An emergency assessment focuses on evaluation of the three major body systems: cardiovascular, respiratory and neurological. The assessment aims to identify and prioritise problems and determine the urgency of the treatment required, without exacerbating any issues present. Cats are solitary creatures and have a high preservation reflex, often masking signs of illness until their condition has advanced. Therefore, cats can present with subtle derangements which may be easily overlooked on initial assessment.
Cardiovascular assessment and management
The purpose of the cardiovascular triage is to assess perfusion parameters. Identification of abnormalities allows determination of the presence and severity of shock. Shock is defined as the reduction in oxygen delivery and/or oxygen use by cells (Porter et al, 2013). There are six physical parameters that should be assessed in order to determine whether an animal is in shock (Reineke, 2015):
Most abnormal physical examination findings are the result of activation of the sympathetic nervous system in response to reduction in effective circulatory volume. Catecholamine release (adrenaline or noradrenaline) in response to activation of the sympathetic nervous system is responsible for the classic signs of shock; tachycardia, hyperdynamic pulses and peripheral vasoconstriction, causing the mucous membranes to be pale and the capillary refill time prolonged. This response is mediated by both activation of pressure receptors (baroreceptors) and chemosensors (chemoreceptors) in the major vessels. Cats are very sensitive to hypotension, but unlike dogs, where the sympathetic nervous system predominates in shock, cats have vagal fibres in close proximity to sympathetic fibres, both of which can be stimulated by reduced effective circulating volume (Mandell and King, 1998; Holowaychuk and Martin, 2006). The parasympathetic nervous system, mediated by the vagus nerve, is activated and this vagal response may blunt any compensatory tachycardic response to shock (Schwartz et al, 1973). As a result, many cats presenting with shock actually have a normal-to-low heart rate, which weakens the patient's compensatory response (Day, 2003). Clinical signs associated with shock are more subtle and include signs compatible with tissue hypoperfusion – for example, impaired mentation secondary to cerebral hypoperfusion and hypothermia (de Laforcade and Silverstein, 2015). Hypothermia may also contribute to further lowering of the heart rate. Absence of peripheral pulses (carpal and metatarsal pulses) can be supportive of a diagnosis of hypotension, but peripheral pulse palpation can be difficult in cats and care should be taken not to over-interpret these findings in isolation (Reineke et al, 2016).
Cardiac causes of hypoperfusion are not uncommon in cats and can include cardiomyopathies and valvular disease (Boag and Hughes, 2005). In comparison with dogs, cats can frequently present with a history that is not necessarily compatible with cardiorespiratory disease, with symptoms such as coughing less commonly recognised by the owner or potentially associated with retching or furballs (Beatty and Barrs, 2010). The presence of a murmur or gallop rhythm may suggest that the cat has underlying cardiac disease; however, cats with congestive heart failure are less likely to have a murmur than asymptomatic cats with hypertrophic cardiomyopathy, and the presence of a murmur cannot be used in isolation to reliably detect cardiac disease (Payne et al, 2010; Dickson et al, 2018).
A blood pressure reading should be taken in all cats with clinical signs compatible with shock. Direct blood pressure via placement of an arterial catheter is the gold standard for blood pressure measurement, as non-invasive methods have shown to correlate poorly with direct measurement in cats under anaesthesia (da Cunha et al, 2014). Practically it is difficult to place arterial catheters in awake, critically ill cats. These difficulties, along with the risks associated with arterial catheter placement in small patients including haemorrhage and ischaemic injury, mean that non-invasive methods of measurement are the mainstay of blood pressure assessment in cats in the emergency setting (Summerfield, 2019).
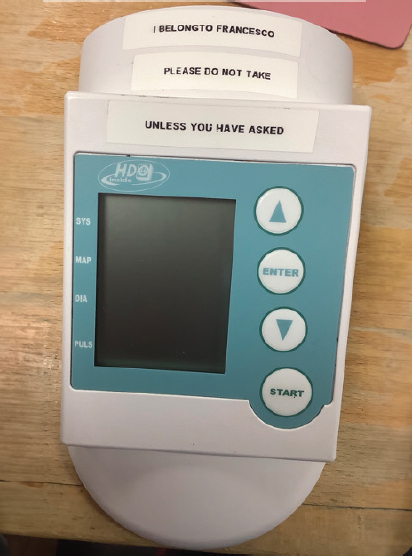
In light of their small size, Doppler blood pressure measurement (Figure 1) or the use of high-definition oscillometric devices (Figure 2) are preferred over traditional automated oscillometric devices as a result of the latter's inaccuracy in small patients (Boag and Hughes, 2005). A Doppler ultrasound device only detects one blood pressure measurement, and this value is usually considered to be closer to the mean arterial pressure than the systolic blood pressure in cats (Grandy et al, 1992). The high-definition oscillometric devices are the only monitor validated for use in awake, healthy cats (Martel et al, 2013). These devices have not been validated on a population of critically ill cats, so it is best to monitor the trends in blood pressure measurement rather than absolute numbers, and always interpret the result in light of clinical examination. Documenting the device used as well as the limb and cuff size used is important to ensure consistency in measurement and validity of the blood pressure trends observed, as is selection of an appropriate size cuff, which should have a width of 30–40% of the limb circumference. Studies have suggested that Doppler measurements have the highest correlation to direct arterial blood pressure measurements when the hind limb is used (Haberman et al, 2004; Skelding and Valverde, 2020). Different measurement techniques should not be used interchangeably in one patient because of the variability in reliability between devices, which could lead to inaccurate interpretation of readings and trends (Cerna et al, 2020).

Early vascular access is important in the cardiovascularly unstable cat, but this can be challenging in the species when in shock as a result of their small size. The medial saphenous vein is the easiest vein to cannulate in hypovolemic cats (Figure 3), but this site can be challenging to maintain. Blood sampling at the time of cannulation can help determine the cause and severity of shock. Key biochemical parameters, electrolytes and metabolites to measure include (Pachtinger, 2013):

Because of their small size and lower blood volume than dogs (60 ml/kg in cats vs 90 ml/kg in dogs), cats are at higher risk of developing clinically significant anaemia during critical illness and the minimum volume should be taken when drawing blood (Lynch et al, 2016). Retrieving a minimum database only requires 0.3 ml of blood, and this can usually be obtained from the intravenous cannula at the time of placement. Additional emergency assessment of the cardiovascularly unstable cat often involves point-of-care ultrasound, which relies on application of surgical spirit to the skin in place of clipping. Care should be taken to limit the amount of surgical spirit to the cat as this can worsen hypothermia, and proactive placement of a heat mat or blanket under the cat is recommended to prevent further heat loss (Isaza et al, 2021).
Temperature monitoring is crucial in an unstable cat, as hypothermia secondary to critical illness or injury has significant metabolic affects and leads to reduction of cerebral blood flow (Oncken et al, 2001; Brodeur et al, 2017). Repeated rectal temperature measurement may not be tolerated and can cause undue stress. A rectal probe could be placed in the recumbent cat after initial assessment. Failing that, axillary or tympanic membrane temperature measurement can be substitutes to rectal temperature. Axillary temperature is generally the best tolerated in conscious cats; however, the rectal–axillary temperature difference increases with obesity (Smith et al, 2015). The potential differences in rectal, tympanic and axillary temperatures can lead to pyrexia and hypothermia being missed in some cases. Therefore, as with blood pressure, techniques should not be used interchangeably and trends in axillary and tympanic temperature are more useful (Smith et al, 2015; Girod et al, 2016).
Respiratory assessment and management
Cats presenting with respiratory compromise are extremely fragile and particularly difficult to manage. They may appear apparently stable on distant examination but can quickly decompensate with excessive handling (Reineke, 2015). In some situations, the cause of the respiratory distress will be obvious, for example in the case of traumatic injury; however, in some cases it may be more difficult to identify. As the specific treatment will depend upon the underlying cause of the respiratory distress and timely intervention is fundamental to successful management, an appropriate assessment is essential.
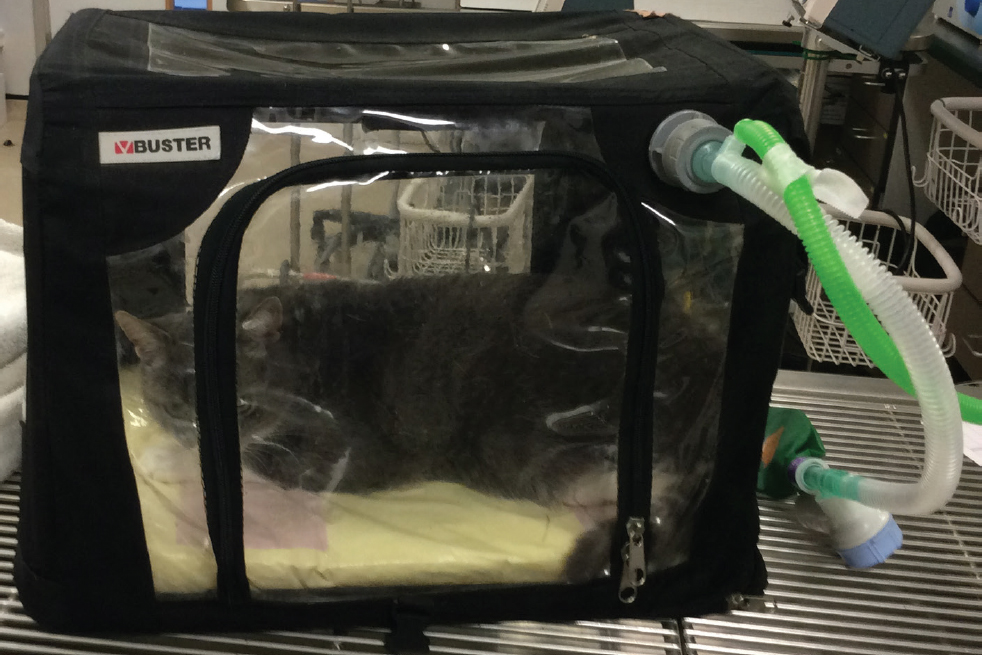
Assessment of the respiratory system is comprised of evaluation of respiratory rate, effort and pattern. Thoracic auscultation should also be performed to allow the cause of the respiratory distress to be localised to the upper airway, lower airway, parenchyma or pleural space. The initial respiratory assessment should be interpreted with caution as stress has a significant impact on respiration; open mouth breathing with respiratory rates of more than 100 breaths/minute have been reported in healthy cats on initial examination, and respiratory rate alone does not reliably identify respiratory disease (Sigrist et al, 2011; Dijkstra et al, 2018). The respiratory rate and effort of a cat are best performed at a distance when the cat is settled. It is recommended after the initial ‘hands-on’ major body system assessment, the cat is placed in a quiet kennel to minimise stress, with a non-invasive source of oxygen supplementation, such as a commercial oxygen cage or tent (Tseng and Waddell, 2000) (Figures 4 and 5). Continuous, remote monitoring can then be carried out to identify any change or deterioration in respiration; any decline in respiratory function can rapidly become fatal and so early identification is key.

It may be necessary to stage treatments for patients with respiratory compromise. As mentioned, handling can cause rapid deterioration and performing treatments in stages can allow the patient to maintain adequate respiratory function. Flow-by oxygen should be provided at all times during handling and treatment for respiratory support (Waddell and King, 2018) (Figure 6). Oxygen masks should be avoided as they are generally poorly tolerated in cats and cause significant stress, increasing oxygen demand in an already compromised patient.

Neurological assessment and management
Neurological assessment is reliant on assessment of mentation, ambulation and reflexes. As impaired mentation is one of the major clinical findings in cats with shock resulting from cerebral hypoperfusion (Holowaychuk, 2018), care should be taken in over-interpreting the neurological exam before the cat is cardiovascularly stable (Garosi and Adamantos, 2011). Treatment should be directed towards metabolic stabilisation (Knipe, 2015) including fluid therapy and warming to allow for a more accurate assessment of the neurological status.
Head trauma is a common emergency presentation in cats, and the main objective of head trauma management is the prevention and minimisation of secondary brain injury. Treatment priorities should be to rapidly reverse hypovolaemia and hypotension to maintain cerebral perfusion, and to avoid increased intracranial pressure, as this will exacerbate secondary injury (Kuo et al, 2018). An increase in intracranial pressure can lead to ongoing deterioration in cardiovascular and respiratory function (Sande and West, 2010). A combination of hypertension and bradycardia with an associated decreased mentation indicates a potentially life-threat-ening increase in intracranial pressure (Farry and Norkus, 2019). Objective neurological scoring systems, such as the Modified Glasgow Coma Scale, can be used as both a monitoring and prognostic tool. The Modified Glasgow Coma Scale involves assessment of level of consciousness, motor activity and brain stem reflexes, including pupil size and reactivity (Cameron et al, 2022). Ocular reflexes including pupillary light reflexes are difficult to assess in cats, particularly those receiving opioids and therefore the overall score should be interpreted in light of this (Pachtinger, 2013).
In addition to patient comfort and welfare, analgesic therapy is essential in minimising intracranial pressure. Cerebral metabolic rate, and therefore cerebral blood flow, blood volume and consequently intracranial pressure, is increased by pain and anxiety (Garosi and Adamantos, 2011). However, pain scoring using objective pain scales should also be interpreted with caution in cats. A large part of the two composite measure pain scales validated in cats involve hands-on assessment, and both can produce unreliable results in cats that are particularly aggressive, shy or afraid (Steagall and Monterro, 2019). The Feline Grimace Scale is a validated pain scale that relies on observation of facial changes and does not require handling of the patient, so may be better at detecting subtle changes indicating pain in cats (Figure 7). Reliability of pain scores can be improved by ensuring that the assessment is consistently performed by the same person. This reduces user variability and allows for detection of subtle changes in behaviour; pain can lead to the loss of normal behaviours such as grooming and resting, and the development of abnormal behaviours including aggression and vocalisation (Robertson, 2018).

Conclusions
Emergency assessment and management of cats provides additional challenges. However, having a better understanding of how feline behaviour and physiology may affect clinical manifestations of their condition will help better appraise their clinical findings and allow a more streamlined and stress-free approach.


