The otitis externa roundtable was held as a virtual meeting on October 26 2020 and was sponsored by Elanco Animal Health. Its aim was to produce best practice guidelines for the diagnosis and treatment of a common condition that can present a major clinical challenge for veterinary staff.
Factors causing otitis externa: identification and management — Claudia Nett
Otitis is a very common condition in veterinary practice, occurring in 15–20% of all canine and 4–7% of feline patients. It is one of the most challenging and frustrating diseases for veterinarians and owners alike. It may become a chronic and very painful condition for the patient and its treatment and management can be costly. It is a multifactorial condition and treatment will need to be tailored to the specific case. Its management is based on the identification and correction of the various elements involved, known as PPSP (i.e. the Predisposing factors favouring the development of otitis, the Primary and Secondary factors causing the condition, and the Perpetuating factors preventing its resolution).
Predisposing factors
Predisposing factors increase the risk of otitis but do not cause the disease per se. These factors will only become significant in combination with a primary cause, but they do need to be taken into account for the long-term management of the condition. A significant predisposing factor can be the anatomical conformation of the dog's ear. The large, heavy ears of Bloodhounds that may block the ear canal is one example; the narrow ostium in Shar Peis is another, as this will close easily if inflammation is present. Meanwhile, in Cocker Spaniels, the combination of large ears and the number of ceruminous glands in the ear canal will predispose these dogs to more severe stenosis because of inflammation and hypertrophy of these glands.
Other predisposing factors include high temperature and humidity and an excessive discharge in the ear canal. Treatment may also become a factor if the medications used cause irritation or there is mechanical trauma through overvigorous cleaning or hair plucking in the ear. Owners of dogs with allergies should be advised to tell groomers to shave rather than pluck the hairs in the dog's ears. Tissues that cause obstruction of the ear canal, such as tumours or polyps, can also predispose the dog to otitis.
Primary and secondary factors
The primary factors that will induce otitis externa are the most important issues to address and are key to successful long-term management of these cases. These are the factors that change the microclimate of the ear and induce inflammation and infection.
The most important primary factor in canine otitis is allergy which is present in 70% of cases (Paterson and Matyskiewicz, 2018). This will often be a result of a food allergy, with otitis externa as the primary sign in 20% of food allergy cases, and the remainder showing otitis along with other cutaneous signs. Only 3–5% of cases of atopic dermatitis present with otitis externa alone, while 80–90% have both otitis externa and other cutaneous signs. Erythema is first visible in the skin around the ostium and spreads out as the disease progresses.
In some cases, dogs will be found to have contact dermatitis as a result of treatment with antibiotics such as neomycin or gentamycin, or with preparations containing silver sulfadiazine, propylene glycol, etc. In cases where there is no longer any evidence of bacteria or yeasts, then contact allergy should be considered as a possibility as a result of long-term contact with the agent concerned.
Some primary factors can be relatively easy to eliminate, such as parasitic mites (Otodectes cynotis, Demodex species, Notoedres cati and Sarcoptes scabiei), Trombiculidae spp., ticks and flies. O. cynotis is a common parasite in companion animals, present in 5–10% of dogs and 25–50% of cats with otitis externa (Scott et al, 2000). Dogs with floppy ears may be predisposed to becoming infected. There is also a high rate of asymptomatic carriers in both species (16% dogs and 11% cats) and further diagnostic tests may be needed to identify the parasites in these cases. While the use of isoxazolines or macrocyclic lactones in controlling ectoparasites in dogs and cats may reduce the prevalence of Otodectes in these species, the increasing numbers of clients committed to ‘natural’ products may have the opposite effect.


Another common primary factor is the presence of foreign bodies in the ear canal, such as grass seeds, hair, drug residues, ceruminolyths, sand particles and dirt. Grass seeds may have long bristles or awns that can penetrate deep into the ear canal and will need to be removed with forceps.
Other primary factors may include keratinisation defects (e.g. sebaceous adenitis, idiopathic seborrhoea, vitamin A-responsive dermatosis, zinc-responsive dermatosis), metabolic causes (hypothyroidism, Cushing's disease, sex hormone imbalances). Hypothyroidism cases tend to present with severe bacterial otitis without other common signs such as erythema or head shaking. If an elderly dog presents with Pseudomonas spp.-based bacterial otitis without a previous history of allergic dermatitis, hypothyroidism as primary factor should be high on the differential diagnosis list.
Autoimmune diseases that may be primary factors in otitis include juvenile cellulitis, pemphigus foliaceus, lupus erythematosus and erythema multiforme; while leishmaniosis and drug eruption may produce similar signs.
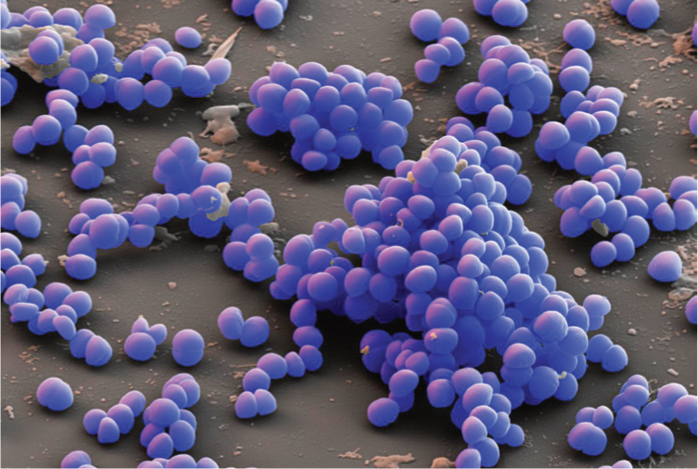
Secondary factors are those causing otitis in combination with the above predisposing factors, such as infections with yeasts (i.e. Malassezia spp.) or bacteria (Staphylococcus, Streptococcus, Pseudomonas spp.). One distinctive feature of Pseudomonas otitis cases is the extensive erosion and ulceration that occurs early in the disease process.
A study by Paterson and Matyskiewicz looked at the frequency that different primary factors were seen in 60 dogs with Pseudomonas otitis (Paterson and Matyskiewicz, 2018). It showed that 70% had allergies, 13% had tumours or polyps, 12% had some form of endocrinopathy and 5% had an autoimmune condition. Hence, allergy is by far the most significant primary cause of otitis externa in dogs.
Perpetuating factors
Perpetuating factors are those that support inflammation and prevent resolution even after controlling the primary factors. These will also have to be controlled in order to achieve long-term success with the treatment. The most important perpetuating factor is hyperplasia and the resulting stenosis of the ear canal, which makes it much more difficult to control and manage the otitis. When the structural changes in the ear are extreme, for example when there is severe ear canal fibrosis or calcification, then it may not be possible to achieve satisfactory results through medical treatment alone, and surgical treatment may be necessary.
Another significant perpetuating factor in otitis externa cases is a middle ear infection. Otitis media has been identified in 16% of cases of acute otitis externa and 50–80% of chronic cases. The most common pathogens seen in otitis media are Pseudomonas aeruginosa, Enterococcus faecalis, Proteus spp., Escherichia coli, Staphylococcus pseudintermedius and Malassezia spp.
Discussion
Sue Paterson wondered when investigations into the primary cause of otitis externa should begin: at the first consultation with a first opinion practice clinician?
Claudia Nett maintained that all aspects of the case will need to be addressed at some stage but it is perhaps unlikely that a first opinion practitioner would need to begin investigations into the primary cause at the first examination. First opinion cases are seen at her clinic by veterinary interns. They are told to treat acute cases empirically but to inform owners of the possibility that it could become a chronic case with significant cost implications, if not addressed early.
Chiara Noli said she will normally only see referral cases which have already been treated unsuccessfully, perhaps several times, by first opinion vets. In these cases, it is imperative to begin investigating the primary cause. So the answer to the question about when to start these detailed investigations would depend on whether the respondent is a first opinion practitioner or a specialist dermatologist.
Asked what advice on treatment she would give a first opinion practitioner, Dr Noli recommended daily flushing of the dog's ears with a disinfectant and steroid-based eardrops for a period of 10 days. There should be some response to this treatment but if the signs do return, then a full investigation should begin.
Ariane Neuber felt the key to this situation was good communication between the veterinary surgeon and the owner. The former should begin empirical treatment but should warn the owner that a full diagnostic work-up may be needed later. It would also be useful to conduct a cytological examination.
Jill Maddison noted that specialist dermatologists will often remind general practitioners that there is an underlying allergic cause in cases of otitis. But if the latter rely on ear drops containing various different active agents — steroids, antibiotics and acaricides — which can provide a temporary solution, then it could be difficult later to persuade the client that the underlying cause is an allergy. That possibility has to be discussed with the client at an early stage. Clients should be told that the problem in the dog's ear is likely to be a manifestation of something else going wrong, most likely an allergy. It is frustrating for general practitioners to have so few options for treating an atopic dog. If the patient appears to have an allergy, then the steroidal component of ear drops is the most important element, not the other active components.
Claudia Nett agreed that the lack of suitable licensed products is a serious issue. In view of the growing awareness of the problems posed by antibiotic-resistant strains of bacteria, there is concern that veterinary surgeons should only use products containing antibiotic agents when necessary: in the early stages of the disease, controlling the inflammation with steroids is important.
Sarah Warren felt that educating owners of young animals is vital, especially those belonging to vulnerable breeds such as Spaniels, Poodle crosses and brachycephalics. Owners must appreciate that the ear canal is lined with skin and subject to the same diseases as the rest of the body surface.

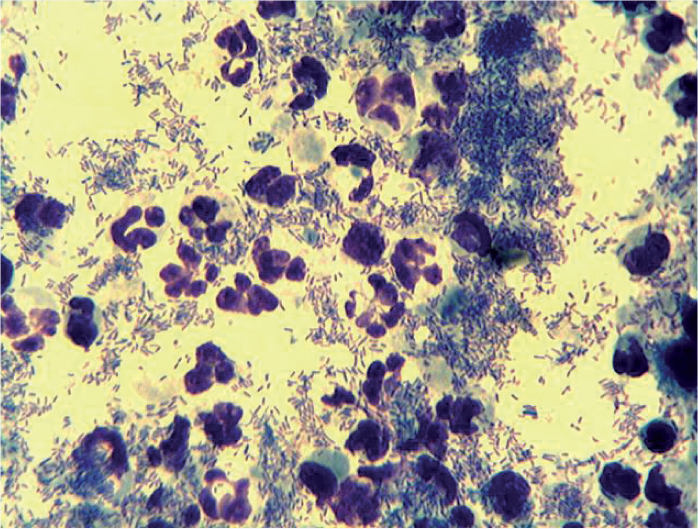
Nicola Ackerman said that nurses can provide this education for owners in puppy clinics where they can show how to examine the pet's teeth and ears, and also how to administer tablets. If puppies are trained to accept these attentions at an early age, it makes them much easier to handle later on. Nurses can also take cytology samples to help guide the decisions of their veterinary colleagues. Knowing what microbial populations are present will improve the effectiveness of symptomatic treatment. The nurses need to be properly trained and have confidence in using microscopes. Owners should be told that samples are needed to treat the current condition rather than find the underlying cause.
Jill Madison noted that it is difficult for first opinion practitioners to take and examine cytology samples within the time constraints of a 10-minute consultation. Most practices will not have the option of delegating the cytology examination to a well-trained nurse able to provide an immediate answer. Also, if 70% of cases are caused by an allergic response, will cytology results be particularly helpful?
Ariane Neuber suggested taking samples from cases of otitis and looking at them later. Even if no veterinary nurses are available who can look at them immediately during the consultation, they can be analysed later. A cleaner can be dispensed while the results are pending and drops can be prescribed later if needed. This ensures antibiotic stewardship and best practice. First opinion practitioners could train themselves to become more confident in examining cytology specimens by taking two samples, sending one to a diagnostic laboratory and comparing its findings with their own observations. Cytology is also a valuable tool in monitoring the response to treatment.
Sue Paterson pointed out that veterinarians from the Scandinavian countries are much more reluctant to use antibiotic products in otitis cases than their UK colleagues. They would argue that it is possible to successfully treat maybe 75% of otitis cases with antiseptics alone. Most pyoderma cases would be treated first with an antiseptic shampoo and the same strategy should work with ears.
Jill Maddison felt it was easy to overstate the value of cytology results, as they provide evidence on secondary issues, not the underlying primary cause.
Ronan Fitzgerald reported the system used in one practice where a dog presenting with otitis is examined first by a trained nurse. The animal will be seen by a veterinary surgeon only later when the results of cytology tests are available. The nurse is making a valuable contribution to the management of the case and is appreciated by the clients.
Nicola Ackerman stated that taking and examining cytology samples does not constitute a diagnosis under the Veterinary Surgeons Act and can be performed by veterinary nurses. There were many veterinary surgeons and veterinary nurses who do not fully understand what tasks can be delegated under schedule 3 of the Act. There is a concept of a nursing diagnosis which is not a full clinical diagnosis. Nurses can, for example, make a finding that a cat has urinary retention without actually diagnosing the underlying reason.
Claudia Nett explained that specialised dermatology nurses do not exist at present in Switzerland although there are programmes in place to develop nurse specialisms in other disciplines, anaesthesia, dentistry, nutrition and laboratory methods. Also there are not many first opinion veterinarians there who regularly perform their own cytology examinations.
Chiara Noli said that most Italian veterinarians work without nurses, relying on newly qualified veterinary surgeons and veterinary students to carry out basic nursing tasks. There were a few trained nurses at the university clinics, many of whom had trained in the UK. She added that while the ear drops currently on the market tend to contain the same agents — a steroid, an antibiotic and an antifungal — their formulations were different and so they produce different results. So cytology can be used to choose the right product for each individual case.
Ariane Neuber said veterinary nurses were an established part of practice in Germany but there were no veterinary nurses with specialist postgraduate training in dermatology. Progress is likely to be slow because the system is decentralised and getting agreement between the different federal states can be complicated. With regards to antibiotic stewardship, Germany has introduced stricter rules on antimicrobial use in veterinary patients and fluoroquinolones may only be dispensed after culture and sensitivity testing.
Claudia Nett agreed that the various different topical products do not have the same performance but first opinion practitioners are unlikely to keep a wide range of different products.
Nicola Ackerman described a study that she was involved with, examining the effects of cytology testing on prescribing patterns in veterinary practices. Starting treatment with an effective cleaning product and waiting for the results of testing, massively reduced the numbers of antimicrobial prescriptions being used to treat otitis cases (Ackerman, 2020).
Sarah Warren recognised that restrictions on the veterinary use of antibiotic agents were stricter in some European countries than in the UK and there was some justification for tightening up the rules on dispensing particular agents. Cytology should be used to direct the veterinarian's choices on the use of topical agents. It would be useful to have a product which is effective just against Malassezia for those cases where there is no evidence of bacterial involvement. She did not support strict rules on which products should be used — it was important to allow veterinarians to use their clinical and professional judgement.
Biofilms in otitis — how often do they occur in bacterial and yeast infections and how can we manage them? — Sue Paterson
Bacteria exist in two different forms during growth and proliferation. In acute infections, the bacteria will be present as single, independent ‘planktonic’ cells. However, in many cases of chronic infection it is probable that pathogens are organised into sessile aggregates described as biofilms.
While biofilms create challenges in treating medical conditions, they also occur widely outside the body and pose major problems in other settings, such as industrial processes, water supplies and heating systems.
A biofilm is any group of micro-organisms (bacteria, yeast, algae or fungi) in which cell–cell adhesion occurs as well as adhesion to a surface. Cells are embedded within a self-produced matrix of extracellular polymeric substance (EPS), which aids in cell adhesion and aggregation.
These films may form on any surface, including medical equipment, such as catheters, artificial valves, orthopaedic implants, but also on many body surfaces, such as the lining of the bladder or the ear canal, where the matrix will impede the normal function of antibodies and phagocytic cells of the host's immune system. It also protects these organisms against the agents that the clinician will try to use in controlling the infection.
In the case of a Malassezia infection, the process begins with a small number of sessile cells that attach to a surface where they grow, divide and form a mat. As the number of cells increases, they begin to produce the EPS material which will later form a considerable proportion of the biomass present on the surface. This may make it difficult to identify the causative organism aft er taking samples for cytology testing. The infectious organisms will stay within this protective shield where they display a phenomenon called ‘quorum sensing’ where they release chemicals that allow them to communicate with each other. The cells in the centre of a colony enter a quiescent state that makes them highly resistant to attack by antimicrobial agents. In some cases they can resist concentrations of the agent thousands of times higher than the lethal dose for the same organism in its planktonic phase.
These properties will create significant challenges for clinicians attempting to treat an animal presenting with a biofilm infection. However, there are some useful guidelines available in human medicine to help in dealing with such cases. It would be very useful for veterinary practitioners to have similar guidelines drawn up to help them make appropriate clinical decisions.
In 2014, the European Society of Clinical Microbiology and Infectious Disease (ESCMID) produced guidelines for the diagnosis and treatment of biofilm infections (Høiby et al, 2015). The criteria that ESCMID developed to determine a diagnosis of a biofilm-related infection require: a medical history of a biofilmpredisposing condition (e.g. a surgical implant or cystic fibrosis); an infection lasting more than 7 days; the failure of antibiotic treatment and the recurrence of the infection (especially if the same pathogen is present on multiple occasions); when infection resolves with antibiotic therapy but recurs once antibiotic treatment finishes; and documented evidence or history of antibiotic failure.
It is clear that similar conditions exist in veterinary patients but what is startling about the above guidelines is that human infectious disease experts interpret 7 days as the threshold at which an infection should be considered to be biofilm-related. Most of the otitis infections that will present at a dermatology referral practice will have existed for much longer than that.
There have been a few notable studies in the veterinary literature on the treatment of biofilmrelated conditions:
- Surgical implants — this will oft en require the removal of the implant before attempting to treat the infection (Edwards et al, 2016; Fullagar et al, 2017)
- Teeth and gums — plaque is a familiar biofilm challenge in veterinary dentistry but the canine mouth does at least provide ready access allowing the physical disruption of the film through mechanical cleaning (Holcombe et al, 2014; Oliveira et al, 2016)
- Bladder and mammary gland — these organs are a common site of biofilm formation in both human and veterinary medicine, and are both difficult sites to treat effectively (Melchior et al, 2006; Aslantaş and Demir, 2016; Shimizu and Harada, 2017)
- Wounds — biofilms can present challenges in treating wounds (Bayne, 2014; Swanson et al, 2014).
Biofilms in otitis
There is not a huge amount of literature on biofilms in otitis but here are a few of the important contributions. Chan et al (2019) published an article on biofilm production by pathogens associated with canine otitis externa and the biofilm activity of ionophores and antimicrobial adjuvants. This paper showed that both Pseudomonas spp. and Staphylococcus spp. will produce biofilms, but it also showed that drugs such as Tris EDTA and N-acetylcysteine are useful in helping to break down bacterial biofilms.
Youn et al (2018) looked at comparative efficacies of topical antiseptic eardrops against biofilms from meticillin-resistant Staphylococcus aureus (MRSA) and quinolone-resistant Pseudomonas aeruginosa (QRPA). Their paper is from the human literature but demonstrates the potentially huge role of antiseptic eardrops. They conclude that ear drops containing 4% boric acid and 2% acetic acid are effective against biofilms from MRSA and QRPA.
Pye et al (2013) evaluated biofilm production by Pseudomonas aeruginosa from canine ears and the impact of biofilm on antimicrobial susceptibility. This paper showed that the concentration of polymixin B, gentamicin, neomycin or enrofloxacin must be significantly increased to be effective against a chronic Pseudomonas biofilm. Topical antibiotic use is much preferable to systemic treatment in otitis externa because of the higher concentrations achievable. Another in vitro study by Pye et al (2014) evaluated the impact of tromethamine edetate disodium dihydrate on antimicrobial susceptibility of Pseudomonas aeruginosa in biofilms. This study showed that Tris EDTA can be a useful adjunct treatment for a chronic Pseudomonas biofilm, if topical gentamicin or neomycin is used, but that it does not work synergistically with fluoroquinolones, and may actually be antagonistic in vitro. It would be interesting to see if the same results are produced in an in vivo study.
A paper by Robinson et al (2019) looked at biofilm production of Pseudomonas spp. isolates from canine otitis in three different enrichment broths. This was a referral case population and so the pathogens are likely already to have been exposed to various different antibiotic treatments. More than 90% of the isolates were found to be biofilm producers. This is probably why Pseudomonas is such a difficult pathogen to treat in first opinion practice.
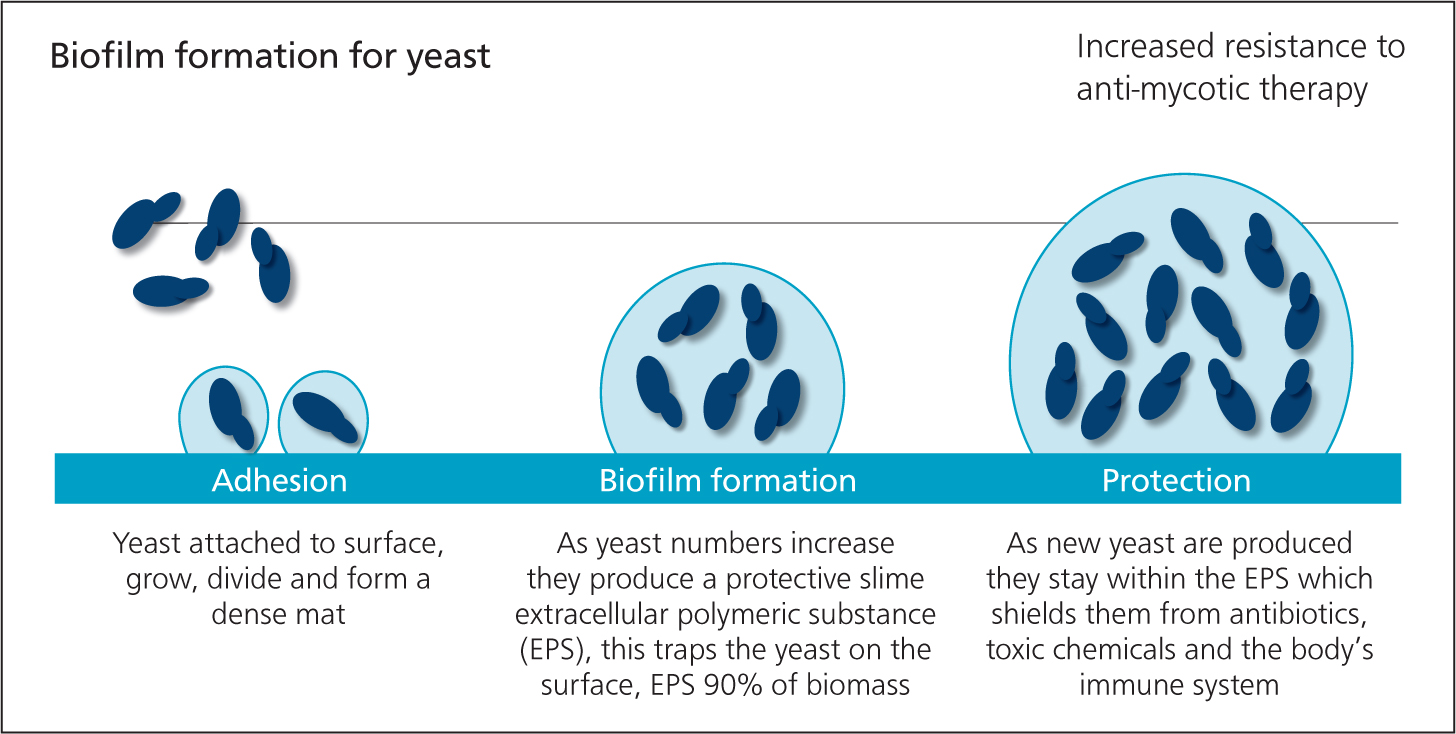
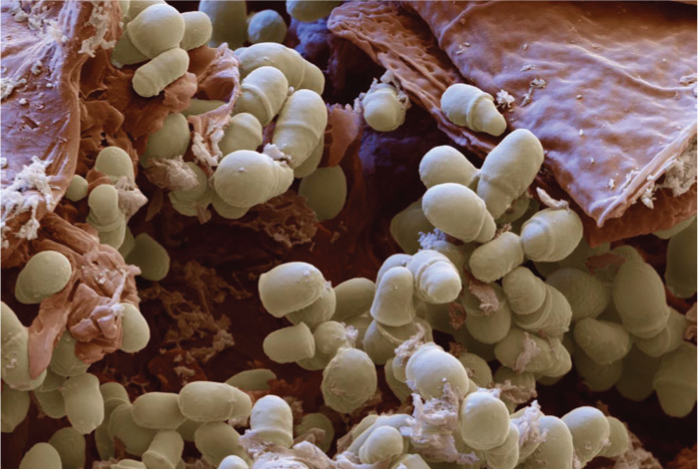
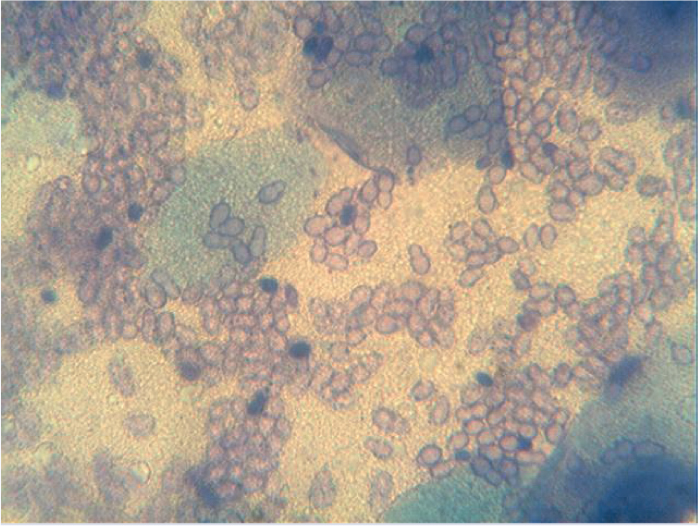
The ability of Malassezia to form biofilms
It is not commonly realised that yeast species such as Malassezia can form biofilms in the same way as the more familiar bacterial species do (Figueredo et al, 2013; Brilhante et al, 2018). Figueredo et al (2013) showed that once Malassezia forms a biofilm it will become resistant to topical agents. It is therefore essential to resolve infections with Malassezia spp. quickly and effectively before a biofilm forms. Once a Malassezia biofilm has formed, it becomes a major clinical challenge because of the resistance of the organisms to topical antimycotics.
A short commmunication co-authored with Stephen Steen was due to have been presented at BSAVA Congress in April 2020. The study was conducted after Dr Steen became concerned about the number of cases of Malassezia otitis that were being presented to him after unsuccessful attempts had been made to treat the infection with a range of different topical licensed antimycotics.
However, evidence from the study suggested that chronic otic Malassezia infections do form biofilms and that any topical antimycotic used after biofilm formation, whether it be miconazole, clotrimazole, nystatin or terbinafine, will be unsuccessful in therapy.
Evaluation of the biofilm-forming capacity of Malassezia pachydermatis
The Steen and Paterson study evaluated the biofilm-forming capacity of canine otic isolates of Malassezia pachydermatis: ten isolates were chosen that had been submitted to a diagnostic laboratory with a history of lack of response to antimycotic therapy; in all cases the patients had been treated with multiple products (clotrimazole, miconazole and terbinafine).
The isolates were identified as M. pachydermatis on the basis of their macroscopic and microscopic morphology and their ability to grow on Sabouraud's dextrose agar.
The protocol consisted of injecting 150 ul aliquots of each 0.3–06 OD570 suspension in triplicate into each of two sterile, polystyrene, flat-bottomed, 96-well microtitre plates, which were incubated at 37°C for 48 hours. A negative control of sterile Sabouraud liquid medium was also incubated in triplicate.
Following inoculation, the planktonic cells were aspirated and each well was washed twice with 150 ul of sterile phosphate-buffered saline (PBS) using gentle micropipetting to ensure biofilm integrity. 200 ul of sterile Sabouraud liquid medium was added to each well and the plates incubated for 96 hours at 37°C; spent broth was aspirated and replaced daily.
After 96 hours in culture, wells were washed twice with PBS as before and then air dried at 37°C. Adherent cells were then stained with 0.5% aqueous crystal violet for 45 minutes, before being aspirated and washed twice with 200ul of sterile deionised water.
Finally, each isolate was categorised as a non (<0.13), low (>0.13–<0.27), medium (>0.27–<0.54) or high (>0.54) biofilm-producing sample dependent on their OD570. The mean blank OD (broth) was measured as 0.279, while all 10 isolates were shown to have an optical density above 0.54.
The results demonstrated that all 10 of these isolates from clinical cases that were assessed for biofilm production were found to be high-level producing strains. In view of the fact that the antifungal susceptibility of Malassezia is known to be decreased when a biofilm is present, these results may explain the reason for treatment failure. As the early papers showed, when biofilms are formed, the immediate result is high resistance across the board to all the antimicrobial agents used.
It would seem that the existence of Malassezia biofilms is poorly appreciated in general practice. The questions to be answered by dermatologists in referral practice will be to explain what leads to the formation of these biofilms. Is it a result of poor penetration of the antimycotic agent in the ear, poor cleaning or the use of a weak steroid? Further issues could be an inadequate concentration of antimycotic in the ear preparation or using courses of treatment that are too short. Perhaps we should be using steroids and cleaning agents at the beginning to open up the ear and remove wax deposits that may diminish the effectiveness of medical treatments. First, however, are we seeing Malassezia biofilms in practice and are they a challenge to treat?
Discussion
Chiara Noli felt that treatment failures in Malassezia otitis can be much reduced by using high dose topical corticosteroids early on to reduce inflammation and infection. Daily ear cleaning and flushing with disinfectants and biofilm disruptors is also helpful.
Sarah Warren said there is definitely an increase in cases with Malassezia-related biofilms and the response to treatment is worse than in the past. Reports from diagnostic laboratories will highlight the presence of biofilms and suggest potential options for their treatment.
Sue Paterson noted that this is the most common issue raised by first opinion practitioners when calling her for advice. What were the panel's views on the reasons for this?
Sarah Warren proposed that the increased incidence of Malassezia otitis may be related to the increased popularity of Cockapoo-type dogs which appear to be vulnerable to this condition.
Nicola Ackerman had noticed that the problems may not be related to which treatments are used against Malassezia otitis, but how they are applied. Clients will often say that they have cleaning agents left over from a previous treatment, so veterinary surgeons in her practice have been instructed to give advice to owners on the volume of cleaning fluid that must be used. Delays in the supply of products has meant that her colleagues will often mix steroid solution with the cleaning fluid to give to clients.
Sue Paterson regretted that practitioners have resorted to off-license use of topical ear cleaners to which they have added corticosteroids and suggested it would be great to have a licensed antiseptic ear cleaner that contains a steroid.
Jill Maddison felt that breed factors such as the popularity of Cockapoo-type crossbreeds, brachycephalic breeds and Shar Peis may well be a factor in the growth of Malassezia otitis cases but she was not aware of any published data.
Chiara Noli said that poodle-crosses are not common in Italy — most of her cases are Labradors or Golden Retrievers.
Claudia Nett noted that Cocker Spaniel crosses are very uncommon in Switzerland, but poodle crosses, especially Labradoodles, have become popular in the last few years, and brachycephalic breeds are very popular. Swiss practitioners are certainly seeing a lot more cases of dogs with otitis biofilms. She did not think this was a breed issue as the population of Golden Retrievers and Labradors is not much different from years ago. Nor is it because owners are less able to clean their dog's ears, as they were never very skilled at this task.
Sue Paterson supported the suggestion that increased problems in treating Malassezia may be a result of increased use of topical antibiotics.
Jill Maddison argued that maintaining standards of antibiotic stewardship is vital. There is increasing understanding of the importance of the skin and gut microbiome in general health and in people there is also a clear link between antimicrobial therapy and the development of autoimmune disorders. In regard to the microbiome, the ear is an important organ and changes in the bacterial population will occur rapidly. She wondered whether the ear microbiome in veterinary patients had changed as a result of antimicrobial therapy. Another factor could be that dogs are being treated with eardrops at a younger age which may have an impact on the bacterial population and the development of atopic dermatitis as they grow older.
Sarah Warren felt that the frequency and duration of treatment as well as accurate dosing may be important factors. Ear drops are often better administered by a syringe as this will control the volume of fluid used and will probably be better tolerated by the patient.
Sue Paterson wondered if the changing lifestyle patterns of owners may be a factor in that they are often more busy and less willing to stick with a prolonged course of treatment. In such cases, would longer-lasting products avoid such lifestyle or compliance issues?
Current best practice in otitis assessment — Ariane Neuber
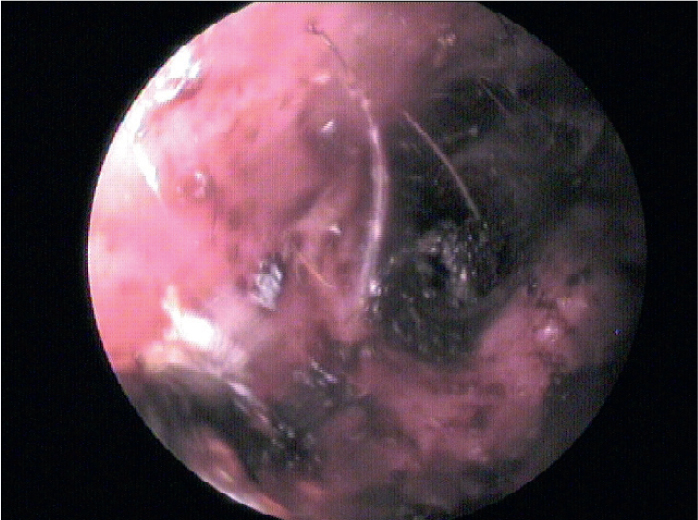
A thorough history is the basis for any assessment of a patient with otitis, taking in both its general medical history and a review of its dermatological and otic background. This will be followed up with a comprehensive physical examination, involving both a general inspection and specific dermatological and otic assessments. The otic examination will involve palpation and inspection of the pinna and external structures to detect any thickening of the tissues. Otoscopy will identify any significant changes, but this procedure is often painful, particularly when there is significant ulceration. In cases where it may not be possible to insert the instrument at the initial examination, it may be necessary to treat with corticosteroids and to wait until the inflammation has calmed down.
Cytology with culture and sensitivity testing of the samples will provide important information, showing for example whether there is an active infection with Malassezia spp. or Gramnegative bacteria. Sensitivity testing is not always necessary at the initial examination but is indicated if empirical treatment is ineffective. Further tests may include imaging and ear flushing under general anaesthetic. In the longer term, there may be a need for further investigations to identify any underlying allergies.
The pros and cons of live and virtual consultations
Which parts of this process can be carried out as part of a virtual consultation and which will require the presence of the live animal? In both situations, the history taking may take some time, and so the clinician may choose to provide the client with a questionnaire in advance, which they can complete with the help of a practice nurse. One disadvantage of a virtual consultation is that the clinician may miss some important non-verbal communication.
In a virtual setting, the physical examination will be more limited and the clinician is very dependent on the information provided by the client. Technological aids, such as images captured using a smartphone or laptop, may be valuable. However, there are important details obtained in a live examination that require the clinician's other senses such as the odour and physical properties of any discharge present in the ear. Long-term assessment will also involve procedures requiring the physical presence of the animal, such as blood sampling.
Time constraints may affect both live and virtual consultations and so it may be necessary to book a double appointment or ask the client to return for a second consultation. Veterinary nurse consultations can be helpful in managing these cases. If a food trial is to be undertaken, much of the necessary information can be provided to owners in the form of hand-outs.
Otoscopic assessment of otitis
Otoscopy is an important tool in the physical examination of the ear and video-otoscopes are being used by increasing numbers of clinicians. These technologies provide a range of important details on the presence of stenosis, discharges, ceruminous gland hyperplasia, masses, foreign bodies and ear mites. The appearance of the tympanic membrane should be noted, and whether the tissue is intact, clear or opaque in appearance, and whether it appears to be bulging, which would be an indication that otitis media is present.
Remote assessment of otitis
Remote otoscopy technologies have been introduced for the human medical market that can increase the amount of information that can be generated during a virtual examination. These include relatively inexpensive devices that can be inserted into the pet's ear canal and transmit images via a smartphone or tablet. There is little information available yet on how useful these devices are in the veterinary setting. Evidence will be needed on how well tolerated they are by the pet, whether there is any risk of damage to the tympanic membrane and other delicate structures, the quality of the images obtained and the degree of training needed for their use.

Cytology may be the most important diagnostic procedure in otitis cases and samples should be taken at the first consultation, although it is likely that this is an underused approach among first opinion practitioners. Follow-up examinations would also be useful in helping to monitor the effects of treatment on the bacterial and yeast species that are secondary factors in the aetiology of this condition.
It may now be possible to carry out such examinations remotely. A team at Stanford University has developed a device called the Foldscope (Cybulski et al, 2014), an origami-based paper microscope and lens that costs around $10. It is claimed that the device is capable of magnifying an image 2000 times. The device can be provided to clients or the referring veterinarian with the materials needed to take a sample (cotton buds and methylene blue) and instructions on using the technology. There is a published paper on using this technology to take cervical smears, which is being used in areas where access to conventional smear tests may be limited (Naqvi et al, 2020). When attached to a mobile phone to transmit the images, the performance of this device appears to be reasonably good. The sensitivity and specificity of the tests are considered quite good with an overall accuracy of about 80%.
Today there are a number of companies offering remote consultations in this discipline either to referring veterinarians or to owners, such as Virtual Vet Derms, Joii, FirstVet. There are differences in approach between these service providers but for each company, the coronavirus lockdown has probably had beneficial effects in stimulating demand. Remote prescribing has also been influenced by the crisis but it is not clear whether the current temporary arrangements will continue long-term.
Will telemedicine ever replace a traditional otic examination?
There are a number of positive aspects to this new approach — reduced overheads for the service providers and therefore lower costs, improved access to care in some remote areas, greater convenience for pet owners, the potential for slowing the spread of infectious agents, such as meticillin-resistant Staphylococcus pseudintermedius (MRSP). The new system has also provided a new revenue stream for practices at a time when there have been restrictions on normal services and the new arrangements may improve client satisfaction.
But there are also some negative aspects to the new arrangements. Insurance companies may be unwilling to pay for a virtual consultation, there can be data protection issues and the potential for remote prescribing may generate problems with medicine licences. There are also still some concerns about the quality of images available with current technologies, and worries about diagnostic standards when it is not possible to carry out a full examination of the patient or to carry out all the available diagnostic tests.
Some of these current issues may be resolved through the development of better technologies or advances in software. Access to broadband technologies is also likely to improve in more remote regions. Other social and economic factors will influence the take up of these services, such as fears over direct contact with other people during a pandemic. A shortage of veterinary surgeons and veterinary specialists may also drive the adoption of new methods, and the probability that costs will go down is likely to further stimulate interest in these services.
However, some of the negative aspects of telemedicine are unlikely to change. The loss of information provided through non-verbal communication and the fact there will also be a reliance on the abilities of the person operating the technology. Clinicians will always find it harder to obtain a full picture of the case without direct contact with the patient, and both client and clinicians will regret the absence of human contact and empathy, so it is unlikely that virtual consultations will ever totally replace live ones.
Discussion
Sarah Warren said she believed telemedicine would never replace a full otic examination but the current situation with COVID-19 is presenting huge challenges by preventing many people visiting their usual veterinary practice. Owners may be self-isolating and in some parts of the country, practices have to turn otitis cases away because they are not considered to be emergencies. Where telemedicine is particularly helpful is in providing a triage service and ensuring that owners can be given sensible advice on next steps.
She explained how her company has been working during the crisis. Its veterinary surgeons are available 24 hours a day and 7 days a week, and free nurse consultations can be arranged between 8 am and 10 pm, offering guidance on whether a veterinary appointment is necessary. Over the past 6 months, its staff have carried out over 20 000 consultations, including around 1000 otitis cases, of which about 20% were directed to a local veterinary practice for further investigation and treatment. In 60% of cases seen, staff recommended a product; of these, 70% were recommended antiseptic ear cleaners and 30% were recommended a POMV topical ear treatment. In 75% of those that were recommended a POM-V, the product was a first-line polymyxin B preparation. Any recommendations for fluoroquinolone antimicrobials were based on culture and sensitivity testing. All cases where a product was recommended were booked follow-up consultations and no adverse reactions were noted.
Chiara Noli noted that it may be difficult to take swabs from an aggressive dog without having to give it a general anaesthetic. Owners may be asked if they can handle the animal but her experience suggests that owners are rarely able to take the sample from where it is needed, deep down within the ear canal.
Sarah Warren agreed that safety of owners and practice staff was very important in cases where the animal had a painful ear. These cases should always be taken into the practice. In some circumstances it may be possible to get a sample of the discharge using a gloved finger. Some owners may be capable of taking a sample from the correct site but there is no guarantee.
Sue Paterson mentioned the NHS England declaration that it would aim to become carbon neutral by 2040. She understood that about 10% of its current carbon footprint is a result of staff and patient travel. The COVID-19 crisis has shown that one way to significantly reduce this figure would be to provide consultations and advice remotely, and by allowing staff to work from home. Of course, one difference between veterinary surgeons and medics is that the latter can talk directly to their patients, but should primary care vets be looking to increase the range of services that they provide online, including nurse consultations?
Nicola Ackerman felt that it depended on the individual circumstances, some clients only want to see a veterinary surgeon but others are happy to talk with a nurse. At the moment in her practice, the disease control restrictions have made it very difficult for owners to see a veterinary surgeon as there are so few appointments available. There is a huge role for the practice nursing staff to operate a triage service. She hoped this would continue after the restrictions end, because it is providing a service that is particularly appreciated by cat owners whose pets find visits to the clinic very stressful.
Jill Maddison said that according to the human medical literature on the factors that were essential in making a diagnosis, a full history accounted for 80% of the information while physical examinations and diagnostic tests accounted for the remaining 20%. So history is hugely important and this can be taken remotely in most cases. There are, however, some cases in which the physical examination is the ‘cruncher’, whether it be feeling the abdomen for a mass, listening to the chest or examining the gums for signs of jaundice. But in most patients with an internal medicine issue, the history will tell the clinician whether or not a physical examination is essential. So a well-managed and well-triaged telemedicine service has huge potential. Many consultations that take place in veterinary practice involve the ‘worried-well’ who only need some reassurance: that can be provided over the telephone or, better still, in an online video consultation.
Ariane Neuber agreed that there are many cases in which reading the referral letter will give the clinician a very good idea of what is happening to the animal. Follow-up tests may be useful in ruling out some of the possible factors.
Sue Paterson concurred with the view that managing telemedicine services was the key issue here. There is enormous potential for using telemedicine consultations in particular situations such as re-checks during ongoing treatment. Playing devil's advocate, she wondered how many of those on the panel had been to their own GP with an ear problem and the clinician had carried out a proper otic examination or had done cytology tests. Even in the absence of those steps, it is likely that the clinician did prescribe a treatment and the condition did improve.
Jill Maddison said the great power of a telemedicine consultation compared with a telephone call was in being able to see the animal. Sometimes there was a mismatch between the owner's concern about the animal's state and the appearance of the patient when it comes into the consultation room. A clinician will begin assimilating the necessary information for their diagnosis when they first see the animal, and so a telemedicine consultation provides a degree of safety that is not present in a telephone call where you are entirely reliant on what the owner says.
Sue Paterson observed that data from the USA suggests that heavy use of telemedicine results in an increase in the prescription of antibiotics because clinicians err on the side of caution. This shows how important it will be in the UK for veterinary telemedicine to be properly regulated.
Sarah Warren agreed that the availability of good quality images was hugely important for telemedicine. Her company encourages clients to take still images of their pet before the consultation so that they are not chasing the animal around while talking to the veterinary surgeon. It is now also possible for clients to upload video clips which may be particularly helpful in dealing with behavioural problems, for example. The company has tasked two of its veterinary surgeons with responsibility for ‘telehealth excellence’, creating guidelines and protocols to streamline the video consultation process, maximise the quality of information obtained by the owner and ensuring that gold-standard evidence-based medicine is practised. Telemedicine is not only useful for triage, as clients will often need to know whether to attend the practice out-of-hours, or if the problem can wait until the next morning, but may have a very useful role in the ongoing management of certain chronic diseases, thereby improving client compliance.
Ronan Fitzgerald said that if the availability of consultations within the practice is limited then it makes sense to use the available slots for initial examinations and use telemedicine consultations for the second appointment. Currently, most follow-up discussions will be carried out by telephone to comply with concerns over social distancing.
Chiara Noli wondered about the quality of the still images that Dr Warren's company receives. In her experience, the pictures transmitted via WhatsApp tended to be very poor. If they are out of context or out of focus, the clinician will struggle to make an appropriate diagnosis.
Sarah Warren disagreed, saying that the quality of images captured by clients on their smart-phone was usually very good and it was possible to see features such as intact pustules and epidermal collarettes, for example. In her experience the cameras on smart phones are very good.
Sue Paterson sympathised with Dr Noli's point after she was sent a picture for an advice call in which the main feature was a radiator! The competence of the person taking the picture has to be taken into account.
Asked if there were any recommendations that she could give on remote otoscopic technologies, Ariane Neuber felt it was difficult to obtain really sharp images with the equipment currently available.
Sue Paterson agreed that the technology available for this sort of investigation is still catching up. In 10 years' time, she was sure there would be technology on the market that will be capable of collecting the information that is now only available through a physical examination.
Owner compliance in administering treatment at home — Jill Maddison
Compliance is obviously a major issue with the treatment of otitis. The animal cannot administer its own treatment and is entirely reliant on the owner's actions. An owner who is 100% compliant will give all the medication prescribed, at the right intervals. An owner who is not 100% compliant may miss doses (sometimes or often) and/or finish a course of treatment too soon and/or give the doses at the wrong time. In the human medical literature, the term adherence is generally used instead of compliance, possibly to make the process less ‘bossy’.
Compliance will rarely be total and it is generally considered that an 80% compliance rate is a reasonably good response. The standards of compliance will depend on the disease and the animal species concerned. There is a single study looking at comparative compliance with two different ear preparations (once vs twice daily) which indicated a similar level of compliance to that reported for oral medication with the twice daily dose (80%) and better compliance (100%) with the once daily dose (Boda et al, 2011). There is a particular risk of noncompliance in cases where the animal has a good initial response so the owner does not complete the course of treatment. Giving the dose at the wrong time is another problem, especially with the administration of corticosteroids.

The factors responsible for poor adherence/compliance have been studied much more closely in the human medical field than in veterinary medicine but it is likely that they will be much the same. Maintaining good compliance is vital in human treatment, in areas such as the management of HIV, tuberculosis, blood pressure disorders and for many public health challenges. The few studies published in the veterinary literature mainly involve antibiotic treatment and suggest that between 70% and 80% of clients will administer the treatment as prescribed although they may not give it at the right time (Barter et al, 1996a,b; Grave and Tanem, 1999; Adams et al, 2005). There are various barriers to full compliance, and they fall into four categories: medication-related, client-related, client–vet relationship related and patient-related.
Medication-related barriers to full compliance
Medication-related factors include the frequency of dosing, with lower compliance in the administration of any medicine that must be given more than once or twice a day. Administering multiple medications is another problem, along with whether the medicine should be given with food. Instructions to not give with food will reduce compliance because that is how many owners are able to persuade their dog to swallow the medicine. In human medicine, for alcoholics taking naltrexone, compliance was shown in one study to be 71% in the first 13 weeks but by 52 weeks it had fallen to 43%.
Otitis cases seen in veterinary practice are unlikely to need medical treatment for that length of time but clients may be asked to keep cleaning their pet's ears on a long-term basis. Palatability is an issue in treating some conditions but that is unlikely to matter with aural treatment. But clarity of instructions and whether these are given verbally or in writing will matter in the management of otitis.
Client-related barriers to full compliance
Client-related factors focus mainly on lifestyle and whether the owner is too busy to always remember to give the medicine as prescribed. Remembering to give the medication can also be a problem in other situations, for example, in clients whose memory is failing. Better client understanding of their medication will improve compliance. Enhanced compliance has been demonstrated in animal owners given more information than is standard about bacterial infections and antimicrobial therapy. Similarly, human asthma patients who wished to know more about their treatment than they had been told were found to be less compliant.
A further issue that may affect compliance is the client's belief system. One study of medication compliance in Scandinavia where veterinary surgeons can prescribe but not dispense antibiotics showed that 18 of 95 clients had to be excluded from the sample because they did not fill in their prescriptions and had not informed their veterinary surgeons of this. The main reason for this lack of compliance was that the clients did not believe that antibiotics were necessary for their animal or they did not support the use of antibiotics in animals. This reluctance was often linked to a more general scepticism about the value of western medicine.
In a recent study, RVC students looked at how often clients follow up on the recommendations given to them for the treatment of dental disease in their dogs. The most common reason given for not complying with the veterinary surgeons' instructions was cost, which was a deterrent for 78% of clients (Dean, 2020). Fear of giving the animal a general anaesthetic was the second most common reason, which was surprising and clearly something that veterinarians will need to address.
Compliance in veterinary medicine shares some similarities with that in paediatric medicine. Patients or animals living in families with relationship conflicts are less likely to receive their medicines as prescribed, and the child or animal that responds badly to being given their medicine will not receive optimal treatment. Some differences in the willingness of dogs to submit to treatment may be breed-related. Meanwhile, otitis treatment in animals may cause pain and discomfort for the patient which is a particular barrier. In cats there is often a reluctance to comply with any form of treatment.
Importance of the client–vet relationship
One issue that needs to be considered is the relationship between the client and the veterinary surgeon — the client's satisfaction with the consultation process will have an impact on how compliant they are with the clinician's recommendations.
The traditional concept of compliance with the veterinary surgeon's or doctor's instructions is based on a very paternalistic relationship in which the client or patient is not greatly involved in the decision-making process and they are unlikely to be able to voice any concerns that they may have with the proposed treatment. In such consultations, the veterinary surgeon will dominate the conversation and set both the agenda and the pace of the conversation. The content of the discussion may be very technical and so the client's contribution will diminish.
The modern alternative to this approach is that of relationship-centred care. This will involve a discussion between the health professional and the patient/client which takes the form of a negotiation intended to achieve an outcome acceptable to both sides. The evidence suggests that this approach will generally lead to more favourable medical outcomes.
In a veterinary setting, the clinician should acknowledge the role that the pet plays in the life of its human family and seek to find out what the client wants and expects from the discussion. It is important to investigate any concerns that the client may have about the treatment. Compliance has been shown to be significantly higher when animal owners feel that their veterinarian has spent sufficient time on the consultation. Similarly, human patients who indicated that they wished to spend more time with the doctor than they were permitted were less compliant than average. Also patients who felt uncomfortable about asking the doctor questions tended to be less compliant.
Clients may be more likely to admit to noncompliance with a receptionist or veterinary nurse. Veterinarians must recognise that they cannot predict which of their clients will be compliant and so they must treat them all as potentially non-compliant. A strategy for improving compliance should be to involve the client in treatment decisions by explaining why the medication is being dispensed, what the expected outcomes are, and what are the potential consequences of poor compliance, which may be more than a simple failure to get better when the treatment involves an antibiotic.
Compliance is significantly improved by repeating the most important instructions and giving a verbal explanation of the effects of the medication. Treatment may also need to be individualised by choosing a treatment regimen that suits the client's lifestyle, and dispensing formulations that suit the needs of both the pet and the owner. If possible, the clinician should choose a medication that can be given with food or can be linked to some other activity performed at a consistent time each day.
Veterinarians must try to ensure that their instructions are clear, and support verbal instructions with written information. If the instructions are to be given on the label, there must be enough space for adequate instructions. Veterinary surgeons should be sensitive to any physical or visual acuity problems that the owner may have, should highlight the most important elements and provide additional written notes where necessary. The YouTube video produced by veterinarian Fiona Smith gives useful information for clients on how they should administer otitis treatments (https://www.youtube.com/watch?v=UzxZdoul0qA&ab_channel=Vetsure)
Veterinary nurses are likely to play a key role in enhancing communication with clients and demonstrating the correct technique for administering the required medication. They will also be able to educate clients about the treatment regimens and why they are important, and again in follow-up discussions on the outcome of such treatment. Clients need to feel that they have received good value from their interactions with the practice and veterinary nurses are able to enhance the perceived value of the consultation.
Moreover, if the client is struggling to follow the instructions, they are more likely to admit this to a veterinary nurse. Clinicians should never forget that however accurate their diagnosis may be, how correct their treatment, and how carefully they have chosen the drug, the treatment will not work if the client is unable to administer it.
Discussion
Sue Paterson noted that secondary infections are a common feature of otitis cases, so she felt that cytology samples should be taken at the first consultation. This would add value to the consultation and possibly help make the client more compliant by improving their understanding of why they have been asked to use a particular treatment.
Jill Madison agreed that this approach would be valuable as veterinary surgeons often take it for granted that their client understands the aims of treatment. Talking to the client while taking a sample gives an opportunity for the vet to explain what they are trying to do. It will give the client more awareness of the rationale for the treatment and make them more likely to follow the instructions. With otitis treatment this is particularly important as the key issue that clinicians are facing is the rise of antibiotic resistance, resulting from inappropriate use of these agents. In these circumstances, it is essential that the client understands the consequences of poor compliance. Unless the treatment plan is followed, this may speed up the emergence of resistant strains.
Nicola Ackerman felt that veterinary nurses will often provide a link between the veterinary surgeon and the client. Too often pet owners will come out of a consultation and tell the nurse that they do not understand why they have been given a particular medicine or that they do not know how to administer it. There are two American-trained veterinary surgeons at her practice who are used to providing 30-minute consultations — so they are used to providing information for clients about the treatment on the label and how it should be administered. Compliance with the instructions of those particular vets has been found to be much better than average.

Chiara Noli said she had searched the literature on compliance with otitis treatments in veterinary patients and found one 10-year-old paper which reported better results with treatments given once a day rather than twice daily (Boda et al, 2011). This relates to the concept of caregiver burden which has become a focus of interest because it has been realised that the responsibilities of being a carer may influence the effectiveness of that care and the quality of life for both carer and pet. In otitis cases, the carer may also feel the burden of watching a dog that is constantly scratching itself and has an unpleasant-smelling discharge. Receiving treatment will particularly affect quality of life for cats.
Dr Noli said she has been involved in a study comparing the clinical efficacy and quality of life impact of two protocols for treating ear disease. One involved ear washing twice a week and once daily ear drops. The second involved a single product given at weekly intervals for 2 weeks. The clinical efficacy and cytology findings were identical with the two protocols but there was a huge difference in quality of life scores. Owners that had fewer responsibilities had a much better quality of life. For those having to provide daily treatment, their quality of life only improved after the end of the treatment, although their dog's otitis scores had improved much earlier. It is important to find a treatment schedule that makes life easy for the owners, particularly when dealing with what may be a lifelong condition.
Jill Maddison agreed that changes in client lifestyles have influenced compliance but that may be for the better. Thirty or more years ago, rabbits were regarded as a children's pet and they received limited care. Now the bond between adult owners and their rabbits is often very strong. Quality of life has become a consideration for both the client and their pets. Research is being undertaken at the RVC into the effects of long-term diabetes treatment on the animal and their owner whereas in the past the veterinary surgeon's main concern was with monitoring blood glucose levels. A similar project is also being undertaken on the management of Cushing's disease. There has been a big shift in attitudes with an emphasis now on the effects of treatment on the owner as well as the animal. This has helped drive the importance of shared decision making over the past decade.
Ronan Fitzgerald noted that in the last practice he worked in before moving into industry, veterinary surgeons were expected to carry out 16 consultations in a 2-hour period. He proposed that this may have been an important factor if there was poor compliance. Given that appointment times are longer in referral practice, does this mean that compliance is improved?
Jill Maddison replied that there are no published data to answer this question but she was aware of unpublished findings from one animal health company that she has worked with, that showed compliance was a little better in referral practice but was not as good as the clinicians concerned, believed it would be. This may be surprising, considering the greater costs of a referral consultation.
Ariane Neuber pointed out that the client populations for first opinion and referral practice were very different, particularly in countries where the pet insurance industry has not grown as much as it has in the UK. Clinicians do have more time to explain their treatment and for that reason compliance is likely to be better. But there are some clients that are unwilling to listen to what the clinician has to say.
Sue Paterson noted that in UK first opinion practice there was a shortage of veterinary manpower at the moment, with long waiting lists for consultations and pressure to carry out consultations within the allotted time. This is likely to drive efforts to expand the use of RVN consultations and telemedicine in general practice. Reinforcement of the messages given about the proposed treatment is very important and that is an ideal role for nursing colleagues.
Key Points
- To successfully treat otitis and improve the long-term outcome, it is mandatory to address and identify the 3Ps.
- The most common cause of otitis is an allergy.
- Otitis media is an important perpetuating factor in chronic otitis.
- Food allergy is common in otitis cases with no concurrent skin disease.
- Pseudomonas spp. has been shown to produce biofilms in a high percentage of cases of chronic canine otitis externa.
- Yeast species such as Malassezia can form biofilms in the same way as the more familiar bacterial species.
- The existence of Malassezia biofilms is poorly appreciated in general practice.
- The presence of a biofilm could be the reason for treatment failure.
- Thorough history taking is a vital part of assessment for all patients with otitis.
- A comprehensive physical examination and otoscopy will provide further valuable information for making a diagnosis.
- Cytology is useful for determining whether a bacterial or yeast infection is present, and for establishing whether treatment is effective.
- There are both pros and cons for live and virtual consultations.
- Some of the current problems with telemedicine are likely to be resolved with the development of better technology and advances in software.
- It is unlikely that telemedicine will replace live consults completely for cases of otitis in the near future.
- There are various barriers to good compliance, and they fall into four categories: medication-related, clientrelated, client–vet relationship related and patient-related.
- Medication-related barriers may include frequency of treatment and length of treatment.
- Compliance is improved if the client understands the rationale for the medication and consequences of poor compliance.
- The quality of the veterinary surgeon–client relationship influences compliance.
- Medications prescribed should suit the client's lifestyle — a treatment will not work if a client is unable to administer it.
- A patient's response to medication administration will impact on compliance and this may be particularly relevant to application of topical ear treatments.
Concluding thoughts
At the close of the discussion, each participant added their own take-home message:
Jill Maddison — The importance of biofilms in the development of dental disease is well known but their importance in ear disease has been underestimated. It is important for practitioners to recognise that allergy, not infection, is the initiating factor for many cases of otitis in dogs and cats.
Sarah Warren — Many veterinary surgeons are adding aqueous steroid preparations to ear cleaners themselves and it would be great if the animal health companies could explore the possibility of producing licensed products, similar in formulation but without an antibiotic component.
Nicola Ackerman — Greater use should be made of the opportunities provided by telemedicine. Encouraging clients to send good quality images of their pet's ears before the consultation would save time and provide valuable information. Practices should also consider sending their clients, quality of life and pain-scoring indices.
Chiara Noli — I was intrigued by the tools that Ariane Neuber described that can be used in telemedicine, such as the Foldscope. These technologies may also prove useful in allowing veterinary staff to monitor client compliance with the agreed treatment. The cost of coming into the practice for a follow-up appointment may be a deterrent for many owners and so these technologies will allow checks to be carried out at a distance and at much lower cost.
Claudia Nett — I was impressed with the concept of the foldable scope and the possibility for using telemedicine in rechecks. However, there are still challenges in making the most of these technologies. Under Swiss law, for example, it is essential for the veterinarian to have an existing professional relationship with their client before dispensing medicines.
Sue Paterson — While the pandemic has created massive challenges for the veterinary profession, it has also opened our eyes to the many opportunities that exist to allow us to improve our patient care.
Ariane Neuber — The main lesson for me was to make better use of the nursing staff in practice in communicating with clients about the proposed treatment and that this is likely to improve owner compliance.
Otitis externa: introducing Neptra®
Although the diagnosis of otitis externa may be straightforward, determining its aetiology may not be. In order to maximise the chances of identifying the causes of the otitis and thereby selecting the optimal approach to each case, veterinary surgeons should adopt a threepronged approach involving history taking, a thorough examination (including otoscopy), and cytology of the ear discharge. Cytology should be performed in all cases of otitis externa. Examination of the otic exudate is quick, simple and practical and allows one to identify whether or not microbial infection is present; if it is, cytology facilitates appropriate product selection and also monitoring of the response to treatment. As discussed elsewhere in these proceedings, ear cleaning is an important element of managing cases of otitis externa, particularly if there has been biofilm formation. Failure to deal with this problem could potentially lead to product failure as a result of the inability of the antibacterial or antifungal component to actually reach the target pathogens.
An overview of Neptra®
Neptra® is a topical ear product for dogs and contains a unique combination of active ingredients: florfenicol, terbinafine and mometasone furoate. It is licensed for the treatment of Staphylococcus pseudintermedius and Malassezia pachydermatis, the most common bacterial and fungal pathogens, respectively, in acute otitis externa. Not only is it a unique combination of active ingredients, it is also the only otitis externa treatment licensed as a single vet-administered application.
Florfenicol, the antibacterial component of Neptra®, is a bacteriostatic antibiotic and a fluorinated derivative of thiamphenicol. Its spectrum of activity includes Gram-positive and Gramnegative bacteria, including S. pseudintermedius, with low resistance rates1. In a recent study which looked at the in vitro susceptibility to florfenicol of 600 isolates of S. pseudintermedius obtained from the ears of dogs with otitis, 99.3% were found to be sensitive2. Florfenicol is a ‘niche’ antibiotic in companion animal medicine: it is not used in any systemic formulations and is only found in one other topical product. In addition, florfenicol is not listed as a critically-important antimicrobial in human medicine3.
Terbinafine is an allylamine with pronounced fungicidal activity. It selectively inhibits the early synthesis of ergosterol, which is an essential component of the membrane of yeasts and fungi, including Malassezia pachydermatis. Terbinafine has a different mode of action to azole antifungals, therefore there is no cross-resistance with them.
Mometasone furoate is a potent, synthetic glucocorticoid that has been used in a variety of human and veterinary otic preparations. It has been referred to as a ‘soft potent glucocorticoid’ because it is more potent than some older glucocorticoids, yet not as likely to cause systemic adverse reactions, such as adrenal suppression. The mometasone is used to reduce exudation and swelling associated with otitis externa, thereby promoting drainage and ventilation, allowing for the antibacterial and antifungal agents to better exert their effects1.
Compliance and Neptra®
It is well recognised that compliance can have a major outcome on the success of treatment, both in human and veterinary medicine. In 2005, it was reported that 50% of the 3.2 billion annual prescriptions dispensed each year were not taken as recommended4. On the veterinary side, a review of studies about compliance revealed that although 70 to 80% of owners administered the right number of doses each day, only 20 to 34% gave doses at the correct time5. With regards to the use of topical products to treat otitis externa, there is a risk of over- or underdosing, missed doses or the course of treatment being stopped too soon. There is also the possibility that the owner may be scared to treat the dog or unable to administer the treatment for fear of hurting the animal or indeed, being hurt by it. Not only does this increase the potential for treatment failure, it may also undermine the client's confidence in their veterinary surgeon. A survey6 of dog owners in 2019 found the following:
- 86% of owners said that reducing stress for their dog was a priority when treating ear infections at home
- 55% of owners thought administering an ear medication twice daily for up to 14 days at home would be difficult or impossible
- 70% of dog owners preferred a single-dose treatment administered by the veterinary surgeon.
Using Neptra® avoids issues of owner compliance. The treatment is administered in the veterinary practice meaning that compliance is not a problem and the veterinary surgeon knows that the treatment has been administered correctly. This avoids any stress the owner may feel about having to try and treat their dog and there is no impact on the dog–owner bond.