Systemic hypertension, a persistent increase in the systemic blood pressure above 160 mmHg systolic, is now commonly recognised in feline practice. There are several reasons for this, including an increased awareness of hypertension as a feline problem, increased access to diagnostic facilities and potentially, an increased prevalence of this condition related to the increasing age of the cat population – with current estimates of its prevalence at approximately 20% of cats aged 9 years and over (Conroy et al, 2018).
An age-related increase in systolic blood pressure has been reported (Bijsmans et al, 2015), meaning that older cats are at an increased risk of developing systemic hypertension. Its onset is also often associated with other conditions, many of which increase in prevalence with age, further increasing the risk to older cats. As an example, one study of 58 cats with systemic hypertension reported their mean age to be 13 years (Chetboul et al, 2003). The most commonly associated illnesses are chronic kidney disease and hyperthyroidism. Prevalence rates reported have been highly variable, for example, 20–65% of cats with chronic kidney disease are diagnosed with concurrent systemic hypertension, compared to 9–23% of newly diagnosed hyperthyroid cats (Kobayashi et al, 1990; Littman, 1994; Stiles et al, 1994; Syme et al, 2002; Syme and Elliott, 2003; Morrow et al, 2009; Williams et al, 2010). Other diseases that have been associated with hypertension in cats include primary hyperaldosteronism (Conn's syndrome), phaeochromocytoma, therapy with erythrocyte stimulating agents and occasionally, hyperadrenocorticism (Patnaik et al, 1990; Henry et al, 1993; Chun et al, 1997; Cowgill et al, 1998; Ash et al, 2005; Javadi et al, 2005; Calsyn et al, 2010; Wimpole et al, 2010; Brown et al, 2012; Chalhoub et al, 2012).
Idiopathic hypertension (also referred to as primary or essential hypertension) accounts for less than 20% of cases (Maggio et al, 2000; Elliott et al, 2001; Jepson et al, 2007).
Why should we assess blood pressure in cats?
Systemic hypertension is a potentially life-threatening condition and four body systems are especially vulnerable to the damaging impact of high systemic blood pressure. These so-called target organs are:
- The eyes
- The brain and spinal cord
- The heart and blood vessels
- The kidneys.
Patients with systemic hypertension may present with clinical signs related to target organ damage (Table 1) or may present with clinical signs associated with underlying systemic disease since, especially since it is estimated that systemic hypertension is associated with another illness in 80% (or more) of affected cats. As an example, a cat with systemic hypertension caused by chronic kidney disease may present with weight loss, increased thirst and variable or poor appetite.
Table 1. Potential target organ damage associated with systemic hypertension
| Organ affected | Pathology | Clinical findings | Reported approximate prevalence |
|---|---|---|---|
| Brain | Hyperplastic arteriosclerosis of cerebral vessels, oedema of the white matter and microhaemorrhage development, resulting in hypertensive encephalopathy and/or stroke | Many changes possible, including behavioural changes (such as night-time vocalisation, signs of confusion or dementia), altered mentation, ataxia, seizures, focal neurological deficits including central blindness, headaches and coma | 15% (Caney, 2020) |
| Heart | Left ventricular hypertrophy and thickening of the interventricular septum | New murmur, arrhythmia, and/or gallop rhythm. | 50–80% (Caney, 2020) |
| Kidneys | Glomerular hypertrophy and sclerosis, nephrosclerosis, tubular atrophy and interstitial nephritis resulting in progression of chronic kidney disease | Reduced urine specific gravity, proteinuria, increasing creatinine and IDEXX symmetric dimethylarginine levels, decreasing glomerular filtration rate | |
| Eyes | Hypertensive retinopathy or choroidopathy resulting in many changes, including intra-ocular haemorrhage, retinal oedema, retinal detachment, arterial tortuosity, variable diameter of retinal arterioles, papilloedema and glaucoma. Foci of retinal degeneration (hyper-reflectivity) may develop where damage has previously occurred | Visual deficits, blindness, hyphaemia, mydriasis | 60–80% (Caney, 2020) |
Unfortunately, in many patients with systemic hypertension, there are no obvious clinical signs and the disease may be a ‘silent killer’. However, systemic hypertension is generally very straightforward to treat, and the prognosis is best if it is identified and addressed at the earliest opportunity. Additional benefits in terms of quality and length of life may be possible with management of any underlying conditions, such as chronic kidney disease.
When is measuring blood pressure justified?
Blood pressure should be assessed as a priority in any cats presenting with clinical signs that are consistent with hypertensive target organ damage (Table 1). This includes:
- Ocular clinical signs such as visual deficits and blindness, as well as retinal oedema, detachment, or haemorrhage
- Signs consistent with hypertensive damage to the brain and/or spinal cord, such as behavioural changes (increased vocalisation, altered mentation) or neurological signs (especially in older cats)
- Auscultable cardiac abnormalities consistent with systemic hypertension (murmur, gallop), or left ventricular hypertrophy evident on echocardiography
- Possible renal hypertensive damage, such as unexplained proteinuria or worsened renal status
In addition, screening for systemic hypertension is recommended in the following situations:
- In cats with any disease reported to have an association with systemic hypertension – particularly chronic kidney disease and hyperthyroidism (3–6 monthly blood pressure assessment is recommended to detect an increase in blood pressure before development of target organ damage). Hypertension has been reported to affect around 20% of previously normotensive cats following stabilisation of their hyperthyroidism (Morrow et al 2009).
- In older cats, routine screening for systemic hypertension is recommended as a component of ‘well cat’ clinics, particularly in cats aged >7 years. The charity International Cat Care recommends annual blood pressure screening in cats aged 7–10 years, with 6-monthly screenings in cats aged 11 years and over.
- In older cats (>7 years) undergoing elective surgical procedures, such as elective dental surgery, blood pressure screening tests are also justified as a component of pre-anaesthetic checks. Depending on the clinic, the cat and the procedures planned, it may be less stressful to perform blood pressure and other pre-anaesthetic assessments for elective procedures on a separate day to the procedure itself.
Preparing for blood pressure assessment
Stress-associated transient increases in systolic blood pressure, referred to as ‘situational hypertension’ or ‘the white coat effect’, are common and can make reliable diagnosis of systemic hypertension challenging (Box 1). Clinic protocols need to be designed with the aim of minimising stress in cats and their caregivers as much as possible. Blood pressure measurements should be collected first, before any other procedures, so that the cat is as calm and relaxed as possible. The author generally favours measuring blood pressure as an ‘outpatient’ procedure with the owner present, where permitted, to reassure the cat. On average, the ‘white coat’ effect increases systolic blood pressure by 15–20 mmHg. However, the effect is highly variable between cats and can be as much as 75 mmHg (Belew et al, 1999).
Box 1.Important definitionsSituational hypertension: a transient increase in systolic blood pressure associated with stress, excitement or anxiety and activation of the autonomic nervous system. Situational hypertension is varies highly between cats and may differ considerably with different visits to the vet clinic. A typical magnitude of blood pressure increase is considered to be up to 30 mmHg, although one study reported an increase of 75 mmHg in one cat (Belew et al, 1999). Allowing a period of ‘acclimatisation’ before collecting blood pressure measurements is usually successful in reducing the magnitude of situational hypertension.Masked hypertension: in some cats blood pressure decreases with stress or anxiety, which can result in ‘masked hypertension’ (where a diagnosis of genuine systemic hypertension is missed because of the individual's stress response).Idiopathic hypertension: a persistent, pathological increase in systolic blood pressure, where the cause of this increase is unknown. Other terms used in the past for this scenario included ‘primary’ and ‘essential’ hypertensionSecondary hypertension: a persistent, pathological increase in systolic blood pressure concurrent with a medication, disease or condition known or thought to cause systemic hypertension, the most notable of which would be concurrent chronic kidney disease.
Cats always like to feel in control of their environment, so a visit to a veterinary clinic is highly stressful for several reasons:
- The cat is removed from their normal environment and then suffers a series of unfamiliar events incorporating strange noises, smells and sights
- The cat carrier used for vet visits is typically unfamiliar and may contain smells or other reminders of previous stressful experiences
- The cat loses their sense of control over their environment when placed into the carrier
- A car journey (or perhaps bus or train) is often involved in taking the cat to the clinic and the cat may experience some motion sickness in addition to the stress
- On arrival at the clinic, the cat typically has a wait in the clinic waiting area before being seen and thus may be exposed to other cats, dogs and owners
Where possible, carers should be advised on how they can choose an appropriate carrier for their cat. Often this is not possible before the first clinic visit, but if the cat is presented in an ‘unsuitable’ cat carrier then advice should be given to reduce stress for future visits (Table 2).
Table 2. Characteristics of good cat carriers and factors to consider when choosing a cat carrier
| Good cat carriers | Factors to consider |
|---|---|
| Should be made of robust material that can be cleaned and disinfected, such as plastic, metal or mesh | Carriers that are made of cardboard soften and disintegrate when wet, can be scratched open by a determined cat and are not possible to clean. Carriers made of different materials that are difficult to clean and disinfect should also be avoided. Line the carrier with something absorbent, such as a towel on top of newspaper or incontinence padding, in case of any urination on the journey. Always clean the carrier thoroughly if the cat urinates, vomits or defecates |
| Should not be possible for the cat to escape from | Home-made carriers and those made from cardboard are less secure. Note that plastic doors can be broken so may present a trauma or escape hazard, but a steel mesh door is durable and hard to break |
| Should have a sturdy frame (soft carriers incorporating a supportive frame can be acceptable for cats) | Soft-sided carriers with no support can be uncomfortable for the cat, can be difficult to get the cat into without it escaping and are vulnerable to being torn by the cat's claws. Zips on soft carriers can become faulty over time and can be difficult to do up quickly (for example, when the cat is trying to escape the carrier). Make sure that the carrier is strong enough if the cat is especially heavy or large |
| The carrier should be large enough for the cat. Generally, the length of the carrier should be 1.5 times the length of that cat from nose to base of tail | The cat should be able to stand up, move around and lie down. If they can't do this, then the carrier is too small |
| The carrier should have a large top opening or be easy to dismantle | If the carrier cannot be dismantled and only has a front opening, it can be very difficult to get a reluctant or injured cat out of the carrier. It is an advantage to have openings on both the front and the top to give flexibility on ways of removing the cat and placing it into the carrier. Openings should be large so that it is easy to do this without causing trauma. It is an advantage for the front door of the carrier to be detachable allowing the cat to choose whether it wants to exit the carrier voluntarily |
| It should be possible to secure the carrier while travelling | Some carriers have holders for passing through car seat belts, which increases the security of the cat when travelling by car |
| The carrier should have plenty of ventilation holes | Choose a carrier that has ventilation holes on at least three sides, as cats can overheat in small spaces, especially if ventilation is inadequate |
Caregivers should be encouraged to familiarise and acclimatise their cat to the carrier before it is used to transport the cat. The carrier should be placed into a room which the cat uses and left open (remove the top if it is a dismantlable carrier), with familiar bedding, toys and treats placed inside to encourage the cat to explore the carrier. If possible, the carrier should permanently stay in this location and, hopefully, will become viewed as a positive rest location for the cat. If it is not possible to always leave the carrier out, then it should be introduced a few days in advance of the appointment (if possible) to familiarise the cat with it. A once daily spray of the synthetic feline facial pheromone (Feliway, Ceva Animal Health) also helps to transmit a sense of reassurance to the cat. On the day of the visit, the carrier should be sprayed 20–30 minutes before placing the cat inside. One spray into each corner of the carrier should be enough. It may also help to cover the carrier with a familiar blanket or towel, as this helps the cat to feel more secure. The blanket can also be used as a surface to examine the cat on when in the clinic consulting room.
Caregivers bringing more than one cat to the clinic should be advised to use one carrier per cat, even if the cats get on well at home, as the stress of the clinic visit and close confinement can lead to tensions, even between cats that are friends. Other tips for caregivers can be found in Table 2.
In an ideal world, to minimise stress associated with a clinic visit, the clinic would be quiet and free of other animals for the duration of the visit, and the vet would be running on time to minimise waiting times. However, this is most often not possible, so other measures can be followed to help reduce stress levels.
- Ideally, cats should not be able to see, hear or smell other patients during their visit. A separate waiting room, entrance and exit points for cats (compared to dogs) are ideal where possible. If not, try and create a cat waiting area which is ‘screened off’ from other animals. An empty cat consulting room can also be helpful as an occasional cat waiting room (preferably for one cat at a time rather than more).
- Cats feel safer at a height rather than being at floor level, so consider having shelves to place cat carriers on, or allowing carers to place cat carriers on to chairs in the waiting room
- Covering the carrier with a towel or blanket can increase the feeling of security, so consider offering clinic towels, pre-sprayed with Feliway, in the waiting room for this purpose
- Make sure that you have a Feliway diffuser in the waiting area. The synthetic feline facial pheromone transmits a sense of calm and reassurance to the cats
- If possible, allow for occasional spare appointments so that if the veterinarian is running late, the waiting room is not filling up with animals.
In waiting areas that must be shared with dogs or other animals:
- Encourage clients to be as calm and quiet as possible
- Advise owners of dogs to try and sit as far away from the cats as possible and not allow their dogs to sniff or approach the cat carriers
- In addition to the Feliway diffuser, install a DAP diffuser (Adaptil, Ceva Animal Health) as the canine appeasement pheromone will help the dogs to feel calmer and hence create a more restful environment for the cats
- Consider offering clients the option of placing the cat in its carrier in a different, quiet and calm location (such as on a raised surface behind the reception desk)
- Consider asking the client to wait in their car with their cat until the clinician is ready to see them
- Consider having ‘cat only’ appointment times to minimise cat exposure to dogs and other species.
For cats that remain very stressed by blood pressure assessment, pre-visit administration of gabapentin can be helpful in providing some sedation, without impacting blood pressure results (van Haaften et al, 2017). A suggested dose of 20 mg/kg can be given in a treat or small amount of food 2 hours before the cat is due to be put in their carrier. Cats with chronic kidney disease metabolise gabapentin more slowly, so may need a downward dose adjustment.
Blood pressure measurement
Blood pressure measurement and eye examination are both important when evaluating a patient for possible systemic hypertension, although many patients will not have any clinical signs associated with their high blood pressure.
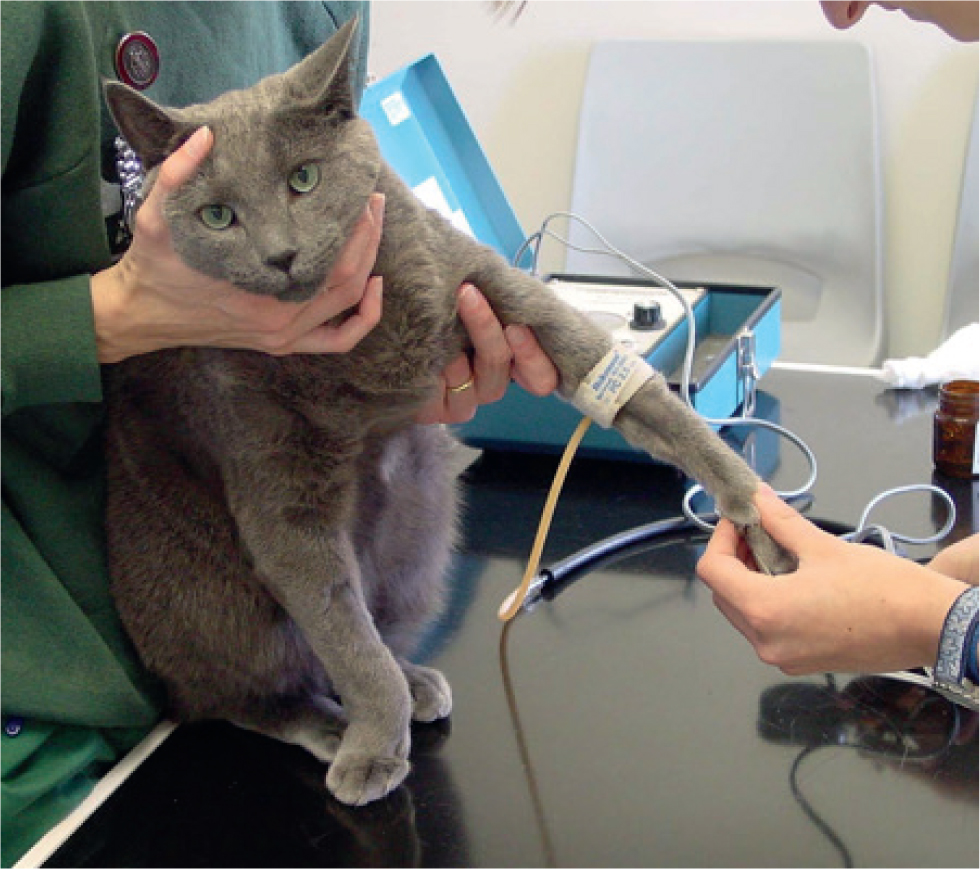
The author favours the Doppler technique for measurement of blood pressure in conscious cats (Figure 1). Techniques for blood pressure measurement are reviewed elsewhere (Taylor et al, 2017; Acierno et al, 2018).
Regardless of methodology, the most reliable blood pressure readings will be obtained by allowing the cat a period of acclimatisation to their surroundings before taking measurements and by performing this procedure in a calm and quiet location. Tips for reducing the ‘white coat effect’ are shown in Box 2.
Box 2.The author's tips for reducing ‘white coat’ hypertension and obtaining reliable blood pressure readings
- Use a quiet room for blood pressure measurement, away from barking dogs, telephones and human traffic
- Allow the cat 5–10 minutes to acclimatise to you and the surroundings before starting the procedure
- Always measure blood pressure before performing any other assessments in the cat. Otherwise, add a 30-minute rest period after procedures before collecting blood pressure readings
- It can be helpful having the owner present to gently restrain their cat
- Use minimal restraint
- Do not rush!
For Doppler blood pressure measurements:
- Wear headphones so that the cat is not aware of any noise associated with the procedure.
- There is no need to clip the fur, even in long-haired cats, as this may be stressful to the cat. Instead, prepare the area by wiping with water or surgical alcohol and then applying plenty of ultrasound gel.
- Slowly inflate the cuff in a series of gentle puffs, as sharp inflations can surprise or stress the cat. Sometimes doing a series of ‘practice’ cuff inflations and deflations can be helpful in acclimatising your patient to the procedure.
- Completely deflate the cuff between readings, otherwise the procedure may start to become uncomfortable and therefore stressful to the cat.
- Use a sphygmomanometer that allows slow and gradual cuff deflation.
- Collect at least five readings: discard the first reading if very different to the others and average the remainder. If the readings are very variable, continue to collect readings until they ‘plateau,’ averaging the ‘plateau’ readings. If no plateau is reached, the lowest reading is likely to be most representative of the cat's true systolic blood pressure.
- Always record the cuff used and site of blood pressure measurement, as the size and location of the cuff affects the readings obtained. The cuff should be at the level of the right atrium. The ideal cuff width is 30–40% of the limb circumference: if wider than this the readings obtained will be lower than the ‘true’ blood pressure.
The International Renal Interest Society (IRIS) and American College of Veterinary Internal Medicine (ACVIM) recommend a reference range of 120–149 mmHg for systolic blood pressure readings in cats. Treatment for systemic hypertension is recommended if systolic blood pressure readings are above 160 mmHg, with the following guidance:
- Systolic blood pressure >160 mmHg, with evidence of target organ damage (Table 1): Systemic hypertension is diagnosed and treatment should be started
- Systolic blood pressure readings of 160–180 mmHg, but no target organ damage: repeat measurements should be collected within 1–2 months and if found to be persistently in this region (or higher), systemic hypertension is likely and treatment should be considered. Where possible, consider investigations for conditions commonly associated with systemic hypertension.
- Systolic blood pressure readings >180 mmHg but no target organ damage: repeat measurements should be collected within 1–2 weeks and if found to be persistently in this region, systemic hypertension is likely and treatment should be considered. Where possible, consider investigations for conditions commonly associated with systemic hypertension.
A detailed ophthalmic examination is essential both in the diagnosis and assessment of the patient. A thorough ocular examination is most easily done by using distant indirect ophthalmoscopy in a dark room (Figure 2). This is an ideal way to visualise large portions of the retina very quickly. Gross abnormalities including retinal oedema and detachment, intraocular haemorrhage and vessel changes can be seen (Figure 3) (Caney, 2019). Direct ophthalmoscopy can be used to have a closer look at any lesions identified.


Conclusions
Systemic hypertension is defined as a persistent, pathological increase in systolic blood pressure (160 mmHg or higher). Several (preferably a minimum of five) systolic blood pressure readings should be collected and an average calculated. Since situational hypertension can result in readings transiently 160 mmHg or higher, systemic hypertension is only confirmed in cats with an average systolic blood pressure of 160 mmHg or higher if:
- There is concurrent evidence of target organ damage (Table 1)
- Or, the systolic blood pressure readings are 160 mmHg or higher on several occasions.
Since the risk of target organ damage is proportional to the magnitude of systolic blood pressure elevation it is recommended that:
- For cats with systolic blood pressure readings of 160–179 mmHg but no evidence of target organ damage, reassess blood pressure on 2–3 occasions over a 2-month period. If systolic blood pressure results are persistently 160–179 mmHg (or greater), then treatment is justified
- For cats with systolic blood pressure of 180 mmHg and higher but no evidence of target organ damage, reassess blood pressure on 2–3 occasions over a 2-week period. If systolic blood pressure results are persistently 180 mmHg or greater, then treatment is justified
Where diagnosed, systemic hypertension is typically very straightforward to manage with anti-hypertensive therapies such as amlodipine and/or telmisartan. Once the hypertension has been stabilised, investigations (blood and urinalysis) are recommended to look for an underlying cause of the hypertension. Venepuncture of a severely hypertensive cat carries a risk of potentially fatal hypertension-induced haemorrhage associated with the stress of the procedure. Therefore, investigations should be delayed until the cat has been successfully stabilised with anti-hypertensive therapy. Further information on management of systemic hypertension is reviewed extensively elsewhere (Taylor et al, 2017; Acierno et al, 2018).
KEY POINTS
- Systemic hypertension is a common disorder, primarily affecting older cats.
- Systemic hypertension is usually secondary to another illness; primary hypertension is uncommon in cats.
- The most common condition associated with systemic hypertension in cats is chronic kidney disease.
- Measurement of blood pressure is indicated in all situations where patients present with clinical signs compatible with target organ damage.
- Screening for systemic hypertension is recommended in older cats and those with underlying health problems associated with hypertension.
- Accurate diagnosis of systemic hypertension requires measurement of blood pressure and is strengthened by ocular examination.


