Ixodes species ticks are abundant this spring and summer with temperatures and humidity ideally placed for tick activity. Lyme disease remains the most common Ixodes-transmitted pathogen of veterinary significance, affecting dogs, cats and people. However, in the past month attention has been drawn to two other Ixodes-associated pathogens causing cases of human disease. A human case of babesiosis caused by Babesia venatorum has been recorded in the UK for the first time, alongside only the second UK case of tick-borne encephalitis.
Babesiosis caused by Babesia venatorum
There are several Babesia spp. present in the UK, with Babesia canis transmitted by Dermacentor reticulatus the most pathogenic in dogs. Other Babesia spp. transmitted by Ixodes spp. ticks, while less pathogenic in pets, are zoonotic. B. venatorum is notable in that it appears able to infect humans without immune suppression or splenectomy, and resultant disease can be more severe than in other zoonotic Babesia spp. (Herwaldt et al, 2003).
Since it was first found in UK ticks by Smith and Wall (2013), evidence has been building regarding its presence in the UK. It has been found by polymerase chain reaction (PCR) in Scottish sheep (Gray et al, 2019), in 1.26% of ticks on dogs (Abdullah et al, 2018) and 0.37% of ticks found on cats (Davies et al, 2017). However, there had not been a human case identified in the UK until July this year, when an individual in Devon was hospitalised and infection confirmed. Despite hundreds of ticks in the area being tested, none were found to be carrying B. venatorum. This is not surprising given the low percentage of infection previously found in ticks, but gives no indication of geographical risk or why the first UK human case has taken so long to emerge. This case may be an isolated incident, have been detected because of increased awareness of babesiosis in humans, or may have occurred as a result of shifting epidemiological factors. Ticks are now more active throughout the summer and increasing in numbers (Figure 1) (Wright et al, 2018). Increased green space and outdoor recreational activity is also thought to be bringing the public into closer contact with ticks. This case should therefore be taken seriously but also kept in perspective when compared with the number of human cases of Lyme disease confirmed in the UK each year (2.7 cases per 100 000 people in 2017).

Tick-borne encephalitis caused by tick-borne encephalitis virus
Ixodes ricinus is also a vector for tick-borne encephalitis virus (TBEV) which can cause a potentially fatal neurologic disease known as tick-borne encephalitis (TBE) in humans and, less commonly, dogs. The European subtype of the virus has rapidly spread across central and western Europe in recent years, raising concerns it might establish here in the UK. A surveillance programme carried out by Public Health England in 2018 found 4% of UK deer samples to be serology positive for TBEV with foci in the New Forest and Thetford Forest. The Thetford Forest area had the highest proportion (47.7%) of seropositive samples with a tick also confirmed positive for TBEV by PCR (Holding et al, 2020). This is strong evidence for TBEV being endemic in at least one focus in the UK. Since then, there have been two human cases of human TBE in Hampshire. Although the parasite currently appears to be limited to two UK foci, others may be present and spread via infected ticks on deer, people and pets seems likely.
How B. venatorum and TBEV have been introduced to the UK is uncertain but ticks attached to migratory birds, travelled pets or livestock are all possibilities. Media coverage of both of these infections is likely to make pet owners concerned for both their and their pet's welfare. Veterinary professionals continue to play a vital role in giving evidence-based advice regarding tick-borne disease. The risk to dogs and their owners from these new pathogens is low and should be kept in perspective. However, tick protection for pets and public engaging in outdoor activities is important to minimise risk of exposure.
Tick prevention for pet owners
Public Health England's tick prevention advice for the public is to:
- Keep to footpaths and avoid long grass when out walking
- Wear appropriate clothing such as a long-sleeved shirt, and trousers tucked into your socks, to make it less likely that a tick will bite and attach
- Consider the use of repellents
- Make it a habit to carry out a tick check regularly when you are outdoors and when you get home
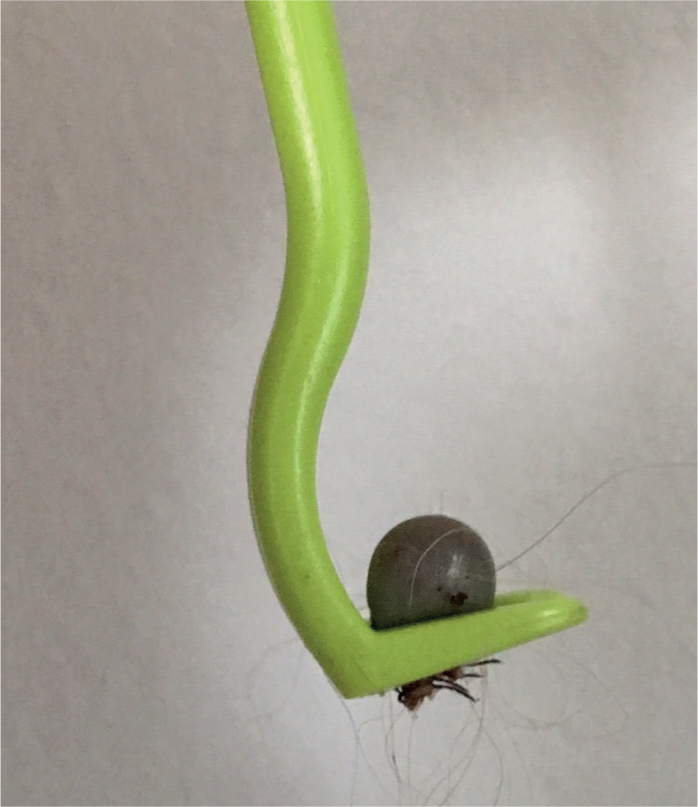
- If you have been bitten by a tick, remove it as quickly as possible, using fine-tipped tweezers or a tick removal tool (Figure 2)
- Contact your GP promptly if you begin to feel unwell, remembering to tell them you were bitten by a tick or recently spent time outdoors.
Tick prevention for pets
Protection for pets should consist of a preventative product and checking for ticks at least every 24 hours. Products containing an isoxazoline or pyrethroid all fulfil these criteria. With the exception of Seresto®, pyrethroid products must never be used on cats because of the resultant toxicity. Although highly efficacious, no tick prevention product is 100% effective and challenge in some geographical foci can be very high. Latest tick surveillance scheme data suggest that the majority of ticks are located and found around the head, face, legs and ventrum (Wright et al, 2018). Ticks should be removed with a tick removal device or fine-pointed tweezers. If tweezers are used the tick should be removed with a smooth upward pulling action. If a tick hook is used, then a simple ‘twist and pull’ action is employed.

