Malnutrition strictly refers to both under-nutrition and over-nutrition (obesity). However, it is malnutrition secondary to disease that most commonly causes under-nutrition. Malnutrition is usually associated with chronic diseases such as neoplasia, gut disease (such as inflammatory bowel disease or protein-losing enteropathies), kidney disease (such as chronic kidney disease or protein losing nephropathies) and liver disease (such as chronic hepatitis or chronic liver failure). However, severe acute diseases (including trauma, acute kidney injury, septic peritonitis, pancreatitis) can also lead to malnutrition.
A consensus publication by the Global Leadership Initiative on Malnutrition (GLIM) proposed both phenotypical and etiological criteria to diagnose malnutrition in people (Cederholm et al, 2019). Specifically, at least one phenotypical criterion (weight loss, low body mass index, reduced muscle mass) and one aetiological criterion (reduced food intake or assimilation, inflammation) must be present in a patient to make a diagnosis of malnutrition. Furthermore, the consensus statement recommended grading the severity of malnutrition based on the magnitude of the three phenotypical criteria (weight loss, low body mass index, reduced muscle mass).
The metabolism of illness
Sick animals undergo processes called stressed starvation, during which certain metabolic derangements can lead to malnutrition. These processes include:
- Increased energy expenditure (mediated via inflammatory cytokines, catecholamines)
- Increased fat mobilisation
- Increased and preferential muscle catabolism
- Hyperglycaemia caused by insulin resistance and other factors.
In contrast, animals undergo simple starvation when not ill (such as when food is scarce). Compared to stressed starvation, with simple starvation there is reduced energy expenditure (mediated via thyroid hormone) and preferential fat use to preserve the muscle mass.
Identifying malnutrition in dogs and cats
Currently, there are no recognised classification or grading systems for malnutrition in animals. For this reason, the criteria used in human medicine are often extrapolated (Table 1). Other factors associated with malnutrition include poor hair-coat quality, inadequate wound healing, coagulopathy, lymphopenia and hypoalbuminaemia.
Table 1. Key indicators of malnutrition in dogs and cats
| Indicator | Clinical assessment | Objective assessment |
|---|---|---|
| Weight loss | Review of clinical notes | Daily weight recordings in hospitalised patients |
| Body fat loss | Body condition scoring | Dual x-ray energy absorptiometry |
| Muscle wasting | Muscle condition score | Computed tomography or ultrasound |
| Reduced appetite | Estimation based on information from owners | Food measurement and calorie calculation in hospitalised patients |
| Inflammation | Clinical signs (such as pyrexia) | Neutrophilia, increased C-reactive protein and other inflammatory markers |
Bodyweight loss
Weight loss is often an easily identified abnormality in veterinary patients, as bodyweight measurement is common in veterinary practice. In addition to this, there is also usually historical information regarding bodyweight from when the animal was healthy (for example, at vaccination appointments). This can serve as a comparative healthy weight yardstick for each patient. For hospitalised patients at risk of malnutrition, daily recordings of bodyweight (using the same set of scales to minimise variability) can provide useful information about a patient's progress.
In people, more than 5% loss of bodyweight within 6 months, or greater than 10% weight loss beyond 6 months, is considered consistent with malnutrition (in conjunction with other criteria) (Cederholm et al, 2019). Severe (stage II) malnutrition is categorised by a greater than 10% weight loss within 6 months, or greater than 20% weight loss beyond 6 months.
Weight loss can be a common feature of many diseases in dogs and cats where malnutrition typically occurs. In one study of dogs with cancer, 69% of dogs lost weight, and 23% of dogs lost greater than 10% bodyweight (Michel et al, 2004). Similarly, weight loss in feline cancer patients is also common (Baez et al, 2007).
Body fat loss
The gold standard of body fat assessment is dual X-ray energy absorptiometry (DEXA). Although this imaging modality is available in veterinary medicine, it is not usually used in a clinical setting but rather for research purposes. This imaging modality provides information about the patient's body fat content, muscle mass and bone density.
In the GLIM classification system for malnutrition in people, low body mass index (BMI) is cited as a phenotypical criterion. Specifically, a BMI of less than 20 is considered consistent with malnutrition (Cederholm et al, 2019). However, there are some geographical differences listed, for example in Asia the cut-off BMI is less than 18.5, and in North America BMI is used less often as it underestimates fat loss in obese patients.
Although morphometric analyses such as BMI are not used in dogs and cats, body condition scoring is commonly used to identify patients who are over- and underweight. Some of these scoring systems (such as the 9-point system recommended by the World Small Animal Veterinary Association) have been validated against DEXA scanning (Mawby et al, 2004).
Body condition scoring allows veterinarians to assess and semi-quantify the body fat mass. Dogs and cats are graded into one of nine categories, with 5/9 being ideal for cats and scores of 4 and 5 considered ideal for dogs (Figures 1 and 2). Each integer score below the ideal presents 10–15% loss of body weight (and 5% loss of body fat) compared to the ideal. Although some interobserver variation may occur between veterinarians performing the scoring, this method provides a quick and free assessment of the patient's fat mass and body shape.


Body condition scoring is particularly important in dogs, where there can be large variations in natural body size. However, similarly to in humans body fat loss may be underestimated in obese dogs and cats (malnutrition may be more difficult to detect in an obese dog or cat). In addition to this, some breed variations may also effect scoring (as an example, sight hounds are considered leaner compared to other breeds).
Muscle wasting
Muscle wasting associated with illness (cachexia) is arguably the most important aspect of malnutrition. This criterion has strong evidence to support its inclusion in the GLIM consensus. However, there is some debate in human medicine about the best method of assessing a patient's muscle mass. In addition to this, assessment of muscle function is also recommended in people. Loss of muscle mass and function not only affects the appendicular muscles; cardiac, respiratory and oropharyngeal muscle groups can also be affected, sometimes with devastating effects.
The measurement of muscle mass in dogs and cats can be performed using DEXA or other imaging modalities. Computed tomography can be used to measure the muscle mass at a standardised point (for example, the lumbar spine using the vertebrae as a reference point) (Sutherland-Smith et al, 2019). Ultrasonography can also be used to measure the muscle mass in certain points of the body (Bullen et al, 2017).
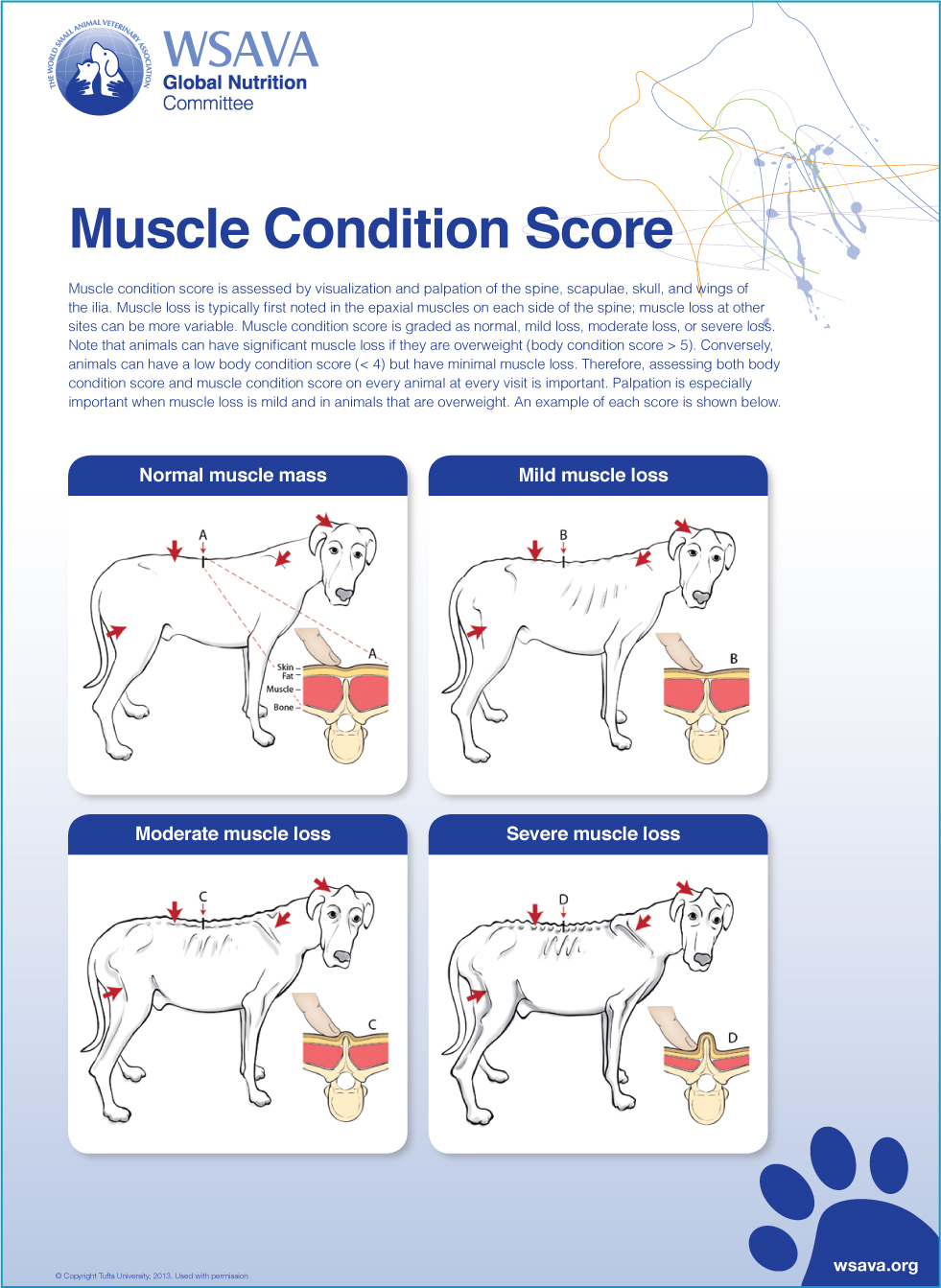
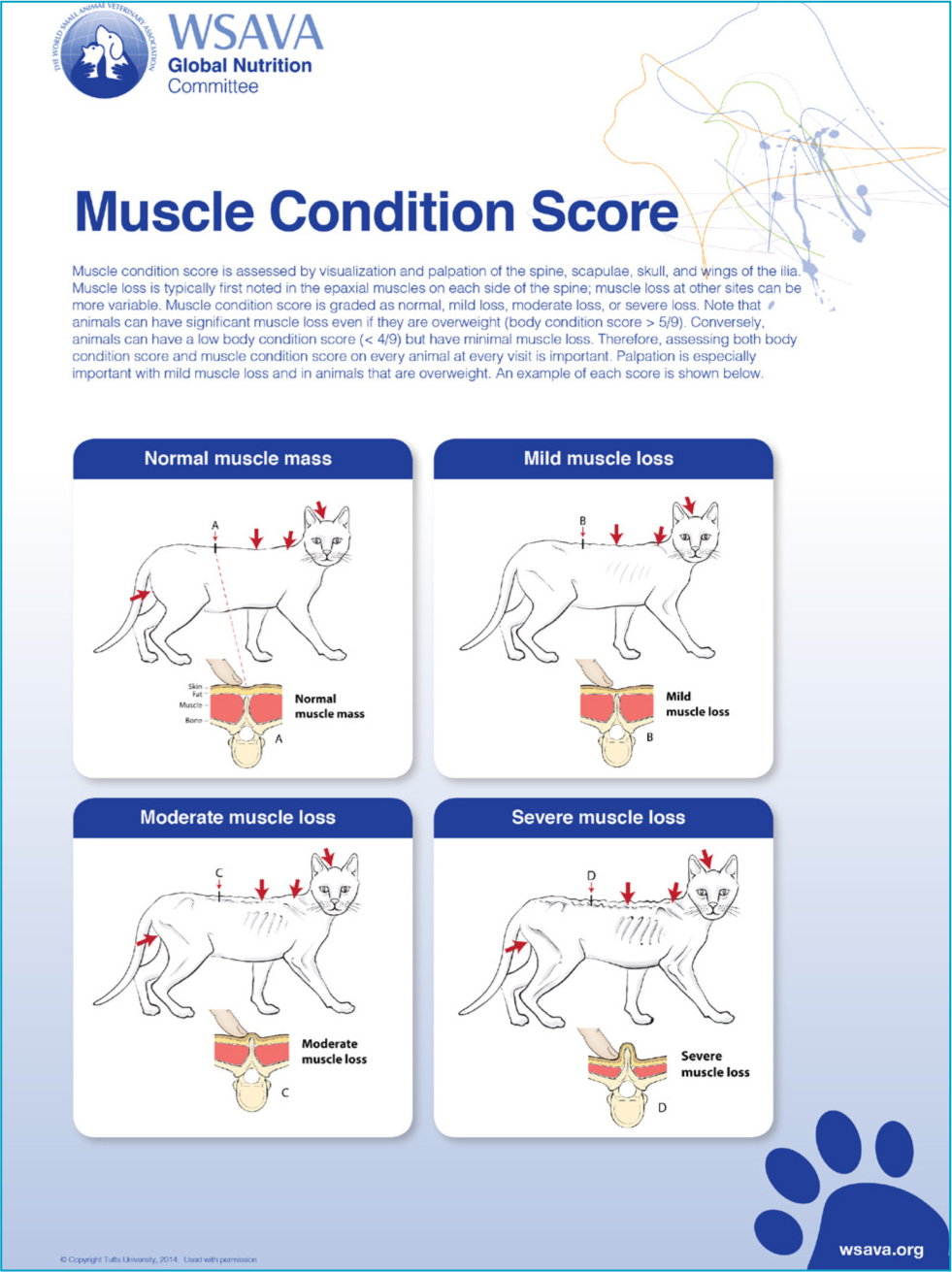
Objective measurements of the muscle mass are rarely performed in a clinical setting. For this reason, a qualitative muscle condition scoring system has been developed to assess the muscle mass, independent of the fat mass (Cline et al, 2021). This scoring system assesses the muscle mass at four different sites in the body and categorises it from normal to mildly, moderately or markedly wasted (Figures 3 and 4). It is worth noting that appreciating muscle wasting in obese patients can be challenging.
Causes of malnutrition
Reduced food intake or assimilation
The GLIM consensus statement lists reduced food intake (eating up to 50% of the energy requirement over one week, or any reduction in appetite for over 2 weeks) in people as a cause of malnutrition (Cederholm et al, 2019). In addition to this, malabsorptive gut disorders are also thought to contribute to malnutrition.
Inappetence and anorexia are common complaints in sick dogs and very common in ill cats. There can be a number of causes for this, including factors related to underlying disease (particularly if the disease affects the gastrointestinal system), the secondary physiological effects (for example, appetite suppression caused by inflammatory mediators), effects related to treatment (such as adverse effects of medication), food aversion (caused by pain or stress) and environmental factors (such as the location of food, use of Elizabethan collars). It should be noted that in some dogs and cats, malnutrition may occur despite the presence of a normal appetite.
Inflammation
Inflammation is a key component of many diseases, even when the primary cause may not be considered an inflammatory disorder (such as trauma or neoplasia). Thus, it is not surprising that inflammation, particularly when severe, chronic or recurrent in nature, has been linked to malnutrition in people. Surrogate markers of inflammation (including C-reactive protein, albumin and pre-albumin) are often used in people to assess malnutrition risk (Cederholm et al, 2019).
Inflammatory biomarkers such as C-reactive protein are now increasingly being used in veterinary medicine. This is in addition to other more common aberrations, such as those noted on complete blood count (such as neutrophilia or lymphopenia) and protein alternations of serum biochemistry. A study by Pointer et al (2013) of dogs that were malnourished as a result of starvation identified hypoalbuminaemia, anaemia, thrombocytosis, increased blood urea and hypocalcaemia as the most common clinicopathological abnormalities. Of these, anaemia and hypoalbuminaemia were thought to be particularly clinically important.
Consequences of malnutrition
There is clear evidence that malnourished people have poorer outcomes in a number of diseases. There is similar evidence in canine and feline medicine to support the notion that malnourished patients have a worse outcome. For example, in one study of cats with cancer, cats with a body condition score of 4/9 or less had a median survival time of 3.3 months compared to 16.7 months in cats with a body condition score of 5/9 or higher (Baez et al, 2007). Similarly, Pedrinelli et al (2020) showed that dogs with chronic kidney disease that had a subnormal body condition score compared to overweight and obese dogs had a poorer outcome. This study also showed that a low muscle condition score was significantly associated a poor prognosis in canine chronic kidney disease.
Management of malnutrition
Supportive care and medical treatment
The management of malnutrition often requires a therapeutic intervention such as a feeding tube or administration of parenteral nutrition (Table 2). Use of supportive therapies may only help improve the appetite in a small percentage of cases. These measures may include fluid therapy to correct fluid, electrolyte or acid-base deficits, as well as analgesia and anti-emetic medications. In addition, techniques such as warming food and using different textures may also encourage voluntary consumption of food. Patients managed conservatively should be carefully monitored for quantifiable improvements in food consumption, so that an enteral or parenteral intervention can be implemented if there is a poor response.
Table 2. Nutritional interventions to manage malnutrition in dogs and cats
| Advantages | Disadvantages | |
|---|---|---|
| Appetite stimulants and other medical/supportive therapies | Cheap, readily available, easy to administer | Potentially ineffective, adverse effects |
| Naso-oesophageal feeding tubes | Anaesthesia not required, provide partial enteral nutrition | Not tolerated in long-term, liquid diet only |
| Oesophagostomy feeding tubes | Well-tolerated, low adverse effects, medium to long-term support, able to use liquidised canned diets (rather than liquid convalescence diets) for specific conditions | Requires general anaesthesia, not suitable if coagulopathic, not suitable for many oesophageal diseases |
| Gastrostomy feeding tubes | Well-tolerated, bypasses oesophageal pathology, reduces risk of regurgitation and aspiration, long-term use possible | Requires general anaesthesia and endoscopy or surgery, serious complications possible (e.g. septic peritonitis) |
| Jejunostomy feeding tubes | Ideal for limited scenarios requiring post-pyloric feeding | High risk of feeding related complications, serious adverse effects possible (e.g. septic peritonitis), requires expensive elemental diets |
| Parental nutrition | Only option when enteral feeding not tolerated, in conjunction with partial enteral feeding | Complications (e.g. thrombophlebitis, hyperglycaemia, catheter infection), limited availability, high level of monitoring required |
Appetite stimulants are often used in veterinary medicine as a cheap and quick method to address a poor appetite. The most commonly used medications include mirtazapine (mainly used in cats) and capromorelin (in North America), although these medications are unlikely to be effective in moderate to severe disease. Some of these medications (such as mirtazapine) can also cause adverse effects, especially in cats with compromised organ function.
Feeding tubes
The provision of enteral nutrition via a feeding tube is often the most effective way to address malnutrition in dogs and cats. The possible tube options include: naso-oesophageal, oesophagostomy, gastrostomy or jejunostomy feeding tubes. Oesophagostomy feeding tubes are often the best option as they are safe and have low rates of complications, versatile (can be used with liquid diets or liquidised canned diets) and these can be used for a reasonable time period (3-4 weeks or longer). Naso-oesophageal feeding tubes are generally poorly tolerated in the long-term, but can be useful for short-term nutritional support, particularly in critically ill patients needing stabilisation before general anaesthesia. Gastrostomy feeding tubes are generally reserved for patients requiring by-pass of oesophageal pathology (such as oesophagitis or megaoesophagus), in large dogs (where an oesophagostomy feeding tube may be challenging to place) or with chronic disease. Jejunostomy feeding tubes are rarely used and are usually reserved for patients that require bypass of the proximal gastrointestinal tract.
Parenteral nutrition
Even though parenteral nutrition is used in people to manage chronic diseases (including home parenteral nutrition), in veterinary patients this nutritional intervention is typically only used for short-term management of critically ill patients. The main drawbacks associated with this form of nutrition are the cost and expertise needed to safely administer the solutions and monitor for possible adverse effects. For this reason, parenteral nutrition is typically currently used only at referral institutions. In addition to this, parenteral feeding alone (without concurrent enteral feeding) can lead to gut dysfunction, including enterocyte atrophy and increased bacterial translocation.
Calorie and nutrient requirements in malnutrition
The provision of adequate calories is the most important aspect of feeding in malnutrition (Table 3). More often than not, this requires an enteral or parenteral feeding intervention. The energy requirements of ill animals are usually estimated using mathematical formulae, rather than measured using methods such as indirect calorimetry. Estimations of energy requirements can inherently lead to inadequate or excessive provisions; so careful monitoring is always needed.
Table 3. Key nutrients to address malnutrition in dogs and cats
| Reasons for requirement | Amount needed | Precautions and adverse effects | |
|---|---|---|---|
| Calories | Correct energy deficit | To meet resting energy requirement | Risk of complications from over-feeding or refeeding syndrome if provision excessive |
| Protein | Provide essential and conditionally essential amino acids, counteract muscle wasting (cachexia), provide energy | Moderate to high | Take care if protein intolerance present, such as in kidney disease |
| Fat | Provide energy, essential fatty acids, fat soluble vitamins | Moderate to high | Take care if fat intolerance present, such as fat malabsorption diarrhoea, as this can worsen gastroparesis caused by ileus |
| Vitamins | Especially water soluble B-vitamins as body stores likely inadequate | Moderate to high | None with a balanced diet |
| Minerals | Especially macro-minerals (sodium, potassium, calcium, magnesium, phosphorus) to prevent refeeding syndrome | Moderate to high | Specific mineral intolerances, such as phosphorus with kidney disease |
Although there may be a willingness to feed aggressively to slow declining body condition, this approach can be harmful owing to the metabolic derangements associated with overfeeding. For this reason, a more conservative feeding plan is recommended (aiming to meet the resting energy requirements of the patient slowly over 3–5 days). This amount can then be gradually increased to achieve the desired target body condition score (Figures 3 and 4).
After calories, protein is probably the most important nutrient in dogs and cats that are malnourished; the protein requirement of these patients is generally high, to counteract the negative nitrogen balance associated with illness. This is particularly the case in cats who have a higher protein requirement compared to dogs as a result of their obligate carnivore metabolism. In addition to the diet being replete in protein, the protein sources should be highly digestible and contain all of the essential amino acids. Furthermore, some amino acids (called conditionally essential) are required only during illness (such as glutamine), and these should also be provided in adequate amounts.
Dietary fat and carbohydrate are also important sources of energy for the malnourished patient. Fat in particular can be very helpful in those patients with reduced voluntary consumption of food, as it is the most energy dense nutrient, althoough the adverse effects of high fat diets, such as delayed gastric emptying and fat malabsorptive diarrhoea, should be noted. Dietary carbohydrate is not considered an essential nutrient, as it does not provide vital nutrients such as those found in protein (amino acids) and fat (fatty acids), but it is an excellent source of easily digestible energy for cats and dogs. Some caution should be exercised with the amount of carbohydrate used in patients with insulin resistance or in those at risk of refeeding syndrome.
The importance of micronutrients is often ignored because of the relatively small amounts needed in the diet. However, these nutrients are vital for cats and dogs recovering from malnutrition. For example, many of the B vitamins and trace minerals have essential enzymatic and other functions, which are vital for normal metabolism. The minerals needed in the largest amounts in food (sodium, phosphorus, calcium, magnesium, chloride and potassium) serve several vital roles, including maintaining serum osmolarity, membrane integrity and muscle function. Trace minerals are needed in the smallest amounts, but these nutrients still play major roles, including iron for haemoglobin and selenium for anti-oxidant function.
Diets used to manage malnutrition
An ideal diet used to manage malnutrition should be:
- Nutritionally complete and balanced
- Highly palatable (if for voluntary feeding)
- Appropriate for physiological needs (growth)
- Species specific
- Cooked, to prevent risk of microbial infection
- Calorie dense
- Highly digestible
- High in protein (80–100 g per 100 kcal), including a complete amino acid profile.
Good food choices for both cats and dogs include convalescence diets and intestinal diets. Convalescence diets tend to be calorific with high protein and fat contents and lower carbohydrate contents, and intestinal diets are usually high in protein and highly digestible. There are fewer options for puppies and kittens but some convalescence, intestinal and hydrolysed diets are balanced for growth. Home-cooked diets can also be high in protein and highly digestible, but these require formulation by a board-certified veterinary nutritionist to ensure the diet is balanced. Owing to the formulation, preparation and supplementation required with home-cooked diets, these are usually used only when commercial diet options have been exhausted.
Complications associated with feeding malnourished patients
The rapid re-introduction of food after a prolonged period of starvation can lead to a phenomenon known as refeeding syndrome. This is caused by the rapid intra-cellular shift of key electrolytes (calcium, magnesium, sodium, potassium, phosphorus) in response to the re-introduction of food. The resultant sudden and severe electrolyte disturbances can cause a number of life-threatening complications including haemolytic anaemia (caused by hypophosphatemia), cardiac arrhythmia (hypokalaemia, hypocalcaemia, hypomagnesaemia), seizures (hypocalcaemia) and peripheral oedema (hyponatremia). Refeeding syndrome is best prevented by slow reintroduction of food (over 3–5 days) after prolonged starvation and careful monitoring and intravenous supplementation of key electrolytes (phosphorus and potassium).
Other more common yet less severe complications associated with feeding include: vomiting and diarrhoea (after introduction of enteral feeding), regurgitation (from delayed gastric emptying) and metabolic complications associated with parenteral nutrition (such as hyperglycaemia, azotaemia).
Prevention of malnutrition
The prevention of malnutrition is highly dependant on the awareness of this disorder and ideally access to a scoring system similar to the GLIM criteria used in people. In dogs and cats, malnutrition can occur in both acute severe diseases (or as a result of trauma or sepsis), as well as in chronic medical disorders (such as inflammatory bowel disease, chronic kidney disease or neoplasia). In susceptible patients, careful questioning of the owners is necessary to highlight and quantify reductions in food consumption. It is also important to review the patient's bodyweight compared to its historical weight. Physical examination, including body condition and muscle condition scoring should then be performed. Finally, diagnostic testing, including blood tests for inflammation, may be necessary.
In patients with evidence of or risk factors for malnutrition, proactive steps should be taken to address this. These steps usually include placement of a feeding tube (or starting parenteral nutrition in some cases). For example, a patient with septic peritonitis undergoing surgery should have a feeding tube placed so that enteral nutrition can be provided in the postoperative period.
Conclusions
Malnutrition can be a serious and devastating complication of chronic and acute illness in people. The recent GLIM criteria have highlighted the importance of this problem and have enabled medical professionals to diagnose and categorise malnutrition in people. It is likely that the prevalence of malnutrition in cats and dogs is underestimated in clinical practice. To address this, it is important for veterinarians to be familiar with this condition. By assessing patients for weight loss and by performing body and muscle condition scoring, dogs and cats at risk for malnutrition can be identified. These patients can then have a suitable nutritional support plan implemented to address the cause of malnutrition.
KEY POINTS
- Malnutrition in dogs and cats may manifest with bodyweight, fat and muscle loss, in conjunction with systemic inflammation and reduced food consumption.
- Assessment for malnutrition in susceptible patients requires careful historical review, physical examination (including body and muscle condition scoring) and diagnostic tests (blood tests).
- The key nutrients needed to address malnutrition include calories, protein, fat and micronutrients.
- Malnourished patients are best treated with feeding tubes and parenteral nutrition, because other methods (such as appetite stimulants) are usually less effective.

