Osteoarthritis is a commonly encountered condition in both dogs and cats, particularly as they age. In dogs under primary care in the UK there is an annual prevalence of 2.5%, with larger breeds having an even higher prevalence, such as 7.7% in Golden Retrievers (Anderson et al, 2018). Cats appear to have a very high prevalence of osteoarthritis with evidence of appendicular degenerative joint disease in 74% (Kimura et al, 2020).
A diagnosis of osteoarthritis is frequently presumptive, based on history, clinical signs and orthopaedic examination. Historical indicators of osteoarthritis are usually a reluctance to exercise, which may include reports of laying down more often during play; stiffness when rising that is worse after a period of inactivity; lameness, and a reduced ability to jump. Cats may also have an unkempt appearance and no longer sharpen their claws (Bennett and Morton, 2009).
One study found that many veterinary surgeons were frustrated that owners do not always accept their recommendations for analgesia in affected pets (Belshaw et al, 2020). This article explores the available tools that can be used in clinical general practice to help diagnose and monitor patients with osteoarthritis.
Osteoarthritis causes chronic pain, which can wax and wane, so a singular snapshot of the patient in the consulting room for 15 minutes may not represent the entire clinical picture (Belshaw et al, 2020). One of the most useful and underused tools for a more thorough assessment of the patient's condition is a client metrology instrument (questionnaire) (Mathews et al, 2014).
Client metrology instruments for canines
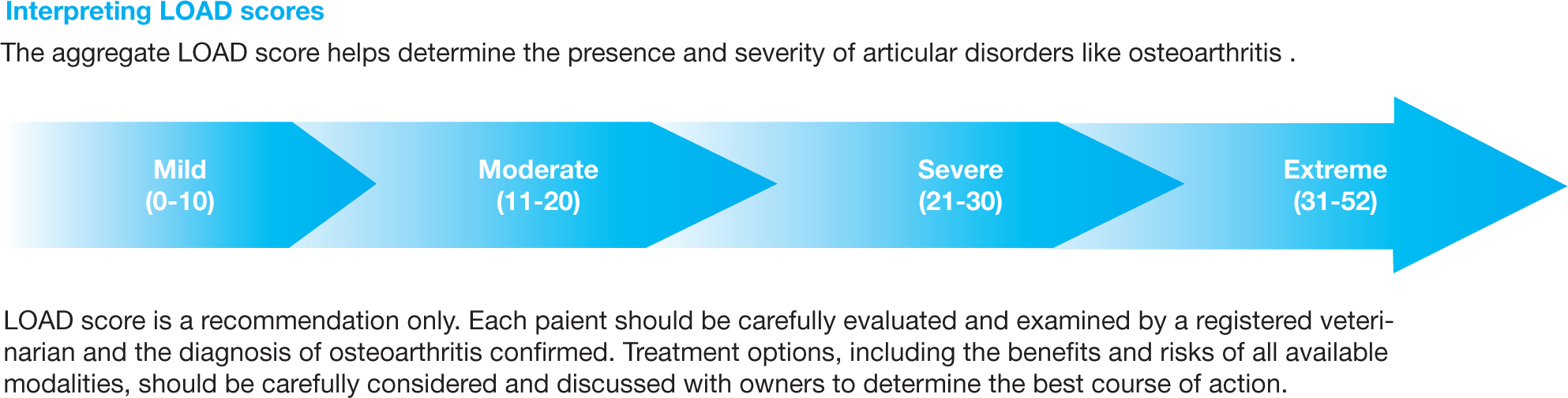
There are many available, validated, client metrology instruments for canine patients. The most readily accessible in the UK are the Liverpool Osteoarthritis in Dogs (LOAD) questionnaire, the Helsinki Chronic Pain Index and the Canine Brief Pain Inventory (CBPI). The LOAD questionnaire offers a useful explanation of how its findings can be incorporated into clinical practice, and gives a suggestion on its interpretation with clear guidelines for the owner on how to fill out the form. It has been used in several research studies to assess the development of osteoarthritis following surgical intervention (Renwick et al, 2018; Biskup and Conzemius, 2020; McCarthy et al, 2020a, 2020b). A review of three different client metrology instruments, including the LOAD and CBPI, found that the LOAD provided the most consistent results at baseline (Muller et al, 2016). Permission for use of the LOAD questionnaire should be sought from Elanco (Elanco Animal Health, Hook, England), but it is free to use. The CBPI can be downloaded from the University of Pennsylvania web portal (Brown, 2017). The LOAD and HCPI have a similar format in which the owner is asked a series of questions related to their dog's activity and mobility and given a 5-point rating scale for each question. A score is assigned to each answer and the total score calculated. The CBPI uses an 11-point scale with questions focused on how the owner perceives their dog's pain and how this pain is interfering with their dog's function. A user guide for the CBPI is currently being updated. The previously reported scoring system averaged the answers on pain severity for one score, and took the mean of the answers to the six questions relating to how pain interferes with the patient's daily functions for a second score (Brown, 2017).
Diagnosing osteoarthritis
Osteoarthritis in dogs is typically secondary to an underlying joint abnormality such as hip laxity or previous fracture (Langenbach et al, 1998). Investigation for such abnormalities will typically include a thorough orthopaedic examination and radiographs of the affected joint. If the stifle joint is affected then common, potentially surgical, conditions such as patella luxation and cranial cruciate ligament rupture, should be ruled in or out before instituting a treatment plan consisting of osteoarthritis management alone. In some cases, the patient may not be a candidate for pursuing a radiographic diagnosis, so a detailed history, the patient's signalment and a thorough orthopaedic examination will often lead to a presumptive diagnosis of osteoarthritis. A clinical metrology instrument could be used as a diagnostic tool aid in these cases. Although the LOAD questionnaire has not been validated as a diagnostic tool specifically, it does provide an overall score out of 52, with a scale for interpretation of the score in correlation to expected osteoarthritis level in the patient. This score is very useful in the clinical setting, as it can be used to provide the owners with a visual representation of the severity of their pets' disease (Figure 1).
Monitoring osteoarthritis
Several studies in dogs have shown that the patient's canine metrology instrument score decreased following institution of analgesia (Brown et al, 2007, 2013; Hielm-Björkman et al, 2009; Walton et al, 2013). Owners should therefore be asked to retake the chosen canine metrology instrument when they return for a recheck appointment following instigation of management and treatment of osteoarthritis. Hopefully seeing an improvement in their pet's score will help to encourage continued compliance. The LOAD questionnaire conveniently has a separate follow-up form which is shorter but gives the same overall score to allow direct comparison to the previous results. Although specific guidelines on how much the score should be expected to change have not been issued, the interpretation chart can help contextualise the change numerically for the owner. For the CBPI, a reduction of ≥ 2 in pain interference score and ≥ 1 in pain severity score has been suggested to define treatment success in clinical studies (Penn Vet, 2021). In the author's opinion, the LOAD questionnaire provides the most convenient, user friendly and clinically applicable client metrology instrument which is readily accessible to all to use, which will hopefully encourage owner participation so that ongoing data collection is possible.
Gait analysis
Gait analysis using force plates can also be used for monitoring a patient's response to osteoarthritis management. Force plates measure the overall ground reaction force of the limb which is not specific to any one joint (Spencer et al, 2018). A strong, direct correlation between a lower score on a client questionnaire and an increased peak vertical force on gait analysis has not been found (Brown et al, 2007, 2013; Hielm-Björkman et al, 2009; Walton et al, 2013). It is postulated that this is because of the effect on overall behaviour that chronic pain exerts, which cannot be completely assessed by gait analysis alone, particularly when multiple limbs are frequently affected (Brown et al, 2013). Therefore, for complete assessment of patients with osteoarthritis, it is likely advantageous to use one of the previously discussed questionnaires and it is not necessary to consider implementing a gait analysis system in general practice.
Client metrology instruments for felines
For feline patients there are numerous different client metrology instruments available. A six-question checklist has been developed for use in the clinic to screen cats for pain related to osteoarthritis (Enomoto et al, 2020). Unfortunately, the sensitivity of this checklist fell to 59% if the owner was previously unaware that their cat had osteoarthritis (Enomoto et al, 2020). The change in sensitivity may result from the phrasing of the questions which, for example were ‘does your cat jump up normally?’ (Enomoto et al, 2020). Without client education on the differences between a normal cat jumping and an osteoarthritic cat jumping, it appeared that owners were not able to differentiate a change from normal. This highlights the importance of owner education about osteoarthritis as this will in turn help to improve their ability to detect in their own pet. This checklist could be incorporated into clinical practice as an aid to screening but should be used in conjunction with a full history, physical and orthopaedic examination findings. Other client metrology instrument options for felines, that have been rigorously tested for their ability to assess chronic pain and osteoarthritis in cats, are the Feline Musculoskeletal Pain Index and the use of client-specific outcome measurements (Bennett and Morton, 2009; Benito et al, 2013). The Feline Musculoskeletal Pain Index has been validated for diagnosing and monitoring of chronic pain in cats resulting from osteoarthritis (Benito et al, 2013). It is available to use for free following a simple online registration via painfreecats.org. There are not yet any specific guidelines on how to specifically interpret the score, but their website states that they are currently undertaking this research. The website also contains an explanation on the aims of the tool, how to use it and a useful section of frequently asked questions relating to pain, lameness and osteoarthritis in cats (Duncan and Lascelles, 2018). An advantage to this client metrology instrument is that the owner can log on at their own convenience to complete further questionnaires and monitor a change in score.
The client-specific outcome measurements ask owners to consider whether specific activities related to their cat such as jumping, playing, grooming and general attitude are normal or abnormal, and rate the severity of any abnormalities (Bennett and Morton, 2009). Research comparing client-specific outcome measurements to accelerometer data has shown that owners are able to detect changes in their cat's behaviour associated with the administration of non-steroidal anti-inflammatory drugs (Lascelles et al, 2007). As client-specific outcome measurements have been further researched they has been modified to include just three activities. A change in these allows detection of clinically relevant pain relief in cats with pain caused by osteoarthritis (Gruen et al, 2014). The advantage of client-specific outcome measurements is that it can be individualised for the patient, allowing the owner to look for behaviours that they are able to observe their cat performing. To use client-specific outcome measurements, the client is asked to select three activities in which they feel their cat is impaired in. Most commonly, owners report changes in their cats' ability to jump, go up and down stairs smoothly and in their gait. Changes in overall activity level and perceived mood are also commonly noted in cats with musculoskeletal disease (Klinck et al, 2012). An overall score is calculated based on a 5-point integer scale for each activity. During monitoring of response to treatment, a change of 2 or more in the score has been shown to correlate with changes in the chronic pain status of cats (Gruen et al, 2014).
It may be helpful to combine the checklist, client-specific outcome measurements and Feline Musculoskeletal Pain Index in clinical patients with osteoarthritis. For example, many clinics run geriatric cat clinics for those over the age of 8 years old, so clients could be asked to fill out the six-question checklist while waiting for their appointment. Once osteoarthritic patients have been identified the client-specific outcome measurements can be explained and clients can be encouraged to explore the Feline Musculoskeletal Pain Index at home as the website provides plentiful information and instruction on how to fill this out. Clients can then be encouraged to fill out the Feline Musculoskeletal Pain Index from their homes at regular intervals to allow monitoring of response to treatment. When they come back to the clinic for recheck appointments the client-specific outcome measurements can be repeated so a full overview of the patient's chronic pain status can be gained.
Conclusions
Although definitive diagnostic cut-offs have not yet been established for most of these questionnaires, just as clinicians gain experience with interpretation of clinical examination findings, by using these client metrology instruments frequently, clinicians will gain experience in their interpretation. The availability of these questionnaires online allows owners to complete them in their homes before appointments, in between appointments, in the waiting room and/or during the appointment itself. The satisfaction of seeing the scores reduce as management practices are instituted helps keep clients engaged and motivated and provides job satisfaction and reassurance to the clinician. Most importantly, they provide accurate data on patient outcomes and can therefore improve patient welfare.


