | Meat, turkey, soy | No change |
| Royal Canin GI Loaf | 8.4 | 5.6 | 5.2 | 0.6 TDF0.34 crude | Chicken | Faecal score 5 |
CHO – carbohydrate; TDF – total dietary fibre
Box 2.Comparing commercial diet nutrition data – convert from the guaranteed analysis (as fed) to g/100 kcal or dry matter basis to compare dietsPet food labels list nutrition data in a guaranteed analysis. This is referred to as an ‘as fed basis’. This is the food as seen when poured into the food dish. Generally, dry foods have similar moisture levels (around 10% moisture) and it is easy to compare nutrition information as reported on the label across dry kibble diets. Canned diets or fresh diets are higher in moisture, however, and vary quite a bit more (20–35% moisture). It is not possible to compare nutrients across these diets as the moisture dilutes the nutrient content.To compare foods of different moisture content, nutrient information must be converted to either an energy basis (g/100 kcal or 1000 kcal) or a dry matter basis which is essentially the nutrition information with the moisture removed (Hall and Day, 2017).As fed to energy basis (g/100 kcal or g/1000 kcal)Nutrients can be compared across diets on an energy basis, which is expressed as amount nutrient/1000 kcal or amount nutrient/100 kcal. This is the form that many nutrition clinicians, veterinarians and prescription diet product guides will follow.To convert nutrition data from a pet food label, the energy density of the diet or kcal/kg must be known.For this diet, the energy density is 3190 kcal/kgCrude protein = 23% as fed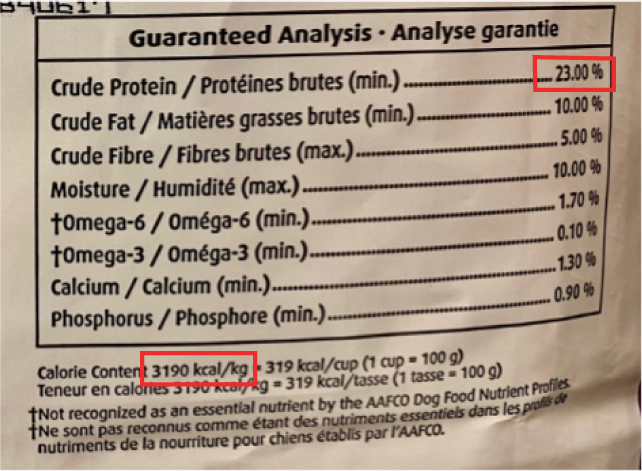
To convert the amount of crude protein from an as fed basis to g/100 kcal, follow these steps:Crude protein (as fed)=23%=23g protein ×kg food ×1000g100g food 3190kcal 1kg= 0.072g protein × 100 kcal=7.2g protein/100 kcalConvert as fed to dry matter basisHere is a guaranteed analysis. What is the % dry matter?% dry matter = 100 – moisture %= 100 − 11 = 89 Or 89% dry matterConvert as fed to dry matter crude protein = Amount protein % / (100 – moisture %/100)% dry matter crude protein = 21 / ( 100 − 11 / 100 ) = 21 / ( 89 / 100 ) = 21 / ( 0.89 ) = 23.6 % crude protein dry matter basis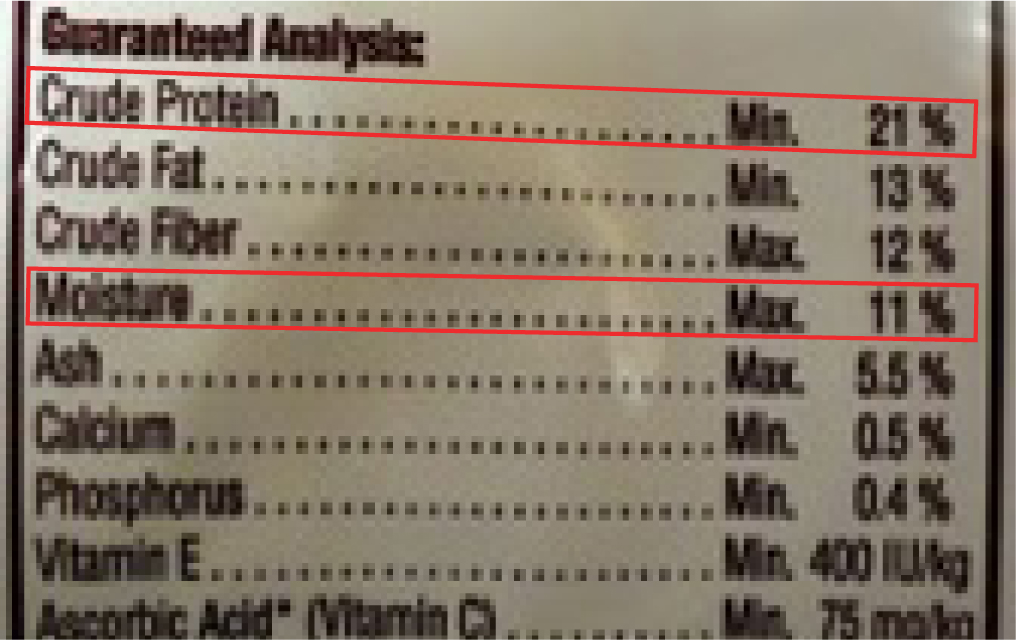
Table 3. Macronutrient levels in canine and feline diets
| Low (g/100 kcal) | Moderate (g/100 kcal) | High (g/100 kcal) | ||||
|---|---|---|---|---|---|---|
| Dog | Cat | Dog | Cat | Dog | Cat | |
| Protein | 3–4.75 | 4–7.5 | 5–7 | 8–11 | >7 | >11 |
| Fat | <3‘ultra-low’ <2.0 | <4.5 | 3–5 | 4.5–6.5 | >5 | >6.5 |
| Dietary fibre | <1.5 | <1.0 | 1.5–3.5 | 1–2.5 | >3.5 | >2.5 |
| Carbohydrate (digestible) | <10 | <3 | ||||
Diet selection for chronic enteropathy
Small vs large bowel Patients with clinical signs consistent with small intestinal disease may respond to a highly digestible, low residue gastroenteric diet containing modest amounts of mixed fibre sources (Tolbert et al, 2022). Fat content in therapeutic gastroenteric diets may be low, moderate or even high, so it is important to assess tolerance to fat or the need for fat restriction. Reducing fat intake may be beneficial for patients with gastroenterocolitis and a normal body condition score. Conversely, if no concerns for fat intolerance are present, if the patient is underweight or larger meal volume is not well tolerated (as rations very low in fat necessitate higher meal volumes), a moderate to increased fat content may be trialled to facilitate lower meal volumes, help with weight gain or prevent weight loss.
For large bowel disease, the initial diet trial should be a fibre-enriched diet (Tolbert et al, 2022). Fibre can have numerous purported health benefits including supporting the microbiome as a prebiotic, directly providing fuel for colonic mucosal cells and helping to ‘normalise’ stool quality by absorbing faecal water and/or promoting intestinal motility (Leib, 2000; Rossi et al, 2020). Increased dietary fibre intake may be achieved by selecting a therapeutic diet with a higher fibre content or by supplementing fibre with any diet. Options for this include:
- Psyllium husk fibre powder: 1–2 tsp/10 kg bodyweight per meal
- Powdered cellulose: dogs and cats: 0.5–1 g/kg bodyweight.
Fibres are characterised by their solubility, viscosity and intestinal fermentability, with most soluble fibres being viscous and more fermentable (eg beet pulp, inulin) and most insoluble fibres being non-viscous and non-fermentable (eg cellulose). However, fibres fall within a spectrum depending on their source (Box 3) (Rudinsky et al, 2018; Moreno et al, 2022). Foods contain a blend of fibres and concentrated fibre supplements are commonly added to commercial pet foods for many reasons including stool quality benefits (de Godoy et al, 2013; Fuller et al, 2016; Montserrat-Malagarriga et al, 2024). Caution is warranted when adding fibres to balanced commercial diets as they may interfere with diet digestibility and nutrient absorption. Choosing a balanced diet formulated to include the targeted fibre levels is preferable if available (National Research Council, 2006; Thatcher et al, 2010).
Box 3.Fibres (Rudinsky et al, 2018)
Hydrolysed vs novel protein
If a patient presents with dermatological signs as well as gastroenteric signs, or if no improvement is noted with the initial diet fed for a minimum of 2 weeks, a hydrolysed or novel protein diet may be fed to test if a food allergy is present as the combination of cutaneous and gastrointestinal signs increases the suspicion for adverse food reaction. Available only as a commercial diet option, hydrolysed therapeutic diets are manufactured by enzymatically hydrolysing proteins to small polypeptides and amino acids <3–5 kilodaltons. Mast cell degranulation requires proteins of sufficiently large size to crosslink immunoglobulin E antibodies and trigger degranulation (type 1 hypersensitivity), so hydrolysed proteins should ‘escape’ these immune responses (Cave, 2006). As many as 20–50% of still react to protein hydrolysates, so selecting a hydrolysed diet option using protein sources the patient has not consumed before is still recommended if possible (Kathrani, 2021). Hydrolysed diets are also proposed to be highly digestible and can benefit many patients with chronic enteropathies (Cave, 2006). However, commercial hydrolysed protein diets may be lower in total dietary fibre, so monitoring faecal scores is important. The authors have used fibre supplementation for some patients while using a hydrolysed protein diet to improve stool quality.
Novel protein diets are selected by identifying all previous protein exposures and then selecting a diet containing proteins that have not been fed previously. Novel protein diets may deliver a higher total dietary fibre content compared to hydrolysed diet options which may benefit some patients with fibre responsive enteropathies. Often these diets will also contain novel carbohydrate sources, but the importance of novel carbohydrate is uncertain (Johansen et al, 2017; Jackson, 2023). As pet foods available over-the-counter expand in the range of included ingredients, it is becoming increasingly difficult to identify diets based on strictly novel ingredients. As commercially available pet foods expand in their range of ingredients, it is becoming increasingly difficult to identify diets containing strictly novel ingredients. In addition, commercial diets not intended to be fed to patients with adverse food reactions or food allergies may be contaminated in manufacturing with trace amounts of other commercial foods as sterility is not required in the manufacturing of these diets (Raditic et al, 2011). As a result, diets used for a food trial should be formulated specifically for this purpose.
Low fat vs ‘ultra-low’ fat
If a patient has signs of fat intolerance or malabsorption (delayed gastric emptying, pancreatitis, hyperlipidaemia, lymphangiectasia, hypocholesterolaemia), a diet that is lower in fat than the current diet should be chosen. Fat malabsorption may lead to dysbiosis, colonic cell damage, increased faecal water content or adverse inflammatory effects which can worsen diarrhoea. Challenges with lower fat diets include low caloric density, which means higher food volumes must be fed to achieve the same calorie intake. In addition, fat is also a driver of palatability in diets which is beneficial for dogs with poor appetites (Kathrani, 2021; Tolbert et al, 2022; Myers et al, 2023).
Patients that fail to respond to the initial level of fat restriction may improve when fed an ‘ultra-low’ fat diet which has been carefully formulated to be very low in total fat content, yet still contain recommended levels of essential fatty acids and fat-soluble vitamins (Myers et al, 2023). This may be achieved by feeding a commercial therapeutic diet or a carefully balanced recipe formulated by a board certified veterinary nutritionist. Recipes may use medium chain triglyceride fats strategically, as they are generally more digestible and therefore may be useful for patients with compromised gastrointestinal tracts (Tolbert et al, 2022).
In some cases, there may not be a commercial diet option that addresses the key nutrients of concern for all comorbidities of the individual patient. Additionally, dogs and cats can have adverse food reactions or food intolerances to various commercial pet food ingredients including processing effects (Teodorowicz et al, 2017; Gupta et al, 2018), preservatives or emulsifiers (Kathrani, 2021). These situations may prompt the recommendation to use a limited ingredient, commercial fresh food diet option or a custom home-prepared diet formulated for an individual patient. Advantages of a homemade diet include precise customisation for an individual pet including ingredient selection, nutrient levels and palatability, and recipes can be sequentially changed or adjusted as needed based on the patient's response. Home-prepared diets can be formulated to be balanced with even lower fat levels than commercial therapeutic diets when needed. Once a recipe is identified that has improved clinical signs for the patient, a similar commercial diet may be trialled if available, or the patient may be fed the home-prepared diet long-term. Disadvantages of home-prepared or commercial fresh diets may include time commitment to shopping and food preparation, need for expanded cold storage, potential owner error and unknown bioavailability and digestibility. Homemade diets are often more costly than commercial therapeutic diets depending on the ingredients and supplements used (Kratzer et al, 2022). Home-prepared diets are typically lower in total dietary fibre content, so additional fibre supplementation may be required if a high fibre diet is desired. Currently, several commercial pet food companies are beginning to offer custom diet services for pet owners to make individualised recipes for pets; however, this service may be very costly for pet owners.
Rules of the diet trial
A transition to any new diet should be gradually made over a 7–14-day period, slowing the transition if negative clinical signs occur (eg vomiting, regression of faecal score). If performing an elimination diet trial, the diet trial begins at the point of feeding only the new diet. When a food allergy is suspected, it is critical to eliminate all other foods, treats and animal-based chews as well as flavoured supplements, dental care products and oral medications. Changing to topical heartworm or flea/tick products may eliminate oral exposures to confounding animal proteins or flavourings. It is optimal to eliminate all extra foods and treats – however, when treats or vehicles for medication administration are required, providing clients a list of ‘safe’ options is recommended to improve compliance (Table 4). For these additional treats, the authors recommend discussing with owners the potential for any food item to trigger adverse responses and to test foods in small quantity, one at a time for several days to confirm no adverse responses occur. Client compliance is essential throughout the entire diet trial period to assess the efficacy of the diet change. Pets must not be allowed to access unknown foods or scavenge if allowed outdoors unsupervised. During the diet trial, owners should keep a diary to track appetite, food intake, faecal scores (Cavett et al, 2021) and any other concerns. Interestingly, the authors have noted some patients will respond to a combination of diets which is discovered during the transition period (eg, feeding 50% new diet plus 50% old diet), so tracking responses during the transition is also recommended.
Table 4. Treats allowed during elimination diet trials
| Fruits | Banana, watermelon, apple, strawberry |
| Vegetables | Green beans, carrots, pumpkin, cucumber |
| For medications | Vegan marshmallows, pill dough made from potato, sweet potato |
| Other treats | Commercially available hypoallergenic/hydrolysed protein therapeutic treats |
Additional diet trials may be required
Using the complete patient assessment including prior diet history, physical examination and diagnostic workup, an appropriate diet for a diet trial can be chosen, but multiple trials are required to identify the diet a patient responds to best. As a result, it is important to set owner expectations in the beginning and provide education that multiple diet trials may be required. Diet change was identified as key in the remission of clinical signs for patients with refractory protein-losing enteropathy using a combination of diet trials and immunosuppressive therapies, meaning that performing several diet trials is often beneficial (Wennogle et al, 2021). For some patients, it may be necessary to focus on resolving one or a few urgent clinical signs as the priority, such as first resolving vomiting and stopping weight loss. Then, as a second goal, addressing other clinical signs can follow (eg working on improving stool quality by adding fibre supplementation). Many patients will achieve a reduction in the frequency or severity of clinical signs with the combination of nutritional and medical interventions, but it is important to educate owners that the dog or cat is not ‘cured’ and will likely have periodic ‘flares’ which may even require some medical support. Keeping clinical signs mild or avoiding hospitalisation may be consistent with a significant clinical improvement.
Feeding management
As each pet is an individual, evaluating the pet's environment and optimising feeding practices may also help to improve diet trial outcomes. Effort should be made to create a stress-free feeding environment without any competition from other pets in the household. Changing food bowls or using disposable dishes and changing feeding location to a quiet area may also help address negative food associations for some patients (Delaney, 2006; Taylor et al, 2022). Some pets prefer foods served at body temperature, while others will eat colder or warmer foods. Each option should be tried for that individual. Increasing feeding frequency is also helpful for some patients with variable appetites (Delaney, 2006). While behavioural causes may play a role in picky eating, it is important to assume that a medical cause is likely to be present first and pursue proper diagnostics to identify best medical management along with the nutrition plan.
Appetite support
A common symptom of chronic enteropathy is reduced or variable appetite. Optimising medical management of concurrent disease conditions and using medications to support appetite is appropriate. While diet change to address the underlying disease process may improve appetites rather quickly, many patients will require medication support to improve appetite either temporarily or long-term. The patient should be evaluated to determine if the addition of pharmacological therapy for appetite stimulation or gastrointestinal bleeding is warranted. Providing medical support early may help avoid the development of negative food associations that can occur when continually offering various foods while the patient is hospitalised or feeling unwell.
For very picky eaters, the authors may strategically use additional foods in limited quantity as toppers or palatants that are carefully chosen to be compliant with the diet trial (same animal protein or carbohydrate source, same macronutrient targets). Amounts are limited to within the patient's treat allowance calories (no more than 10% of the calculated daily calorie intake) to avoid unbalancing the daily diet. It is important to note that home-prepared diets are not always the solution to picky eaters and in many cases, it is difficult to achieve a complete and balanced diet with home-prepared recipes for those patients with appetite challenges.
If picky eating is persistent, these patients may commonly reject individual foods or supplements required to achieve a balanced diet. Feeding an unbalanced homemade diet is not a long-term solution, so some patients must return to a commercial diet option to achieve a balanced diet, or assisted feeding may be indicated.
Assisted feeding
Assessing a patient's current food intake pattern, severity of symptoms (vomiting/diarrhoea), body condition score, muscle condition score, presence of weight loss, laboratory abnormalities (serum total protein, albumin, globulin, cholesterol, magnesium, calcium, levels of liver enzymes) and expected course of illness is helpful when assessing risk or presence of malnutrition and developing the individual nutrition plan. For cats, anorexia lasting anywhere from 2–14 days has been associated with hepatic lipidosis in the clinical setting (Valtolina and Favier, 2017). In the authors' experience, chronic enteropathy may have variable effects on appetite. It is important to assess a patient's current nutritional status when designing a nutrition plan and picky eaters should not simply be offered new diets when food intakes are extremely low. In general, if a patient is falling under 80% of calculated calorie needs for 3 days or more, assisted feeding should be considered (Chan, 2020). It is important to note that this timeline starts on the first day the patient stops eating and may begin before presentation in the clinical setting. For critically ill patients, hydration and electrolyte abnormalities should be addressed before starting a nutrition plan to decrease risks of complications of assisted feeding (Preiser et al, 2015). Using the gastrointestinal tract to provide enteral nutrition via a naso-oesophageal, oesophageal, gastrostomy or jejunostomy feeding tube is preferred whenever possible and monitoring for refeeding syndrome is important for patients with prolonged anorexia (Khoo et al, 2019). A comprehensive review of assisted feeding guidelines is available elsewhere (Brunetto et al, 2010; Chan, 2020).
Conclusions
Nutritional management of patients with chronic enteropathies can improve clinical signs in 50–66% of cases. Diet selection for these patients can be made in a thoughtful manner by evaluating clinical signs, physical examination and laboratory data, identifying the involved segments of the gastrointestinal tract and using a thorough diet history including reviewing ingredient exposures and macronutrient data. Client education is essential to setting expectations for duration and possible number of required feeding trials, as well as potentially expected improvements. Diet options for feeding trials may be commercial diets (dry food, canned or fresh diets) or home- or custom-prepared recipes. Often, multiple diet trials are required to achieve the best responses. A positive clinical response may be characterised by a reduction in some or most of the clinical signs; however, the patient is usually not ‘cured’ of all symptoms and ongoing monitoring is needed. For patients with poor appetites, it is very important to consider assisted feeding early in the treatment plan rather than pursuing multiple diet trials because of the serious consequences of malnutrition.
KEY POINTS
- Thorough nutritional assessment and creation of a nutrition plan for a patient includes collection of a detailed diet history, thorough physical examination and evaluation of diagnostic findings.
- Localising the part of the gastrointestinal tract involved and identifying key nutrients of concern are essential steps when designing the appropriate nutrition plan for a patient.
- Diet trials must last at least 8–12 weeks, with clinical improvements in gastrointestinal signs expected within the first 2–3 weeks of feeding the new diet.
- Multiple diet trials may be required to identify a macronutrient profile and ingredient list that works for each individual patient.
- For patients with hyporexia or variable appetites, optimal medical management is essential to supporting appetite and increasing compliance with new diets. Use of appetite support medications should always be considered.
- For patients with persistently poor appetites, assisting feeding should be considered early in the management plan.


