Behavioural medication is certainly not necessary or appropriate for every animal showing problem behaviour. Some behaviours perceived to be problematic by owners, such as chasing, digging and marking-related behaviours such as cats scratching furniture, can be normal species-specific behaviours associated with a positive emotional response. These behaviours will generally respond well to management and the provision of more appropriate outlets for these behaviours (Overall, 2013). Even where a problem behaviour is associated with distress or a negative emotional response, if the context and triggers are predictable and avoidable an animal may also respond to environmental management and behavioural modification, without medication.
Medication is most likely to be useful in cases where:
- An animal will be unavoidably exposed to specific situations that will cause them to become distressed. These will vary, but can include car travel, visits to the groomer, vet visits in general or particular handling procedures during examination, and exposure to loud noises such as fireworks. Repeated exposure to situations that cause distress is likely to increase the animal's fearfulness over time (Overall, 2013). In some situations, animals may learn to use avoidance and/or aggressive behaviours, making handling increasingly difficult (Riemer et al, 2021). Appropriate medication can prevent the escalation of fearfulness and distress, but this approach should always be supported by a behaviour modification plan aimed at teaching the animal to be more comfortable in those situations.
- An animal is experiencing chronic stress and it is not possible to completely reduce or avoid their exposure to problem triggers. If not addressed, this will negatively affect both an animal's physical health and mental wellbeing (Notari, 2009). Medication can improve tolerance of stress generally and also improve tolerance of problem triggers, although this must also be used alongside a comprehensive environmental and behaviour modification plan.
- An animal is experiencing high levels of emotional arousal. As well as resulting in problematic behaviour, high levels of arousal will interfere with learning and can make it very difficult to make progress with behavioural modification (Notari, 2009; Overall, 2013). Medication can potentially help lower arousal and improve an animal's response to a behaviour modification plan.
- A more rapid response to behaviour modification is needed. Medication can potentially speed up an animal's response to a behaviour modification plan (Crowell-Davies and Landsberg, 2009; Overall, 2013). This may be particularly important in situations where there are time pressures, for example where owners are having to consider euthanasia or where a council noise abatement order has been issued.
Important considerations before prescribing behavioural medication
Medical problems
Medical problems are a very common cause of behaviour changes in dogs and cats (Camps et al, 2019) and it is important to identify or rule this out as a cause of problem behaviour. For example. pain can cause or exacerbate a wide variety of problem behaviours including aggression, abnormal repetitive behaviours, anxiety and fearfulness (Mills et al, 2020). In many cases, a change in behaviour may be the only obvious sign of an underlying medical problem. It is therefore essential that any animal presenting with a new problem behaviour, or a change in an existing problem behaviour, receives a thorough health check before referral to a behaviourist, and before the use of behavioural medication is considered. This is important primarily to ensure the welfare of the patient, as starting behavioural medication may delay their access to more appropriate treatments such as pain relief. In addition, behavioural therapy is less likely to be effective if an underlying, undiagnosed medical condition is present. It is also important to rule out the presence of medical conditions that might cause particular drugs to be contraindicated, especially before the use of longer-term medication. The presence of a medical condition does not necessarily preclude the use of behaviourally-active medication, but it is important that any medical condition that could be contributing to a problem behaviour is recognised and addressed before treatment with behaviourally-active medication is begun.
Behavioural assessment
A behavioural assessment should provide a good understanding of what behaviour is being shown by the animal and why. It should include a thorough assessment of the contexts in which the problem behaviour is shown, the animal's motivation(s) for showing the behaviour and the emotion(s) underlying it, including the degree of emotional arousal (Mills, 2017). An accurate behavioural assessment will increase the likelihood of successful resolution of the problem behaviour. This can also inform selection of the most appropriate behavioural medication, as some medications are more suited to treating particular emotional states and higher or lower levels of emotional arousal. Unless the veterinarian is also a behaviour specialist, this behavioural assessment will need to be made by a behaviourist.
Comprehensive behaviour modification plan in place
Behavioural medication alone is unlikely to resolve problem behaviour. It is much more likely to be successful if used as part of a comprehensive behaviour modification programme that includes general stress-reduction strategies, reducing exposure to problem triggers, provision of appropriate outlets for normal behaviours and, where appropriate, changing the animal's emotional response to specific stimuli or situations. The role of behavioural medication is to reduce stress associated with negative emotional states and to reduce high levels of emotional arousal. This will improve the animal's welfare and in the case of longer-term medication it will also augment the behavioural modification plan by improving the animal's ability to learn more appropriate behaviours.
Medication selection
There are several factors that need to be considered when choosing behavioural medication. These fall into three separate categories: legal constraints, considerations relating to the problem behaviour being shown and considerations associated with the individual animal.
Legal constraints
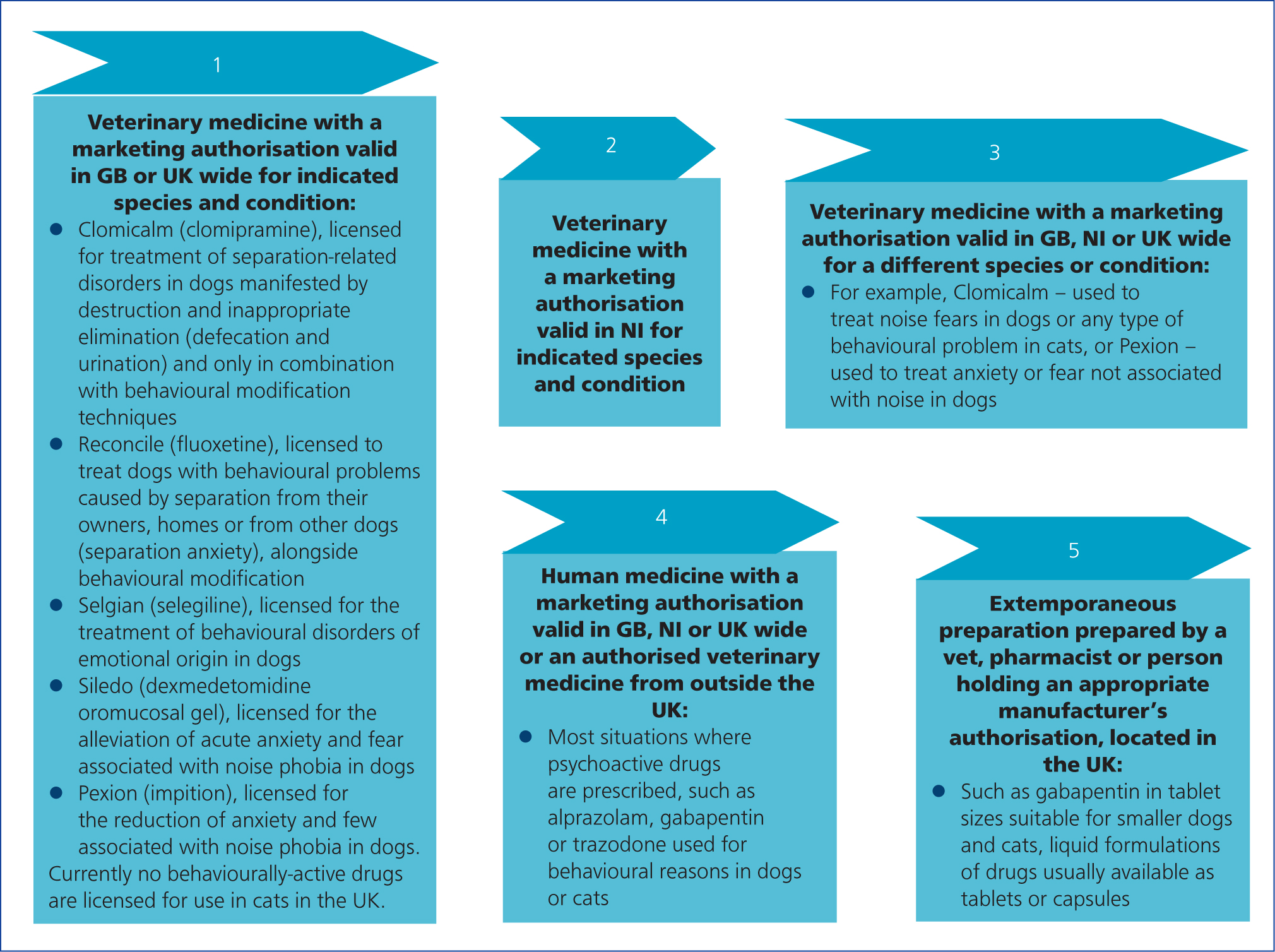
Like many drugs used in veterinary practice, most behaviourally active drugs are prescription only medications and must be prescribed by a veterinary surgeon according to the Veterinary Medicines Directorate (VMD, 2021) prescribing cascade. However, there are some particular issues with regard to the prescription of behaviourally active drugs.
There are very few behaviourally-active drugs licensed for use in dogs in the UK, and none at all for cats. In many cases, the terms of the license for a drug are fairly narrow, and are often associated with specific behavioural presentations. For example, the tricyclic antidepressant clomipramine is licensed in the UK, as Clomicalm (Elanco) for ‘treatment of separation-related disorders in dogs manifested by destruction and inappropriate elimination (defaecation and urination) and only in combination with behavioural modification techniques’. However, in practice, no one drug is particularly suited to treating one specific behavioural presentation such as aggressive behaviour, separation-related distress or noise-fear. This is because the behavioural presentation is not the ‘problem’ in itself, but the manifestation of an underlying emotional state such as fearfulness, anxiety or even frustration. Behaviourally-active drugs vary in their efficacy in terms of reducing these states, and there are significant variations in effect between individual animals, as seen in people (Preskorn, 2014).
The monoamine oxidase inhibitor selegiline (Selgian) has a much broader licence in the UK, for ‘the treatment of behavioural disorders of emotional origin in dogs’. However, its mode of action, mainly increasing dopamine with a stimulating, arousal-increasing effect, means it is not suitable for all individuals and all types of problem behaviours.
There are significant variations between different countries regarding the terms and licensing of behavioural drugs. As an example, fluoxetine has been licensed for the treatment of separation anxiety in dogs in both the USA and the European Union for some time, but has only recently been approved for use in the UK, as Reconcile (Forte Healthcare). While selegiline has a relatively broad behavioural license in the UK and EU, in the USA it is licensed specifically for the treatment of canine cognitive dysfunction.
This means that the drug highest on the VMD prescribing cascade may not necessarily be the one most suited to treating a specific problem behaviour in an individual animal. The most sensible approach is to choose a licensed option initially, if one is available for that particular behavioural presentation (for example there are a couple of licensed drug options, Sileo (dexmedetomidine oromucosal gel) and Pexion (imepitoin), for treating noise-related fears). However if the licensed drug is not sufficiently effective, or if there is a valid reason not to choose the licensed option for an individual animal, for example because of potential medical contraindications or behavioural concerns, a drug lower on the cascade can be used as long as there is good published clinical evidence available for its efficacy to treat that particular type of behavioural problem. In practice most behaviourally-active drugs are prescribed at level 3 or 4 of the prescribing cascade (Figure 1).
Considerations relating to the problem behaviour being shown
The most important considerations are the type of emotional response(s) believed to be underlying the problem behaviour, the degree of emotional arousal and how frequently the animal is exposed to the triggers or situations that cause the problem behaviour.
Accurately assessing the underlying emotional state of an animal is central to addressing problem behaviour (Mills, 2017). This will also help to inform the choice of medication. Vets without specialist behavioural knowledge will benefit from working alongside a suitably-qualified behaviourist who can assess the animal's underlying emotional state as accurately as possible.
The drugs most commonly used to treat behavioural disorders associated with underlying negative emotional responses, such as fear, anxiety or frustration, are listed in Tables 1 and 2.
Table 1. Short-acting behaviourally active drugs most commonly used in dogs and cats in the UK Class
| Class | Drug | Main mode of action | Behavioural conditions most suitable for | Approx time to onset of effect | Approx length of activity | Most common side effects | Dose ranges and dosing information |
|---|---|---|---|---|---|---|---|
| Benzodiazepines | Alprazolam | Binds to GABAA receptors. Reduces anxiety and panic. Can be sedative at higher doses | Short-term reduction of fears and phobias in dogs. Used less frequently in cats as other drugs such as gabapentin appear more effective | 30-45 minutes | 4 hours |
|
Dog: 0.01-0.1 mg/kg Cat: 0.125-0.25 mg/cat (trial and error may be needed to find most effective dose) |
| Diazepam | Binds to GABAA receptors. Reduces anxiety and panic. Can be sedative at higher doses | Short-term reduction of fears and phobias in dogs such as firework fears or car travel | 45-60 minutes | Up to 6 hours |
|
Dog: 0.5-2 mg/kg (trial and error may be needed to find most effective dose)Cat: 0.2-0.4 mg/kg per os every 8 hours | |
| Other anticonvulsant drugs with sedative/anxiolytic effects | Gabapentin | Inhibits release of various excitatory transmitters including glutamate, noradrenaline and substance P. Does not bind to GABAA receptors but increases GABA activity indirectly | Short-term sedation and reduction of fear and anxiety in dogs and cats. Can be effective when used alone in cats to reduce fear of vet visits and car travel. May need to be supplemented by other medications in dogs | 1-2 hours | 6-8 hours |
|
Dog: 10-20 mg/kg as single doseCat: 50-100 mg/cat as single doseFor very fearful animals, a dose can be given the evening before a trigger event and a second dose 1-2 hours before the event.Absorbed best on an empty stomach |
| Pexion (Imepitoin) | Low affinity partial, agonist of the benzodiazepine binding site on the GABAA receptor, plus weak calcium-channel blocking activity | Licensed in UK for the reduction of anxiety and fear associated with noise phobia in dogs | 2-3 hours | 12 hours |
|
Dogs: For short-term dosing give 30 mg/kg every 12 hours starting 2 days before a trigger event and continue through the event. Absorbed best on an empty stomach | |
| α2 adrenergic agonists | Sileo (Dexmedetomidine oro-mucosal gel) | Selective α2 adrenoceptor agonist, reduces activation of locus coeruleus in response to stressors or threats. Low dose via oromucosal route should reduce anxiety without causing sedation or cardiovascular effects | Licensed in UK for short-term treatment of noise aversion in dogs.Potential to be useful in other situations, such as vet visits, car travel or grooming | 30-60 minutes | 2-3 hours. Can repeat up to five times if needed |
|
Dog: 125 micrograms/m2 administered onto the oral mucosa between the dog's cheek and gum (use dosing guide in pack or data sheet) |
| Clonidine | Non-selective centrally acting α2-adrenergic agonist. | Reduction of high arousal and panic: generally used as add-on agent in dogs on longerterm medications such as tricyclic antidepressants or serotonin re-uptake inhibitors | 1-2 hours | Around 8 hours |
|
Dog: 0.01-0.05 mg/kg, can be used as needed (given 1-2 hours before exposure to trigger) or every 8-12 hours. | |
| Serotonin antagonist and reuptake Inhibitors | Trazodone | Increases serotonin activity. Also blocks histaminic and α1 adrenergic receptors | Short term anxiolytic and sedative effects, such as before vet visits, groomers, travel (dog and cat)NB studies suggest gabapentin may be more effective than trazodone for cats before travel, vet visits | 1 hour | 4-8 hours |
|
Dog: lower dose range 2-5 mg/kgHigher dose range: 10-14 mg/kgCat: 25-50 mg/catFor very fearful animals, give a dose the evening before a planned scary event and a second dose 1-2 hours before the event |
Adapted from Overall (2013); DePorter et al (2016); Ramsey (2017); Plumb (2018); Sinn (2018)
Table 2. Behaviourally active drugs used for longer term treatment in dogs and cats in the UK
| Class | Drug | Main mode of action | Behavioural conditions most suitable for | Most common side effects | Dose ranges |
|---|---|---|---|---|---|
| Tricyclic antidepressants | Clomipramine (Clomicalm, Novartis) | Increases activity of serotonin and noradrenaline. Blocks histaminic, cholinergic and α1 adrenergic receptors | Licensed in UK for treatment of separation anxiety in dogs. Has also been used successfully to treat a range of other fear and anxietyrelated problems including noise fears, generalised anxiety and compulsive behaviours | SedationAnticholinergic effects, such as dry mouth, constipation, urinary retention Can potentially increase arousal and reduce frustration tolerance as a result of its noradrenaline-increasing effect | Dogs: 1-2 mg/kg per os every 12 hours.Cats: 0.25-1 mg/kg per os every 24 hours |
| Specific serotonin reuptake inhibitors | Fluoxetine (Reconcile, Forte Healthcare Ltd) | Increases serotonin | Licensed in the UK* for the treatment of separation anxiety in dogs, in combination with behavioural therapy. Has been used successfully to treat a wide range of fear and anxietyrelated problems including noise fears, separation anxiety and generalised anxiety, as well as compulsive behaviours as it can reduce impulsivity | Reduced appetiteSedationPotential for gastrointestinal effects including diarrhoea and vomitingMay cause paradoxical increase in anxiety especially in early weeks of use | Dog: 1-2 mg/kg every 24 hoursCat: 0.5-1 mg/kg every 24 hours |
| Sertraline | Increases serotonin. Very weak effects on noradrenaline and dopamine | Similar to fluoxetine, may be slightly more effective at reducing panic | Similar to fluoxetine | Dog: 1-3 mg/kg every 24 hours | |
| Azapirones | Buspirone | Increases serotonin | Has been used successfully to treat a range of fear and anxiety disorders, particularly in cats. These include urine marking, stress-related inappropriate urination, social tension, timidity. May increase pro-social behaviour towards people and other cats | Generally well-tolerated but may cause paradoxical increase in anxiety, especially in early weeks of useHas been associated with increased aggression to other cats, so needs to be used with care in multi-cat households | Dog: 1-2 mg/kg every 8-12 hoursCat: 0.5-1 mg/kg every 8-12 hours |
| Serotonin antagonist and reuptake inhibitors | Trazodone | Increases serotonin activity. Also blocks histaminic and α1 adrenergic receptors | While mainly used for short-term anxiolytic and sedative effects, trazodone can also be used to treat chronic anxiety problems in dogs that have not responded to other medications. Generally used as an adjunct to other longer-term medication |
|
Dog: 2-12 mg/kg every 12 hoursRecommended to start on lower dose and increase gradually if necessary. For dogs on other serotoninincreasing medication, do not exceed maximum dose of 5mg/kg |
| Monoamine oxidase inhibitors | Selegiline | Small increases in monoamine neurotransmitters including serotonin and noradrenaline. Mainly increases dopamine. Metabolites include amphetamine and methamphetamine, both of which are stimulants | Licensed in UK for ‘treatment of behavioural disorders of purely emotional origin in dogs, such as depression and anxiety, and, in association with behaviour therapy, for the treatment of signs of emotional origin observed in behavioural conditions such as overactivity, separation problems, generalised phobia and unsocial behaviour”. Not licensed in cats. Generally indicated for animals with fear-related problems associated with hiding and withdrawal rather than those showing high levels of arousal and reactivity. Can also be helpful in animals with cognitive dysfunction and in animals experiencing severe grief-related responses |
|
Dog: 0.5-1 mg/kg per os every 24 hoursCat: 1 mg/kg per os every 24 hours Best dosed in morning because of its stimulant effect |
| Anticonvulsant drugs with anxiolytic effects | Imepitoin (Pexion) | Low affinity partial agonist of the benzodiazepine binding site on the GABAA receptor, plus weak calcium-channel blocking activity. | Licensed in UK for the reduction of anxiety and fear associated with noise phobia in dogs. May also be used in combination with a behaviour modification plan for the control of anxiety in dogs in relation to both social stimuli (such as crowds or strangers) and non-social stimuli (such as noises, novel items or new environments) |
|
Dogs: 10-30 mg/kg twice a dayAbsorbed best on an empty stomach |
| Gabapentin | Inhibits release of various excitatory transmitters including glutamate, noradrenaline and substance P. Does not bind to GABA receptors but increases GABA activity indirectly. | Generally used as an adjunct to other longer-term medication such as tricyclic antidepressants or specific serotonin reuptake inhibitors, Can be particularly useful in cases where behaviour is being exacerbated by chronic or neuropathic pain |
|
Dog: starting dose 10-20 mg/kg every 8-12 hours, increase gradually if needed Cats: starting dose 5-10 mg/kg per os every 8-12 hours, increasing gradually if neededAbsorbed best on an empty stomach. If given for a long period animal may develop tolerance and dose may need to be increased |
Based on information from many sources including Overall (2013); DePorter et al (2016); Ramsey (2017); Plumb (2018); Sinn (2018).
*Reconcile's official UK launch will be in November 2021.
These drugs work to reduce fear and anxiety, either by acting on GABAA receptors or on various monoamine neurotransmitter pathways including serotonin, noradrenaline and dopamine. They vary in their effectiveness in treating different presentations of anxiety and fearfulness, including phobias, panic responses and frustration. They also vary in how they affect arousal and activity levels, with some drugs having a calming, arousal-reducing effect and others increasing arousal and activity levels. These variations in effects are partly caused by differences in which neurotransmitters and neurotransmitter receptor sub-types they affect. There also appear to be significant individual variations in responses to different behaviourally-active drugs, possibly related to genetic differences in the number and distribution of specific neurotransmitter receptor sub-types and the various enzyme pathways by which individual drugs are metabolised (Preskorn, 2014).
There are two main types of behaviourally-active drugs: short-acting drugs, that can be used for treatment for specific problem events, and those that are more suited for long-term use. Where animals are exposed to problem triggers infrequently, short-acting drugs given when needed can work well. This is especially the case with predictable exposure to problem triggers, such as fireworks or car travel. Because of their rapid onset of effect, these drugs can also be given after an animal has been exposed to a problem trigger. However, it can be more difficult to dose a fearful animal and medication may be less effective at reducing fearfulness if given when the animal is already in a state of fear. Where animals are exposed to problem triggers or situations frequently and/or very unpredictably, longer-term medication given on a daily basis will be more appropriate.
Considerations associated with the individual animal
Before prescribing behaviourally-active medication for an animal, it is important to be aware of any potential medical contraindications for particular drugs. For example, the anticholinergic effects of the tricyclic antidepressant drug clomipramine can exacerbate constipation and urinary retention and can also cause heart arrhythmias, while specific serotonin re-uptake inhibitors such as fluoxetine can exacerbate bleeding problems associated with poor blood clotting. Most behaviourally-active drugs are metabolised by the liver, so may not be safe to use in animals with impaired hepatic function. There is also potential for adverse interactions with other medications. For example, clomipramine (Clomicalm) and fluoxetine can interfere with the availability of other medications, including some anti-epileptic drugs and thyroxine, which could potentially destabilise animals with epilepsy and thyroid disease. It is also important to be aware that some non-behavioural medications, such as tramadol, can increase serotonin levels and the subsequent risk of serotonin toxicity if an animal is also given a serotonin-increasing behaviourally-active drug. This is also the case if different classes of behaviourally-active medications are given together, particularly if the monoamine oxidase inhibitor selegiline (Selgian) is given alongside a serotonin-increasing drug such as Clomicalm or fluoxetine.
Short-acting behaviourally-active drugs
Short-acting fear and anxiety-reducing drugs tend to work by reducing activity in areas of the brain that trigger acute stress responses, particularly those associated with negative emotional responses such as fear, anxiety and panic. Their effects range from anxiety-reduction to sedation, and this is generally dose-related. They have a fairly rapid onset of action (sometimes less than an hour) and a relatively short half-life. They are most useful for reducing fear, anxiety or panic in response to triggers that are both predictable and relatively infrequent. They can be used alone, for isolated events or triggers, or alongside longer-term medication if additional help is needed for particularly triggering events. For example, to help a generally noise-phobic dog cope better over the firework period, or to help a dog that is worried about unfamiliar people cope better with being handled in a veterinary surgery. Table 1 outlines information about the activity and uses of some of the most commonly used short-acting behaviourally-active drugs in the UK.
Longer-term treatment of problem behaviours
Most of the drugs commonly used for the longer-term treatment of behaviour problems in cats and dogs were originally developed and used as antidepressants in humans. Most affect the activity of serotonin and some also affect noradrenaline and dopamine activity. Exactly how these drugs affect behaviour in the longer term is not yet fully understood (Sinn, 2018). They tend to improve mood, particularly through reducing negative emotional states such as fear and anxiety and have variable effects on arousal levels. They can also improve an animal's ability to learn, both indirectly through reducing stress and high arousal levels, and directly through encouraging long-term potentiation and the formation of new neural pathways, in part through increasing levels of brain-derived neurotrophic factor (Zhou et al, 2017).
Individual drugs, even within the same drug class, vary in their behavioural effects and side-effects as a result of variations in the neurotransmitter sub-types targeted and the different behavioural effects of their active metabolites, as well as the way these are metabolised by the animal. Table 2 outlines information about the activity and uses of some of the drugs most commonly used for the longer-term treatment of behaviour problems in cats and dogs in the UK.
Prescribing behaviourally-active medication in general practice
Animals with behaviour problems may be presented to a veterinary practice in several different ways. The owner may make an appointment specifically to discuss the problem behaviour with a vet or nurse, or problem behaviours may be mentioned during the course of other appointments (Roshier and McBride, 2013). In this case, the veterinary surgeon will need to assess whether the problem behaviour can be assessed and treated within the practice, depending on the level of expertise available, or whether it should be referred to a behaviourist. In other cases an owner may have approached a behaviourist first. If so, all reputable behaviourists will ask the owner to arrange a consultation with their veterinary surgeon before they see the animal to assess their behaviour, both to check the health status of the animal and arrange a formal referral.
All animals presenting with behavioural problems should receive a thorough health exam to rule out (or identify and treat) any obvious medical problems that might be causing or exacerbating the problem behaviour, before they are referred to or assessed by a behaviourist.
If there are no obvious health concerns the animal should be referred to a suitably qualified behaviourist. While this would ideally be an Royal College of Veterinary Surgeons (RCVS) recognised specialist or advanced practitioner in veterinary behavioural medicine, there are relatively few veterinary behavioural specialists available and most behavioural cases will be referred to a non-veterinary behaviourist. In the current absence of regulation in the behavioural industry it is important for the referring vet to ensure that this behaviourist is suitably qualified and capable of making an accurate behavioural assessment. Individuals listed on the Animal Behaviour and Training Council register of Clinical Animal Behaviourists and on the register of the Association for the Study of Animal Behaviour Certificated Clinical Animal Behaviourists have been independently assessed and proved competent. If referring to a non-veterinary behaviourist that is not on either of these registers, the referring vet must be aware of their responsibilities as outlined in the RCVS code of conduct guidance on referrals.
Even where a health problem has been identified as influencing behaviour, the animal may still benefit from referral to a behaviourist as they may be able to help address learned aspects of behaviour such as fear of handling or toileting problems that have occurred secondary to a painful condition. Animals with ongoing health problems should ideally be referred to a veterinary behaviourist. If referred to a non-veterinary behaviourist, the referring vet must retain overall responsibility for the case and continue to monitor and manage the medical aspects of the case, including pain.
If the behavioural assessment indicates that the animal might benefit from behavioural medication in addition to other behavioural support, the behaviourist should discuss this with the referring vet in the first instance.
Unless the animal has been referred to a veterinary behaviourist, the specific choice of drug should be made by the referring veterinary surgeon, based on consideration of the presenting problem behaviour, the availability of licensed drugs for that condition and any potential medical or drug-related contraindications. Information about individual drugs can be found in the drug data sheets and in publications such as the British Small Animal Veterinary Assocation small animal formulary or Plumb's Veterinary Drug Handbook. Ideally the most recent versions should be used to ensure the information is as up to date as possible. The referring vet will be responsible for any adverse side effects caused by the medication.
Behaviourally-active medications are likely to be prescribed according to the cascade shown in Figure 1 (VMD, 2021) as there are relatively few drugs licensed for treating behaviour problems in dogs (and none in cats). Where unlicensed drugs are chosen, in the absence of a licensed option or where the licensed option is not considered clinically suitable for that animal, this choice should be based on published evidence on the safety and efficacy of that drug in treating the specific behavioural condition in that species. As with other types of medication, owners will need to be informed and asked to sign a consent form when unlicensed drugs are prescribed.
Where a drug has a wide dose range, it is generally wise to start at the lower end of the range and increase the dose gradually if needed. There should be time, in most cases, to experiment with dosing of short-acting medication before planned events such as vet visits. However, where a procedure or scary event is unavoidable and unanticipated it may be necessary to use larger doses to ensure the animal is not overly distressed and remains sufficiently calm to be safely restrained.
In cases where vets are not confident prescribing behaviourally-active medication, or where a behaviour case appears particularly complex or is not responding as expected to behaviourally-active medication, consider referring the animal to a veterinary behaviourist with a good understanding of the use of psychoactive medication in small animals. This will include RCVS recognised specialists in behavioural medicine, RCVS recognised advanced practitioners in behavioural medicine or a veterinary behaviourist listed on the Animal Behaviour and Training Council website (https://abtc.org.uk/practitioners/)
Ongoing care of animals on longer-term behaviourally-active medication
When an animal has been prescribed behaviourally-active medication it is important for the vet and behaviourist to liaise regularly to discuss the animal's progress with the behaviour modification plan. This will help monitor any adverse physical or behavioural side effects and make it easier to identify whether any adjustments need to be made to the dose or to the type of drug, as well as informing decisions about when to withdraw medication.
When monitoring progress in animals on longer-term medication it is important to inform owners on how long an individual drug takes to become effective. For drugs such as Clomicalm and fluoxetine it can take 4-6 weeks, and up to 8 weeks for Selgian, to see any obvious behavioural improvement. It may also take 2–3 months before these drugs become fully effective. It is important that drugs are not stopped because they do not appear to be working, when they have not been given for long enough to become effective.
Unwanted side effects often become apparent in the earlier weeks of giving longer-term medication, often before the drugs have started to become effective behaviourally. The most common side effects are mild sedation, loss of appetite and mild gastrointestinal signs such as vomiting or diarrhoea. However, there are other potentially more serious side effects and it is important that vets and owners are aware of these. As long as any side effects are mild, it should be fine to continue giving the drug, as the side effects will generally reduce after a few weeks as the animal adjusts to the medication. In the case of appetite loss or mild gastrointestinal signs, it may help to reduce the drug dose by about a half for a week, then increase again. In the case of severe side effects the drug should be stopped altogether.
If the first choice of drug is not suitable, either as a result of lack of efficacy or side effects, then it should be stopped and another drug tried instead. In most cases it is best to withdraw the first drug gradually, as this can reduce the risk of withdrawal effects. Adverse withdrawal effects, such as increased anxiety and agitation, are more common in drugs with shorter half-lives and where animals have been on a particular drug for a longer period of time (Tondo et al, 2020). It may be necessary to stop a drug suddenly if it is causing severe adverse side effects. It is also wise to have a ‘wash-out’ period of 1–2 weeks off all medication before starting a second drug. This is particularly important when swapping between drugs of different classes that increase serotonin by different means, particularly between serotonin reuptake inhibitors such as clomipramine or fluoxetine and the monoamine oxidase inhibitor selegiline.
When an animal has responded well to medication and the behaviour modification plan, it may eventually be possible to stop giving the medication altogether. Again, it is sensible to do a very gradual withdrawal, tapering the drug over a number of weeks, as this will reduce the risk of withdrawal effect. If the animal's behaviour starts to deteriorate during the withdrawal it may be possible to identify the lowest effective dose for them to stay on longer term.
Conclusions
Behaviourally-active medication can play an important role in the treatment of behavioural problems in dogs and cats, especially where they are associated with a strong negative emotional response and high levels of arousal, as these negatively affect an animal's welfare and interfere with their ability to learn more appropriate behaviours. All vets in general practice should have a good working knowledge of the main principles of using psychopharmacology, including what drugs are available, their modes of action and any potential side effects or adverse interactions with comorbidities or other medications. Vets without specialist behavioural knowledge will benefit from working alongside suitably qualified behaviourists who can assess and address each animal's behaviour and emotional state. It may also be necessary to consider referral of cases with complex behavioural conditions or pharmacological requirements to a veterinary behaviourist.
KEY POINTS
- Behaviourally-active medication can play an important role in improving the welfare of cats and dogs in both the short and longer-term and can play an important role in the longer-term reduction of negative emotional states, particularly fear and anxiety, as long as they are used alongside a comprehensive behaviour modification plan.
- The choice of medication should be based on a sound behavioural assessment from a suitably qualified behaviourist, taking into account a number of factors including the animal's underlying emotional response and frequency of problem triggers.
- Before prescribing behaviourally-active medication, vets will need to consider any health problems or other medications the animal may be receiving that might make specific psychoactive drugs unsuitable for that individual.
- Longer-term psychoactive medication must always be used in conjunction with a behaviour treatment plan.
- Regular monitoring of both health and behaviour is important for animals on longer-term medication.

