Musculoskeletal problems are no less common in street dogs however identifying and managing them in these patients can be a real challenge where opportunities for examining and investigating findings can be limited. This presentation will concentrate on using history and physical examination to identify problems using common examples as illustration. Fortunately, there is no real substitute for these skills in this area so the challenge can be addressed adequately.
Investigating a musculoskeletal issue
This process can be considered in three phases:
- Stage 1: the moving dog
- Stage 2: the static dog
- Stage 3: the sedated or anaesthetised dog.
Before undertaking any physical examination it is very important to obtain a full account of the problem from the owner's viewpoint. In particular, to understand what they are seeing day-to-day and what is concerning them. Remember that the veterinary surgeon has a very short window of opportunity to examine the problem in the patient, while the owner is literally living with it. Their information is critical so it is important to ‘listen carefully’. During this conversation the dog and owner should be carefully assessed. For the dog, posture; the way it rises or sits; and temperament are key.
Stage 1: the moving dog
Observing the way the dog moves is vitally important, but space and circumstances can sometimes make this problematic. When time and space are limited, using a mobile phone camera to capture gait can be useful. It can be re-run without trying to get a dog to repeat movements. Similarly, if the owner has a mobile phone it is useful if they try to capture the movement that is concerning them, for later review.
In an ideal situation it is best if a set sequence is followed:
- Observe patient sitting, rising and standing
- Have the dog walked away from investigator. Observe from directly behind. Dog should be on a ‘loose’ lead and relaxed
- Dog turned and walked towards investigator. Observe from directly in front
- Repeat as necessary
- Move to affected side if possible and observe walk from side
- Repeat all at trot if necessary.
For each patient it is important to keep the objectives simple, looking to answer four simple questions:
- Is the dog lame?
- If so, is it front or back leg?
- Is it left or right?
- Could more than one leg be involved?
If you can answer these questions then this is all the information you need. The more severe the problem, the more obvious the abnormality.
Tips
- It is much easier to identify a forelimb lameness than a hindlimb. This is best seen with the dog walking/moving towards the investigator. Remember the head will dip as the SOUND leg lands as weight is placed on this leg. Pick one leg and every time it strikes the ground repeat in your head ‘down’ to pick up the rhythm of the walk and see if head is moving as it should.
- Hindleg lameness is more difficult and can also cause the head to nod. This is why it is best watching the animal walk away first, to establish any potential hindlimb issue before concentrating on forelimb. Classically, the rump should drop as the weight goes onto the respective hind leg.
- Hindleg lameness can be confirmed by observing movement, flexion and extension from the side
- Walk behind the dog mimicking the foot placement. Often you can ‘feel’ a lameness that is hard to see.
Stage 2: the static dog
Once again, a set sequence for examination should be developed and followed. This ensures that things are not missed. A great deal of information can be obtained by palpating the limbs and joints before they are actually moved. The logical sequence to use reflects that. In most dogs, with the exception of toy or small breeds, the examination is best conducted with the dog standing on the ground rather than being elevated. It is also important to let dogs know where you are as you move around them conducting the examination, much as you do with a horse. Keep a hand on the animal and get close contact during the examination, to maximise control.
- Assess the dog's temperament by approaching the dog from the front. Assess the ability of the handler (owner)
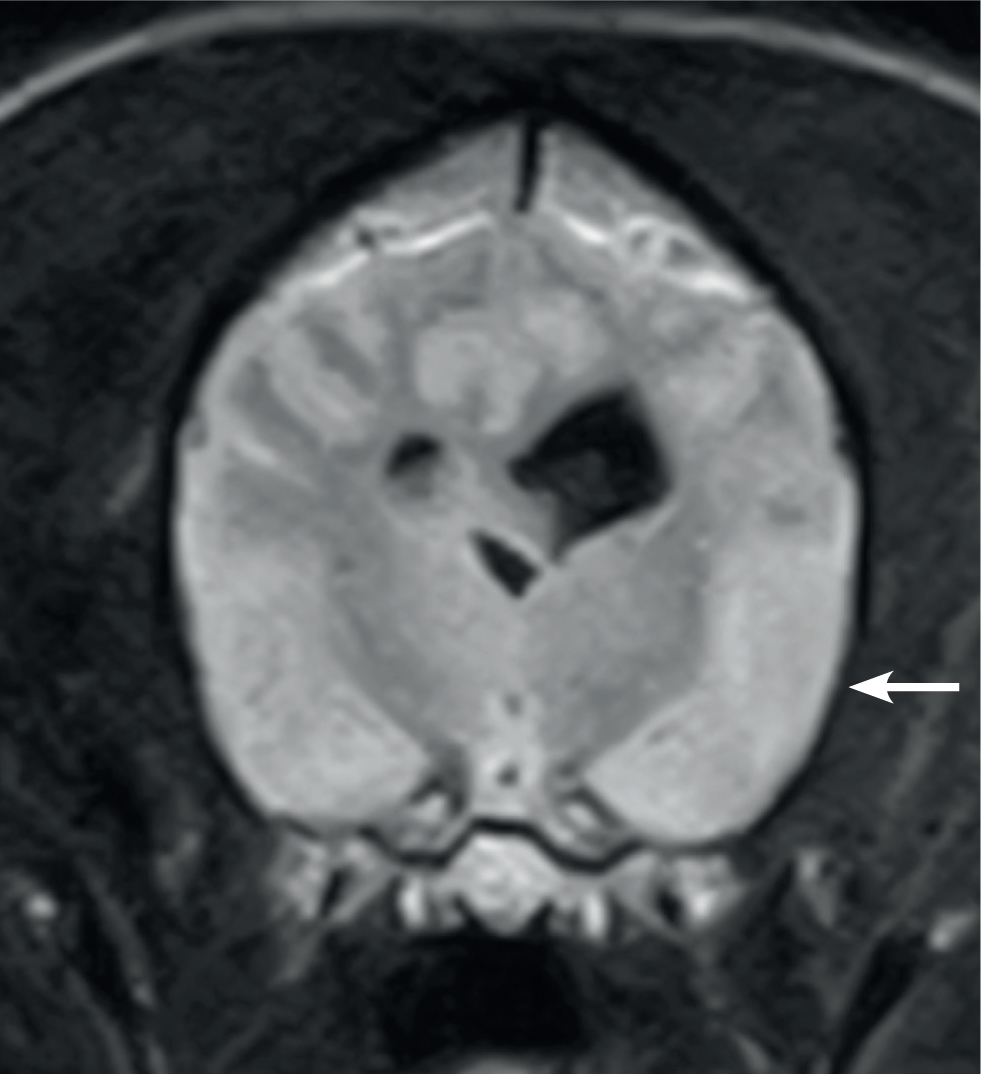
- Move to the back of dog and assess both hindlegs. Placing a knee between the hind legs to support the dog's weight can assist. Simultaneously, run hands from hip to foot on both legs feeling for lumps or bumps, and for muscle wastage (Figure 1)
- Move up the thoracic spine to examine forelimbs (I usually straddle the dog and grip it between my knees at this point)
- Again, working from shoulder to foot feel for any muscle or soft-tissue abnormalities
- Check the neck by moving the head from side to side, flexing and extending.
Next, moving the joints:
- Return to the hindlimbs and, starting from the foot and working up the leg, lift and flex and extend all the joints in sequence, finishing with the hip
- Conduct special tests for the stifle and hip joints
- When both sides are complete, extend both hips together
- Move to the front of the dog (sound side first). Starting from the toes, lift the leg and flex and extend all the joints in sequence.
It is always good practice to target a painful area as the last one to examine. Likewise, comparing one side to another is a good way of establishing whether there is an abnormality or not. If there is a suspected painful reaction then leave the area, continue the examination, then return to the suspicious area at the end of the examination to check if the same response occurs.
Specific tests for stability
It can be useful to perform part of the examination with the dog on its side. This is really of use when we are homing in on a particular area or joint. Sedation to relax the dog is also useful if trying to determine if there is joint instability, i.e. in the anterior drawer test. This option may be limited in a street examination.
Common conditions and findings
‘Common things are common’ and it is useful to have a very good working knowledge of the characteristic features of common disorders which may help in early recognition of these (Table 1).
Table 1. Common conditions and findings
| Condition | History | Clinical findings |
|---|---|---|
| Cruciate disease/rupture | Can vary. Often young large breedGradual onset limp that becomes persistentLittle evidence of pain reportedCan have distinctive sitting postureCan be acute onsetCan have bilateral problem | Unilateral lameness usuallyObvious atrophy of quadricepsFirm swelling on medial aspect of proximal tibiaPain on tibial thrust testInstability on anterior drawer/tibial thrust test |
| Hip dysplasia (HD) | Juvenile dogDifficulty rising/jumpingBunny hoppingBilateral lameness? | Pain on flexion and extensionInstability on hip lift testCrepitus occasionallyTight and painful hip adductors including pectineal muscles |
| Hip arthritis | Differentiate from HD by age: mature dogSigns as above. Difficulty rising or jumping Lameness | GaitInstability is not a featureReduced range of movement, in particular extension of hip Crepitus |
| Patellar luxation | May see in Boxers, Bulldogs, Bull Terriers and LabradorsYoung dogs typicallyLifting leg intermittentlyBowlegged gaitExercise intolerant | May be lameFind tibial crest and follow straight patella ligament to identify the patella: is it in groove?Can it be displaced?Is groove empty with patella displaced medially or laterally |
| Elbow dysplasia/arthritis | Can start to show problems from 5 months old onwardsIntermittent/persistent mild lameness usually, which may show occasional worse boutsOften bilateral gait problem | Lameness — usually one sideDiffuse swelling of elbow jointDiscomfort on forced extensionReduced total range of movement |
| Bone neoplasia | Larger breedsTypically older, but can occur in young animalsWorsening, persistent lameness | Typical sites: metaphyseal; proximal humerus/distal radius; distal femur/proximal and distal tibiaObvious lamenessMuscle atrophyCharacterised by severity and painIn distal limb, swelling palpable; in proximal limb, palpable with sedation |
Dealing with osteoarthritis in street dogs
Many street dogs will develop osteoarthritis (OA) in one or more joints as they get older. Early recognition of this will help with management.
There are many options to alleviate the pain and mobility problems associated with the disease. The main disadvantage in the street dog are the exclusion of more expensive options. The advantage is that we have an owner spending a great deal of time with the dog and able to help in other ways. A multimodal approach to managing the problem yields the best results over the long duration. It also provides an opportunity to customise the best combinations for particular circumstances.
Examples of how these options may be combined in street dogs is shown in Table 2.
Table 2. Multimodal approach to osteoarthritis treatment
| Multimodal target | Options | Clomment |
|---|---|---|
| Pain management | Any non-steroidal anti-inflammatory drug (NSAID)Paracetemol to augmentAcupuncture | Medical pain control can be achieved with NSAID and this can be combined with paracetamol in severe casesAcupuncture could be very useful in responsive cases as an alternative |
| Nutritional management | Keep bodyweight within normal limits | Although there are a great many nutritional options the most important thing is maintaining a normal bodyweight and avoiding obesity |
| Physical rehabilitation | Employ therapeutic exercises specific to the problem that owner can perform daily on dog | Work at maintaining mobility of affected joint(s) in first instance with additional exercises for muscle development and proprioception |
| Owner participation and education | Use simple instructive material to encourage understanding and participation | Give control of problem to the owner by providing clear plans and objectives |
| Local disease modification | None | The drive to produce and use products which can have a longer term benefit could really benefit street dogs in the future but there are no practical (or proven) alternatives right now |
Conclusions
Simplifying the understanding of OA and using ‘tools’ that suit the situation and the environment mean that street dogs suffering from painful OA can benefit and achieve an acceptable quality of life.

