Fleas are considered to be the most important ectoparasite of dogs and cats (Abdullah et al, 2019). They have impressive reproductive capabilities, as well as an ability to persist in the environment and act as pathogenic vectors. Of the 2500 species worldwide, Ctenocephalides felis felis (cat flea), Ctenocephalides canis, Pulex simulans and Echidnophaga gallinacea are seen as significant, because of their ability to infest companion animals in large numbers (Blagburn and Dryden, 2009). Of the aforementioned species, the cat flea is the most dominant, and is found parasitising cats and dogs.
The blood-feeding behaviour of fleas causes direct irritation, resulting in intense pruritus and, in cases of severe infestation, anaemia (Taenzler et al, 2014). Repeated exposure can lead to the development of flea allergy dermatitis in both dogs and cats (Dryden et al, 2013a) and it is estimated that 50% of dermatological cases in dogs are associated with fleas (Beugnet et al, 2012). Flea allergy dermatitis is caused by an exaggerated immune response to fleas' salivary antigens, injected during feeding, which leads to hypersensitivity. If left untreated, skin changes attributed to self-trauma can occur, such as alopecia or crust formation (Stanneck et al, 2012).
As well as having direct effects on an animal itself, fleas can act as vectors for a range of zoonotic pathogens. Cat scratch disease is caused by the bacterium Bartonella henselae, which is spread among cats by C. felis. Transmission to humans occurs when flea faeces containing the bacteria are scratched into bites or wounds (Rust, 2017). C. felis has also been responsible for the transmission of the bacteria Rickettsia typhi and Rickettsia felis via flea bites, causing acute febrile illness in humans (Nelson et al, 2018). In addition, fleas are the intermediate host in the life cycle of the tapeworm Dipylidium caninum. Dogs and cats become infected when they ingest fleas containing the cysticercoids and humans, mostly children, become infected when they accidentally swallow a flea infected with the cysticercoid.
Numerous antiparasitic drugs targeting fleas, known as adulticides, pulicides or insecticides, are available on the market for use in companion animals. Insecticides can be administered orally, topically or subcutaneously. Some topical preparations work directly on the skin surface, while others are absorbed transdermally into the circulation to work systemically. Molecules that work on the nervous system of the adult fleas are known as adulticides, whereas molecules that interfere with egg development or other off-host life-cycle stages are termed insect growth regulators, or insect development inhibitors (Marchiondo et al, 2013). Over the past few decades the discovery of new molecules, combinations of different insecticides in products and the availability of different formulations have expanded the anti-flea product market significantly (Taenzler et al, 2016).
One important advancement in flea control combines adulticides and the ovicidal and larvicidal effects of insect growth regulators for use on both animals and environment (Ritzhaupt et al, 2002). Interruption of the flea life cycle at multiple stages inhibits flea reproduction and prevents the population from being maintained (Rust, 2017). Non-chemical measures, such as vacuuming and washing infested bedding at 60°C, mechanically remove eggs, larvae and pupae. Although it is adult fleas that pose a direct problem to the host, most of the flea population is composed of the immature stages found in the home. If this population is not eradicated, any adult fleas killed on the animal will be replaced (Perrins and Hendricks, 2007; Elsheikha and Wright, 2014).
When flea treatments fail, it is most likely a result of either the the pet owner's behaviour or the product's performance (Halos et al, 2014). Poor performance could be caused by drug inefficacy, for instance flea resistance, innate reduced susceptibility or reduced residual speed of kill. If residual activity of a product is not sufficient to last until the next application, fleas will continue to reproduce and control will break down (Wright, 2016). Previous studies on treatment failure have mainly focused on resistance or reduced susceptibility to older insecticides. Resistance of C. felis to organophosphates, carbamates and pyrethroids has been reported (Bossard et al, 2002; Coles and Dryden, 2014). Although reduced susceptibilities of certain C. felis strains to imidacloprid and fipronil have been documented, there is little evidence to suggest that resistance is widespread in the field. Resistance has not yet been demonstrated in newer formulations (Rust et al, 2018).
There is often an assumption on the part of owners that attributes treatment failure to poor drug efficacy (Beck et al, 2014). However, a successful flea control programme involves the removal of fleas from the infected host and environment (Perrins and Hendricks, 2007) and owner adherence to drug administration at regular intervals is essential to preventing reinfestation (Halos et al, 2014; Fink et al, 2016). Non-adherence can result in suboptimal pharmacotherapy and potentially treatment failure (Lavan et al, 2017).
The present study was conducted to establish whether common flea products used in dogs and cats are still effective. We determined if product inefficacies are the reason behind reported treatment failure or if owners' lack of adherence to recommendations is more likely. We tested the hypothesis ‘When treatment failure occurs, perceived inefficacy of anti-flea products is caused by poor compliance’.
Literature search strategy
Searches were carried out on 30 September 2020 in MEDLINE via PubMed and CAB Abstracts (1973–present). To the authors' knowledge, there is no published data as to which flea products are purchased the most. Furthermore, in order to reflect the huge variety present, each product chosen was categorised into a different chemical class, with different methods of administration. Products were restricted to those used in both cats and dogs, under the assumption that products available to both species are more commonly purchased.
A combination of the following search terms were used: dog, cat, canine, feline, flea, Ctenocephalides, imidacloprid, Advantage®, dinotefuran, flumethrin, Seresto®, fipronil, s-methoprene, Frontline Combo®, spinosad, Comfortis®, selamectin, Stronghold®, indoxacarb, Activyl®, lufenuron, Program®, afoxolaner, NexGard®, sarolaner, Simparica®, lotilaner, Credelio®, fluralaner”, Bravecto, flea treatment, flea product, efficacy, ineffective, susceptibility, tolerance, resistance, treatment failure, attitude, adherence, compliance, motivation, preference and control failure.
Studies were separated into drug efficacy and owner compliance. Studies were included if they reported on the active ingredients used against fleas in dogs or cats, where the outcome involved evaluating the efficacy of the drug. Studies investigating other animals or the treatment of other parasites, for example nematodes, were omitted. Studies that used different combinations of drugs were also excluded. In order to reflect the most recent flea products on the market, the search was limited to studies carried out in the past 10 years. Specific flea strains are often selected for laboratory studies, which does not reflect the genetic variation that occurs in the general flea population (Dryden et al, 2013b; Snyder et al, 2015). Therefore, randomised controlled field studies were chosen as they are more likely to be representative of challenges in the home setting (Franc et al, 2014).
As studies investigating adherence specific to flea treatments were limited, the inclusion criteria were extended to encompass studies investigating factors affecting owners' adherence to preventative medication generally or specific to parasite control. Studies where compliance in relation to other drugs that were used curatively, for a short period of time, or in other animals except dogs or cats, were excluded. Only peer reviewed articles in the English language were included. Review articles, book chapters, conference papers and letters to editors were excluded.
Study findings
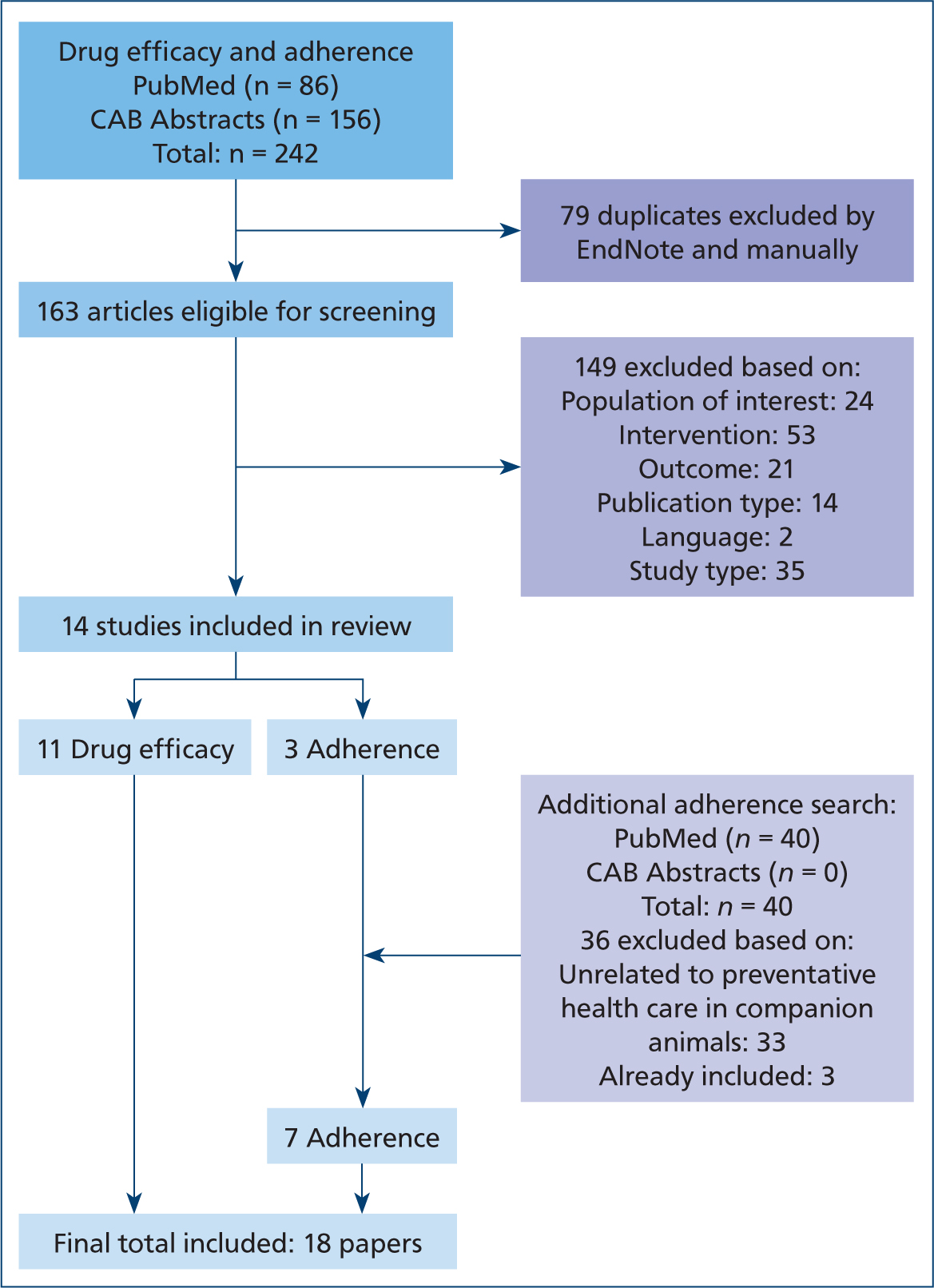
PubMed and CAB Abstracts returned a total of 242 papers. After adjusting for duplications, 163 remained. Title/abstract/full text screening excluded 149, leaving 14 papers that met the inclusion criteria. The additional adherence search returned 40 papers, of which four were included, bringing the total number of articles included in this review to 18. See Figure 1 for flow chart showing the entire selection process.
Evidence for the efficacy of flea products
To find out whether anti-flea treatments used in dogs and cats are becoming ineffective, the authors reviewed the current evidence for the efficacy of the common anti-flea products used in dogs and cats. The authors examined whether drug inefficacies are the reason for reported treatment failures or if owners' lack of adherence is more likely. The literature review search identified 11 papers on efficacy, with one paper reporting more than one study. Of the 12 studies reported, one study investigated the efficacy of indoxacarb, four for fipronil (S)-methoprene, five for spinosad, four for selamectin, two for imidacloprid + flumethrin and three for fluralaner. The main outcomes of each included study on drug efficacy can be found in Table 1. Within the 10-year limit that was applied, no randomised controlled field studies investigating the efficacy of imidacloprid or lufenuron were found.
Table 1. Percentage reduction in flea counts of treated animals compared with pretreatment values on day 0
| Products applied | Study duration (months) | Animals | Outcome | Reference | ||
|---|---|---|---|---|---|---|
| Dogs | Cats | % efficacy after 1 month | % flea free at end of the study | |||
| Dinotefuran-permethrin-pyriproxyfen | 2 | 13 | 7 | 83.62 | 60.00 | Dryden et al (2011b) † |
| Fipronil (S)-methoprene | 2 | 20 | 7 | 88.73 | 55.56 | |
| Imidacloprid + flumethrin | 8 | 291 | 94.1 + 99.0 | – | Stanneck et al (2012) * | |
| Imidacloprid + flumethrin | 8 | 165 | 99.0 | – | ||
| Spinosad | 1 | 186 | – | 97.2 | 54.5 | Wolken et al (2012) ‡ |
| Selamectin | 89.4 | 34.1 | ||||
| Spinosad | 3 | 114 | – | 97.3 | 85.0 | |
| Selamectin | 91.0 | 67.1 | ||||
| Indoxacarb | 2 | 64 | 6 | 95.0 | 77.1 | Dryden et al (2013a) † |
| Fipronil (S)-methoprene | 49.5 | 15.6 | ||||
| Spinosad | 3 | 128 | 97.9 | 94.8 | Dryden et al (2013b) * | |
| Fipronil (S)-methoprene | 78.7 | 38.2 | ||||
| Selamectin | 3 | 102 | 88.8 | 64.7 | Paarlberg et al (2013) ‡ | |
| Spinosad | 100 | 100 | ||||
| Spinosad | 3 | 30 | 97.5 | 92.6 | Saridomichelakis et al (2015) ‡ | |
| Fluralaner | 3 | 34 | 100 | 100 | Dryden et al (2016) | |
| Fluralaner (topical) | 3 | 321 | 99.8 | 93.3 | Meadows et al (2017) ‡ | |
| Fipronil (S)-methoprene | 81.2 | 30.3 | ||||
| Imidacloprid + flumethrin | 12 | – | – | 91.7 | Otranto et al (2017) | |
| Fluralaner (topical) | 3 | – | 204 | 98.5 | 100 | Dryden et al (2018) ¶ |
| Selamectin | 77.8 | 38.5 | ||||
: flea counting performed by area counts;
‡flea counting was performed by whole body counts for at least 10 minutes and personnel carrying out flea counts were blinded to treatment;
¶: cats were combed using modified whole-body comb counts, whereas in dogs fleas were counted using area counts. % efficacy after 1 month = (Day 0 geometric mean flea counts - Day 28 geometric mean flea counts) ÷ (Day 0 geometric mean flea Counts) × 100%
% flea free at end of the study = (number of flea free animals total number of animals in study) ÷ (total number of animals in the study) × 100%
For anti-flea products to be licensed, they must comply with regulations set out by the European Medicines Agency. The reported methodologies differ with regard to how flea counts were performed. Flea counts in two studies were performed by area counts, marked by a [†] in Table 1. In one study, efficacy was determined in cats using a modified whole-body comb count and using visual area counts in dogs (Dryden et al, 2018). Results from these studies are acceptable as the method of counting was consistent in the study and had been previously validated (Dryden et al, 1994), but whole body counts would have been preferable as area counts are less accurate and should only be used to initially recruit flea infested animals (Marchiondo et al, 2013).
All reviewed studies were pharmaceutical industry funded, but the potential for bias is reduced by the use of controls. Two studies used a negative control (Saridomichelakis et al, 2015; Otranto et al, 2017), with the remainder using positive controls. Although using an untreated group might have provided a better comparison, withholding treatment in cases of severe flea infestation raises ethical issues (Wolken et al, 2012). This was reflected in the Otranto et al (2017) study where 16 out of 100 cats in the negative control group presented with flea allergy dermatitis. To prioritise their welfare, flea treatment had to be administered but resulted in the exclusion of these cats. Therefore, the use of a positive control may have been more appropriate. Although controls were used, in six studies the personnel who conducted the flea counts were not blinded to treatment groups so there is a possibility that bias could have been introduced. Investigators may have also introduced bias by not being as meticulous when checking for signs of flea infestations or by combing animals more vigorously, resulting in more fleas being collected.
In field studies, because of the reinfestation pressure, it is normal for the efficacy of anti-flea products to be lower than the proposed 95% efficacy in controlled laboratory studies (European Medicines Agency, 2016). As a specific value has not been defined, for the purpose of this review, an arbitrary 10% reduction has been applied. Treatment with a mean efficacy ≥85% at 28 days after treatment was considered effective. The results from the above studies, except three cases of fipronil (S)-methoprene (FSM) and one case of selamectin, have exceeded this limit. However, the overall mean efficacy for selamectin was 86.75% but the mean % for FSM was 74.5% therefore discussion will mainly focus on FSM.
The percentage efficacy achieved 1-month post-application is notably lower for FSM, with three out of four studies achieving 81.2% efficacy or lower. One of these studies (Dryden et al, 2013a) was conducted in Tampa Bay, Florida and the other two were multi-centric studies each conducted across ten US states (Dryden et al, 2013b; Meadows et al, 2017). These three studies reported that FSM failed to achieve adequate flea control. All animals were randomly assigned to treatment groups, so the differences in efficacy between products were more likely caused by product performance than differences in home conditions (Dryden et al, 2013b).
In the study by Dryden et al (2013a), where 49.5% efficacy was reported after 1 month, the product was applied by trained investigators. This reduces the likelihood that compliance or incorrect administration of treatment could be the reason for lower performance. In the study by Meadows et al (2017), investigating efficacy of topical fluralaner and FSM, the topical application of fluralaner was demonstrated to be effective, suggesting that owners in the study understood how to administer topical products correctly and misapplication of FSM by owners was unlikely.
One possible reason for lower efficacy of FSM could be the impact of water. Water activities such as bathing and swimming were not restricted, except for the Meadows et al (2017) study where no water contact was allowed for 72 hours after application and Dryden et al (2013a), who restricted bathing to a maximum of twice a month. Apart from spinosad, the other treatments were all administered topically. Bathing dogs treated with indoxacarb twice monthly, or fluralaner 4 times within a 12-week period did not have an impact on efficacy (Armstrong et al, 2015; Taenzler et al, 2016). Despite manufacturers stating that FSM does not require avoidance of swimming or bathing, one study demonstrated that weekly bathing reduces the residual efficacy of FSM against fleas by about 2 weeks (Cruz et al, 2020). This could provide one reason as to why the reported efficacy of FSM was reduced in the included studies.
The apparent increase in flea counts recorded in the Dryden et al (2013a) study suggests that there is a greater flea burden in Tampa, which could provide one explanation for the lower efficacy of FSM observed. Rising flea challenges in Tampa are supported by the recent increase in initial geometric mean pet flea burdens. The initial geometric mean number of fleas in area-counts reported in a 1997 study for two treatment groups was 19.0 and 19.8 (Dryden et al, 2000). It is useful to note that the area count methodology used in these studies only accounts for approximately 23.5% of the total flea burden. Therefore, total flea burdens are four times larger. Similarly, in another Tampa-based study carried out in 2000, the geometric mean number of fleas in area-counts on day 0 in two groups was 15.8 and 19.2 (Dryden et al, 2001). Comparing these values with the geometric means of 28.6 in 2011 and 28.1 in 2013, it seems that the flea population was increasing in those two later years. However, despite those initial flea count differences, the 1-month post-treatment efficacy of 49.5% observed by Dryden et al (2013a) was dramatically reduced from the efficacy of 89.4% observed by Dryden et al (2000). Both studies were conducted in the same geographical location (west-central coastal Florida) using the same treatment and data collecting methodologies.
A study carried out in seven European countries demonstrated that 91.75% of dogs and 89.41% of cats became flea free after 3 months of treatment with FSM with no environmental control (Beugnet and Franc, 2010). The animals that remained infested were subject to high infestation pressures, including being in a multi-pet household and having regular outdoor activity, where other pets and wildlife may act as reservoirs for fleas. Therefore, treatment of all susceptible animals within the household and measures mitigating the risk of feral cats or wildlife entering gardens would be needed (Abdullah et al, 2019). In these cases of severe flea burdens, to achieve optimum control quickly and successfully, environmental treatment is also strongly advised (Dryden et al, 2000).
It has been reported that 2–4 months of regular monthly treatment is needed to remove fleas from the environment, or longer still if the pet is in a high-risk area (Jacobs et al, 2001; Chin et al, 2005; Dryden et al, 2011a). This relies on the time taken for the pupal reservoir to be depleted, as this stage is often unaffected by insecticides because of their location within the environment. (Elsheikha and Wright, 2014). The percentage of flea-free animals reported in the included studies documenting FSM efficacy, ranged from 15.6–55.56% after 2 or 3 months of treatment. Fleas on an infested pet are more likely to be from environmental reinfestation rather than survival of treatment, so it is possible that high reinfestation pressure and lack of appropriate environmental treatment are responsible for the reduced level of control achieved with FSM.
However, this does not explain why the other treatments spinosad, fluralaner and indoxacarb were significantly more effective than FSM with ≥95% efficacy, despite facing the same challenges. It is possible that the residual activity of FSM tapers off faster than with other treatments. As a result, closer to the end of the dosing period, the effectiveness of FSM falls to the extent that the fleas' reproductive cycle is no longer disrupted (Dryden et al, 2015). Resistance or the presence of flea strains in Tampa that are innately tolerant to FSM could be another explanation. It is interesting to note that in the Dryden et al (2000) study, efficacy was 96.7% by 2 months after the second application of fipronil, whereas in the Dryden et al (2013a) study efficacy was only 54.8% at 2 months. However, in the 2011 study (conducted in 2010), also carried out in the Tampa Bay region, FSM achieved an efficacy of 88.7% at day 28 (Dryden et al, 2011b). It is unknown why efficacy dropped so substantially within the 3-year time period between when these studies were conducted. The reduced performance of FSM was further exemplified by the lower percentage of flea-free animals in those studies (15.6–55.56%), compared with what was achieved by the comparative formulations. Flea-free rates were 77.1%, 93.3% and 94.8% for indoxacarb, fluralaner and spinosad, respectively (Dryden et al, 2013a, 2013b; Meadows et al, 2017). It was only the dinotefuran-permethrin-pyriproxyfen formulation in Dryden et al's (2011b) study that had a similar flea-free rate (60.0%) to FSM formulation in those studies.
The marked increase in the number of pets that still had fleas at the end of the FSM studies warrants further investigation. Whether this an indication of reduced speed of kill and continued flea reproduction in the households studied, ought to be considered. In the Dryden et al (2013a) study, when the 2 month flea-free rate of FSM was only 15.6%, flea emergence in the homes, based on previous flea trap counts, was reduced by 60.3% and 84.6% at 1 and 2 months, respectively. In the homes where pets were treated with indoxacarb, the percentage flea-free rate at the end of the study was 77.1% and flea emergence was reduced by 87.9% and 97.7% at 1 and 2 months respectively.
A similar issue could be raised with selamectin. In Dryden et al's (2018) study, monthly topical applications of selamectin reduced flea populations on cats by 77.8%, 91.0% and 91.3% at 1, 2 and 3 months respectively, whereas in the other treatment group, where cats were treated with topical fluralaner once on day 0, flea populations were reduced by 98.5%, 99.2% and 100% at the same monthly intervals. The percentage of selamectin treated cats, free of fleas at the end of that 3 month study, was only 38.5%. It is interesting to note that a few years later, when a similar study was conducted in the same geographical region and cats were treated with 3-monthly doses of a topical selamectin-sarolaner combination, 100% of cats were flea-free at the end of the 12-week study period (Dryden et al, 2020).
The aforementioned reasons for these reductions in efficacy and percentage of flea-free rates are likely multifactorial and may include severe re-infestation pressure, reduction in the residual speed of flea kill and variability in the susceptibility of C. felis flea strains encountered in different regions and different study years.
Factors affecting pet owners' adherence
We also evaluated the impacts of owners' adherence on treatment success. Of the seven papers included on adherence (Figure 1), all explored potential factors impacting owners' compliance, summarised in Table 2. Five studies were survey-based and two studies involved the analysis of purchase records as an indicator of owners' adherence. The study could not identify any papers that evaluated the direct impact of the owner's adherence on the success of anti-flea treatments. Two studies analysed anti-flea purchases from veterinary practices as an indirect measure of adherence (Gates and Nolan, 2010; Lavan et al, 2018). Both of these studies reported low levels of owner compliance, with the vast majority only obtaining one or two doses of a treatment per year. However, if treatment was purchased before the study period but used within it or if owners purchased treatment from other sources, this could have resulted in an underestimation of adherence. In contrast, if owners did not administer the purchased flea treatment correctly, or at all, this would lead to an overestimation. However, analysing purchase records is more objective than the use of self-reporting methods such as interviews and surveys, which were employed in the remaining studies and carry the limitation of owner recall and bias. As an example, owners may overestimate the frequency of anti-flea treatment given to avoid being seen as a bad pet owner (Lavan et al, 2020).
Table 2. Summary of factors that affect owners' adherence based on surveys and purchase records of anti-flea products
| Veterinary team | Client | Product |
|---|---|---|
|
|
|
Three studies concluded that reduced dosing frequency of longer acting anti-flea treatments leads to better adherence (Lavan et al, 2017, 2018, 2020). A reported 67% of dog owners believed that the extended dosing interval of fluralaner would make them less likely to forget to administer treatment, compared to a monthly regimen (Lavan et al, 2020). However, these studies were all funded by the manufacturer of the product, which is the only systemic anti-flea treatment that offers up to 12 weeks of protection. All owners that completed the survey had to be currently using fluralaner, resulting in a biased recruitment process as it is possible that owners had a pre-disposed preference for fluralaner over other anti-flea products. Previous studies in both human and veterinary medicine have also demonstrated that reduced dosing frequency improves adherence, which was used to support the conclusion (Claxton et al, 2001; Adams et al, 2005). However, the cited studies compared once or twice daily dosing to three times daily dosing and it is unclear whether these same results would translate to extended periods of up to 12 weeks.
All studies involved pet owners who had recently visited their veterinary practice. Reported factors affecting adherence may not be representative of the overall population of pet owners. For instance, those who do not visit the clinic regularly may not be able to afford regular treatment or might obtain treatment over the counter. They may have been more likely to administer treatment incorrectly in the absence of veterinary advice (Cooper et al, 2020). It was reported that insufficient advice also presents an issue for adherence, even for owners who visited the clinic. It is important that advice is communicated effectively and that common misconceptions are addressed, including the belief that flea treatment is only necessary seasonally or sporadically (Matos et al, 2015), that side effects can be minimised by reducing dose frequency, that treatment inefficacy is the problem or that fleas are not a risk to humans (Belshaw et al, 2018a). Owners with a better understanding of the importance of anti-flea treatments are more likely to agree and follow recommendations (Lavan et al, 2017).
With the wide variety of available products, it is important for veterinarians to engage with clients in the decision-making process and tailor the treatment plan to individual needs. There is a concern among veterinarians that the promotion of preventative medicine is perceived by owners as solely a financial opportunity for vets (Belshaw et al, 2018a). However, when surveyed, only 10% of pet owners believed that recommendations were driven by profit making (American Animal Hospital Assocation, 2003). Therefore, veterinarians should be confident that this issue can be overcome, provided that different treatment options are discussed and rationale is given so that owners can make informed choices. Owing to time constraints, this responsibility usually falls to veterinary nurses and, increasingly, reception staff who advise on choices of ectoparasiticides as part of pet health care plans. Although receptionists do not require formal training, it is important that adequate training is provided so that accurate advice is given (Belshaw et al, 2018a). Protocols should also be standardised to ensure consistent advice is given by all staff members, with an emphasis on the importance of managing client expectations (Richmond and Wright, 2018). Flea eradication can take up to 8 weeks or more and if owners are not notified they can quickly become disillusioned (Halos et al, 2014). One of the authors (Dryden MWD), frequently councils veterinarians and veterinary students to never let pet owners set treatment expectations, because you will likely not be able to satisfy those expectations. Veterinary professionals must set the proper expectations on treatment duration and outcomes.
Limitations
Only prescription-only veterinary medicine products were included in the present study, so findings cannot be applied to over the counter products. The studies found were focused more heavily on dogs and it is possible other factors that are specific to cats have not been investigated. It was not possible to cover environmental factors that could affect treatment failure, so any conclusions drawn should consider the importance of environmental treatment in flea eradication. The direct effects of owners' adherence on the success of anti-flea treatments appears to be underreported, so factors affecting adherence were found but not tested. Therefore, only claims of a strong causal relationship between poor compliance and treatment failure can be made.
Conclusions
With the exception of fipronil S-methoprene, and possibly selamectin, common anti-flea products are highly effective. Further research into the residual activity of fipronil S-methoprene would be beneficial. This would ascertain whether its residual effects are potent enough to prevent flea reproduction, in line with the manufacturer's guidance.
Cooperation between all veterinary staff is needed to ensure consistent advice is given and misconceptions associated with perceived product inefficacy are clarified. Issues arising from lack of compliance, such as persistence of flea burdens in homes and exposure of flea-borne disease to both animals and owners, should be emphasised so that pet owners can appreciate the importance of flea treatment.
Overall, the current evidence indicates that the failure to reach adequate flea infestation control is more likely a result of poor owner compliance, rather than a lack of drug efficacy. This article provides strong evidence for inferential support of the proposed hypothesis, although it is not a confirmation since the link between treatment failure and poor compliance is a correlation only. However, the included studies have allowed identification of the factors affecting adherence and further research testing these proposed factors in randomised controlled trials, specific to flea control, would be beneficial. There is a need to gain a better understanding of how owner compliance might be optimized, as part of a successful strategy to improve flea infestation control in dogs and cats.
KEY POINTS
- Fleas are considered the most prevalent ectoparasite encountered on dogs and cats.
- Successful flea control relies mainly on the use of effective anti-flea products and pet owners' compliance with treatment recommendations.
- Numerous antiparasitic drugs targeting fleas, known as pulicides or insecticides, are available on the market for use in companion animals.
- With the exception of fipronil S-methoprene and possibly selamectin, common anti-flea products are highly effective.
- Lack of or insufficient guidance given to pet owners can result in poor understanding of the importance of flea treatment.


