Ocular and orbital foreign bodies require immediate treatment and urgent referral to a specialist, particularly in cases of full-thickness penetrating and perforating wounds (Maggs, 2016; Whitley and Hamor, 2021). Ocular injuries caused by accidental contact with plant material are most common in small animals (Jones, 2012; Pont et al, 2016; Wait et al, 2018). The different management options for ocular foreign bodies in small animals reflect their variable clinical presentations and range from medical management to a surgical approach (Maggs, 2016; Pont et al, 2016; Braus et al, 2017).
Epidemiology
Ocular injuries are observed more frequently in young dogs of less than 5 years of age, as well as in hunting and working breeds such as English Springer Spaniels and Labrador Retrievers. Injuries from thorns are commonly seen in the winter months, linked to the working season for hunting dogs, but foreign bodies such as grass seeds are more common in the summer owing to the associated harvesting and holiday period (Jones, 2012; Pont et al, 2016).
Pathogenesis
Ocular damage caused by foreign bodies is usually a result of penetrating or perforating injury, but can also occur from the presence of the foreign body itself causing infectious or inflammatory reactions (Maggs, 2016; Whitley and Hamor, 2021). Foreign body material may reach the globe directly, such as in wooden stake injuries, or following migration from other sites (Gould, 2016). Foreign bodies can easily become lodged in the conjunctival sac or behind the third eyelid. This foreign material may erode the intact conjunctiva, can migrate into the retrobulbar tissues or even penetrate the globe (Peruccio, 2016).
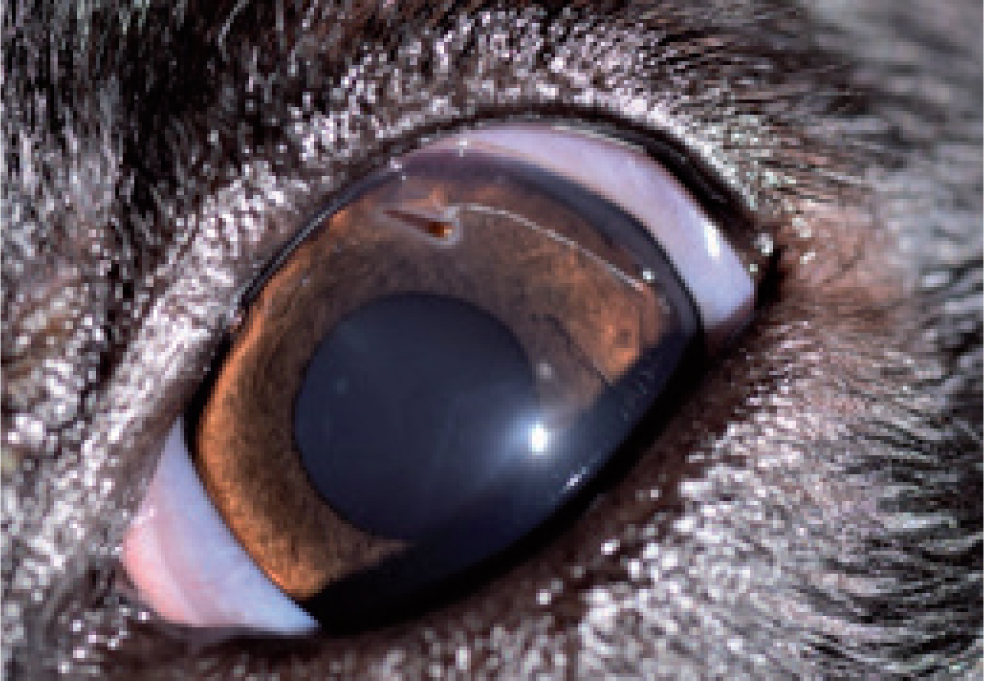
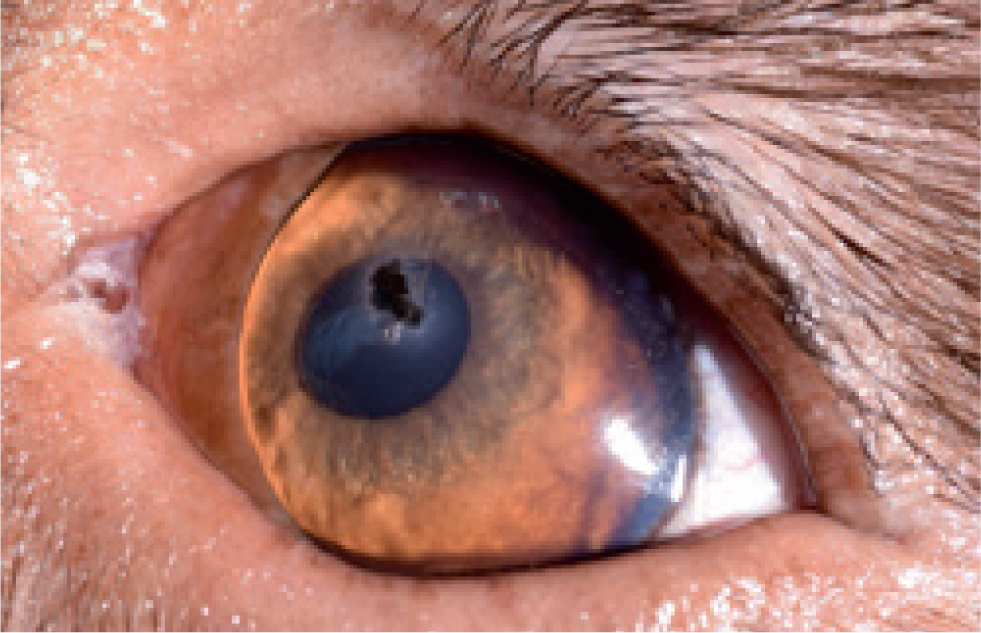
Occasionally, a foreign body can become trapped within the lacrimal sac or may be retained at the entrance of the nasolacrimal bony canal, where the lacrimal duct is at its narrowest (Leiva and Giménez, 2016). Intracorneal foreign bodies can be divided into those embedded in the stroma (penetrating) and those partially in the cornea protruding into the anterior chamber (perforating) (Gelatt and Brooks, 2011; Salmon, 2019). Perforating corneal foreign bodies may become encapsulated by fibrin in the anterior chamber, making their detection more difficult. In rare cases, a foreign body will enter the iridocorneal drainage angle, remain hidden from sight and cause severe anterior uveitis (Whitley and Hamor, 2021).
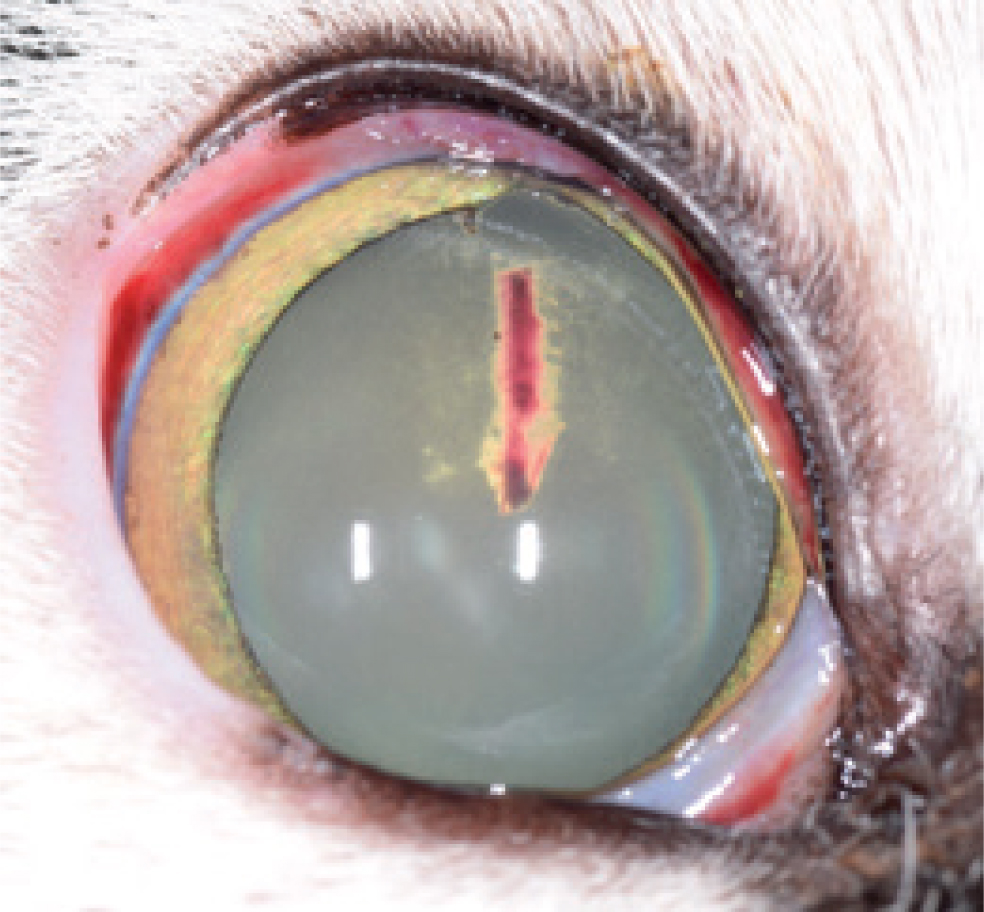
Corneal perforations may occur with or without iris prolapse or associated lens trauma (Gelatt and Brooks, 2011). Corneal foreign bodies tend to be the most common in dogs, while retained anterior chamber foreign bodies are less common (Hendrix, 2021). Ocular perforation can also be associated with injuries caused by oral foreign bodies that penetrate the orbit and perforate the globe (Gould, 2016). The most common intravitreal foreign bodies in dogs and cats are airgun pellets and lead shots, which are generally associated with severe ocular trauma (Heinrich, 2014).
Possible complications of full-thickness corneal foreign bodies include keratomalacia at the site of perforation, iridal abscess formation, and septic endophthalmitis with secondary glaucoma or retinal detachment. Minor lens involvement can result in an incipient cataract (Hendrix, 2021).
Orbital foreign bodies are sometimes encountered in small animals (Stades et al, 2003; Lybaert et al, 2009) and may enter the orbit through the oral cavity, percutaneously or via the conjunctival sac. Dogs presenting with non-neoplastic orbital diseases are significantly younger than dogs presenting with neoplasia. Foreign material in the orbit may lead to orbital abscesses or cellulitis (Pot et al, 2021) and animals presenting with chronic purulent ocular discharge should be checked for the presence of a conjunctival fistulous tract (Stades et al, 2003).
Types of foreign bodies
Small pieces of wood, sticks and thorns, grass awns and glass are the most common foreign bodies (Figures 1–3).

They can become embedded in the conjunctiva or third eyelid, cornea or sclera (Jones, 2012). Gunshot injuries are also common in small animals and are usually intentional in cats and accidental in gun dogs (Sansom and Labruyère, 2012). One case report discusses a retrobulbar lymphoma that was associated with a ballistic foreign body in a cat (Robat et al, 2016).
Generally, foreign bodies consist of organic materials such as plants or vegetables and are not well tolerated, causing endophthalmitis or cellulitis. By contrast, inorganic material is relatively inert (Hendrix, 2021). Inorganic foreign bodies such as glass, plastic, and lead are non-reactive, while iron and copper foreign bodies are reactive and more likely to cause direct toxicity to intraocular structures (Lit and Young, 2002). In addition, the mechanism of entry and size of the object also determine the extent of injury. Metallic foreign bodies that have made their way into the eye at high speed will generate enough heat to become sterile so endophthalmitis will be less likely to develop (Hendrix, 2021).
Diagnostic approach
History and clinical signs
Most patients with ocular foreign bodies will exhibit signs of acute discomfort such as blepharospasm, enophthalmos, third eyelid protrusion, chemosis, conjunctival hyperaemia and lacrimation followed by a mucopurulent discharge (Maggs, 2016). The presence of significant ocular pathology and pain often precludes detailed observation, which means topical anaesthesia is usually essential (Maggs, 2016). Some dogs may have been running through the park and the bushes, and returned with one eye closed, attempting to rub the affected eye. Usually, only one eye is affected and in most cases no previous ocular abnormalities are reported (Whitley and Hamor, 2021). Once the foreign body embeds in the cornea, it is common for the eye to be pain free (Jones, 2012), as corneal pain fibres are relatively superficial (Jones, 2012; Maggs, 2016; Whitley and Hamor, 2021).
Examination
Foreign body detection is often difficult when examining with the naked eye alone. Using adequate magnification, the location, type, size, depth and angle of penetration of the foreign body should be determined. Taking all these factors into account will help the clinician decide whether removal will be relatively straightforward or complex (Jones, 2012; Pont et al, 2016; Hendrix, 2021).
Oblique foreign body tracts will be less likely to leak when the foreign body has been removed compared to perpendicular tracts, although the latter will result in the least scar formation (Gelatt and Wilkie, 2011).
Initially, the menace response and dazzle reflex should be evaluated, as well as the direct pupillary light reflex if possible. If the pupil in the affected eye cannot be visualised as a result of opacification of the anterior segment, or is fixed because of synechiae, the consensual pupillary light reflex from the affected to the unaffected eye is an essential prognostic indicator (Maggs, 2016). A thorough ophthalmic examination should then be conducted in a dark room (Giuliano, 2005), assessing the conjunctival fornices, both sides of the nictitating membrane, cornea, anterior chamber, pupil, iris and lens in particular. The palpebral surface of the third eyelid can easily be exposed for examination by digital retropulsion of the globe through the upper lid. The bulbar surface is examined after applying topical anaesthesia, and forceps or mosquito haemostats are used to grasp the leading edge while avoiding the cartilage (Peruccio, 2016).
The slit-lamp biomicroscope is the most versatile diagnostic tool for the veterinary ophthalmologist. It permits a magnified, three-dimensional examination of the adnexa, cornea, anterior chamber, lens and vitreous. On a slit setting with high levels of illumination, the slit-lamp functions to section the transparent tissues of the anterior segment, allowing for accurate localisation of a foreign body (Featherstone and Heinrich, 2021). A thorn foreign body may appear more distinct when using the technique of retro-illumination through distant direct ophthalmoscopy (Jones, 2012).
Following pupil dilation, the patient's fundic reflex is picked up at arm's length using a bright light source, such as a direct ophthalmoscope or slit-lamp, and any opacities in the clear ocular media will stand out dark against the bright background (Featherstone and Heinrich, 2021). Using this method, a thorn may be easily seen even in areas of oedema, since its distinct shape may be more obvious. The absence of a foreign body outline provides reassurance that there is no thorn present. It can be difficult to distinguish corneal foreign bodies that remain within the cornea from foreign body tracts, because blood or debris within the tract can mimic the presence of a foreign body (Figure 4). These cases would also benefit from retro-illumination (Jones, 2012).
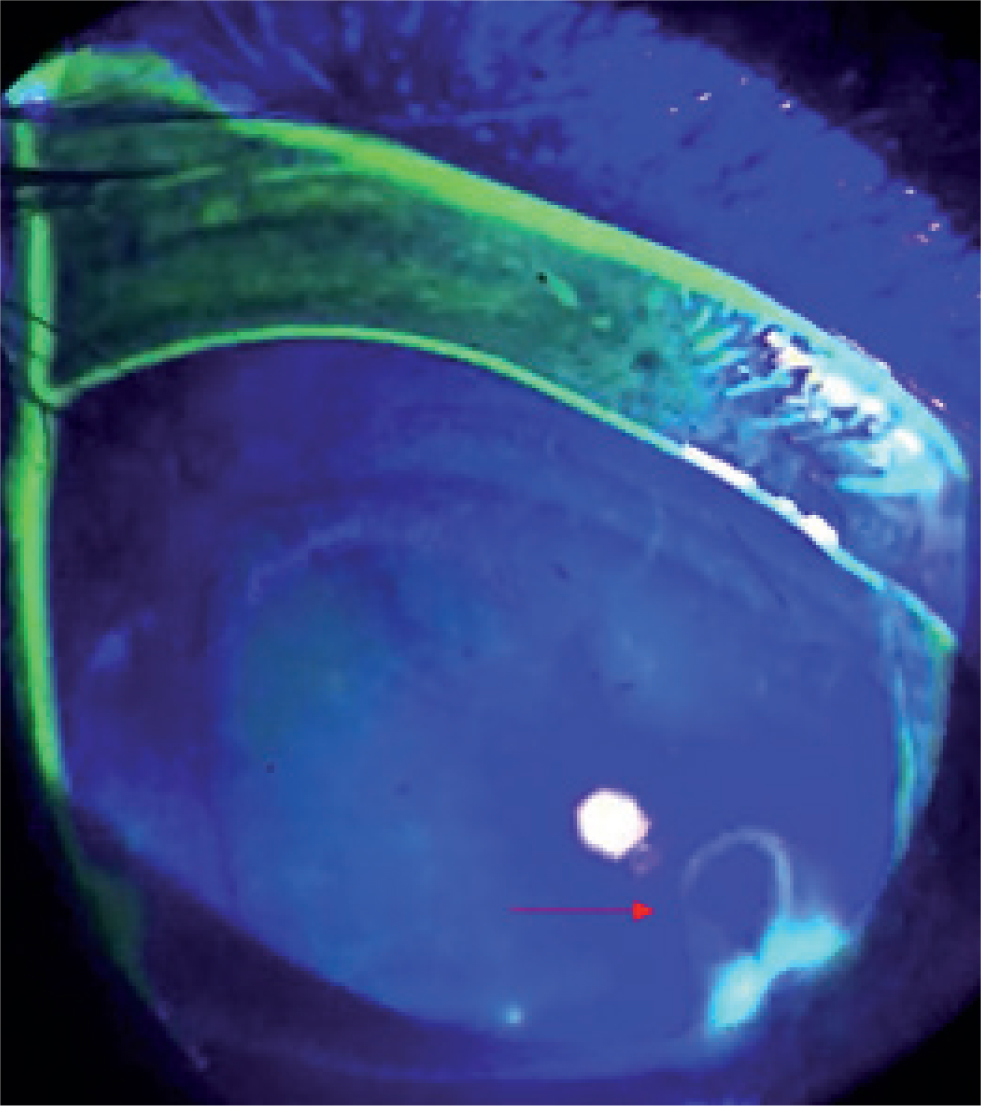
It is important to evaluate corneal integrity and whether any sign of corneal perforation is present. A positive Seidel test can help determine whether a full-thickness perforation is leaking aqueous humour, but a negative test cannot definitively rule this out because of the ability of full-thickness wounds to self-seal (Hamill, 2002). To perform the Seidel test, a substantial amount of fluorescein is applied to the affected eye and distributed by a ‘forced’ blink motion. The corneal wound will retain fluorescein, but any leaking aqueous will dilute the tear film. Consequently, a dark rivulet will be visible at the penetration site (Figure 5). A cobalt blue light source, such as a Woods lamp or slit-lamp, can enhance this phenomenon (Whitley and Hamor, 2021). It may be necessary to manually keep the eyelids open for several seconds when there is a partial leakage. The presence of a leak and the risk of an anterior chamber collapse should be considered an ophthalmic emergency (Jones, 2012).
In addition to looking for fibrin or blood in the anterior chamber, the examiner should also be alert for the presence of dyscoria, anterior synaechia, iritis or iris prolapse, as well as any damage to the lens or lens capsule (Chang et al, 2012; Jones, 2012; Maggs, 2016; Whitley and Hamor, 2021).
Gonioscopy describes the technique that allows examination of the anterior face of the iridocorneal angle and ciliary cleft. This technique is used primarily to determine whether the angle is open, narrow or closed. Additionally, gonioscopy may be used to identify the presence of foreign material in the iridocorneal angle (Featherstone and Heinrich, 2021).
Advanced imaging
Some grass types produce seed-carrying, barbed plant material called grass awns, or foxtails. They are among the most common causes of foreign body-related health problems in small companion animals, with reports of ear, nose, feet, eye, lumbar spine and thoracic cavity involvement (Dennis et al, 2005; Tovar et al, 2005). Different imaging modalities have been used to identify and aid in the removal of grass awn foreign bodies from different sites in dogs and cats, including radiography, ultrasonography, computed tomography (CT) and magnetic resonance imaging (MRI) (Lybaert et al, 2009).
The type of foreign body material determines which imaging modality is most useful for identification (Pot et al, 2021). Most foreign bodies are generally not visible on plain radiographs, but metallic material can easily be identified. Because of the potential for foreign body displacement under the influence of a strong magnetic field, MRI scans are contraindicated when there is a suspicion of metallic foreign body (Malhotra et al, 2011) and CT would be more useful in these cases (Pokhraj et al, 2014). Ultrasonography of the eye and orbit can provide a significant amount of information. However, the bony margins of the orbit prevent a clear view of the entire periocular and orbital structures (Wait et al, 2018). Nevertheless, ultrasound seems to be a relatively sensitive diagnostic tool in determining the presence of a retrobulbar abscess or cellulitis (Stades et al, 2003; Pot et al, 2021).
Larger foreign objects can also be located using this imaging modality. However, foreign body tracks, created by transient penetration of a sharp object, may be impossible to differentiate ultrasonographically from small and/or linear foreign bodies (Ruth et al, 2014).
Ocular and/or orbital foreign bodies may appear differently on ultrasound, depending on the extent of associated tissue damage and the nature of the foreign body. Foreign material is generally identified as hyperechoic linear structures with distal signal attenuation or shadowing. The presence of an anechoic halo, caused by accumulation of inflammatory fluid and surrounding soft tissue reaction, is a common sonographic feature associated with foreign bodies (Gnudi et al, 2005). It is not uncommon for metallic foreign bodies to have very pronounced acoustic shadowing, whereas plant material (Ruth et al, 2014) and wooden foreign bodies may not be as readily apparent (Pot et al, 2021). If a thorn is embedded in the cornea, no direct pressure should be applied to the corneal surface (Jones, 2012).
In patients that show clinical signs consistent with extraorbital involvement, CT or MRI studies are indicated to evaluate the extent to which periorbital tissues are affected (Kneissl et al, 2007), to assess the size, number and exact localisation of retrobulbar foreign bodies (Ruth et al, 2014; Pot et al, 2021), and to determine the prognosis (Kneissl et al, 2007). A CT scan can detect foreign bodies directly if they are sufficiently dense, such as metal, glass, or bone. Plant material, wood and plastic may appear as a filling defect on MRI after contrast administration with a rim of contrast-enhancing reactive tissue around them (Stades et al, 2003). The use of MRI and CT for detecting intraocular foreign bodies has not been described in animals. While these may be detectable in theory, as with ultrasonography, they could be difficult to distinguish from tissue reactions (Ruth et al, 2014). Ultrasonography, CT and MRI may be complementary in certain situations; there have been cases in which ultrasound depicts the foreign body and CT or MRI do not, and vice versa (Pot et al, 2021).
Treatment
Copious irrigation will flush out small conjunctival and third-eyelid foreign bodies (Hartley, 2014). Small conjunctival incisions, such as those caused by grass seed foreign bodies, do not require suturing (Turner, 2014). As the conjunctiva heals very quickly with hardly any scarring, minimal treatment with topical broad-spectrum antibiotics and systemic analgesia would only be necessary in cases of sharp conjunctival foreign body trauma. However, a conjunctival wound may appear minor in cases of penetration by high-velocity foreign bodies such as shotgun pellets, and a careful assessment of the globe, orbit and periocular structures must be performed to detect any further injuries (Peruccio, 2016). In case of a foreign body lodged in the lacrimal sac, simple nasolacrimal flushing may dislodge the foreign object into the lacrimal punctum, allowing it to be removed. However, an incision into the lacrimal sac or nasolacrimal duct may be required. Upon reaching the bony nasolacrimal canal, foreign bodies are difficult to remove and require partial excision of the maxillary bone. In order to prevent stricture formation, a postoperative stent must be placed for 3–4 weeks to allow healing of the incised canaliculus or nasolacrimal duct (Peruccio, 2016).
Most small, superficial adherent corneal foreign bodies can be removed by hydropulsion with a fine stream of sterile saline directed forcefully at the ocular surface after application of a topical anaesthetic (Labelle et al, 2014). It is important to assess the corneal integrity before using forceful streams of fluid, as these may rupture a deep ulcer (Maggs, 2016). If the foreign body is partially embedded in the corneal stroma and partially protruding externally, grabbing it with forceps is very tempting. However, this should be avoided as the foreign material may be pushed further into the stroma, exacerbating tissue damage (Whitley and Hamor, 2021). When a forceful jet of fluid is unsuccessful at rinsing off the foreign body, the tip of a fine hypodermic needle (23 or 25 gauge) may be directed at 90° to the entry track of the foreign body to lift the edge of the object (Figure 6). Using a cotton-tipped applicator to remove adherent foreign bodies often results in further embedding the object and should be avoided (Wiliams et al, 2002; Maggs, 2016). In case a foreign body created a partial-thickness corneal laceration, careful trimming of the loose tissue is required. After debridement, a Seidel test can be performed to ensure the laceration remains partial-thickness (Macsai, 2000). Superficial corneal lesions are treated with topical antibiotics. If secondary anterior uveitis is present, topical mydriatics are also indicated (Gelatt and Brooks, 2011).
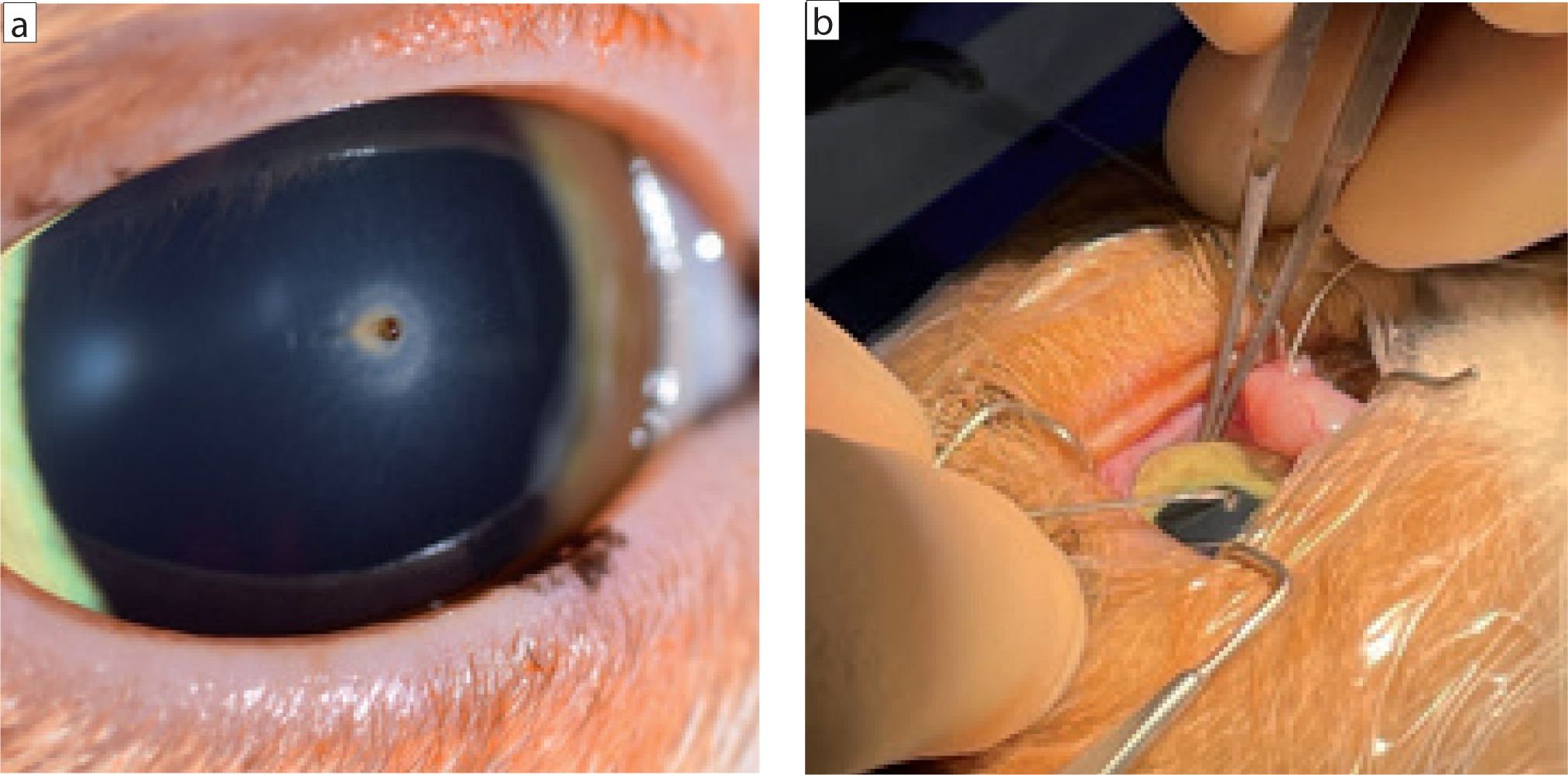
Whenever a stromal foreign body is deeply embedded and the tract has sealed, a superficial keratectomy of the overlying cornea may be required (Whitley and Hamor, 2021). Depending on the size and shape of a perforating corneal foreign body, its surgical removal is approached from the corneal surface or from the anterior chamber. External removal is usually recommended when the largest part of the corneal foreign body is anterior to Descemet's membrane. However, if the largest part is protruding into the anterior chamber, entry through a limbal or peripheral corneal incision over the long axis of the foreign body is necessary as this is less traumatic (Gelatt and Brooks, 2011).
Focal perforating corneal or scleral injuries that seal spontaneously and do not affect any other intraocular structure may be treated medically. Topical broad-spectrum antibiotics and non-steroidal anti-inflammatories are usually the treatment of choice. Ideally, antibiotic selection should be based on cytology findings and culture results (Saphiro et al, 2005; Grundon et al, 2010). Immediate surgical removal of corneal foreign bodies provides the best results before corneal transparency decreases and secondary iridocyclitis intensifies (Gelatt and Brooks, 2011).
Small, deep or perforated corneal wounds of 3mm or less with firm healthy margins may be closed by direct suturing, using 8/0 to 10/0 suture material, with a spatulated needle (Gelatt and Brooks, 2011; Whitley and Hamor, 2021). Stromal deficits of more than 50% and larger perforations will require the additional placement of a flap or graft (Maggs, 2016; Whitley and Hamor, 2021). Diverse grafting techniques have been described for the treatment of larger full-thickness corneal defects (Bussieres et al, 2004; Lacerda et al, 2013). Placement of conjunctival or corneal flaps or grafts requires advanced training, an operating microscope, proper instrumentation and suture material, and basic microsurgical knowledge (Maggs, 2016). Deflated eyes can be difficult to operate on. Therefore, it is critical to prepare the graft before removing a perforating foreign body. In this way, immediate tectonic support can be guaranteed and potential sequelae of prolonged anterior chamber deflation, such as anterior synechiae and endothelial damage, can be minimised (Macsai, 2000). Filling the anterior chamber with a visco-elastic substance will make it easier to incise the cornea and allow suturing (Whitley and Hamor, 2021).
Unless a gaping corneal wound or a very large foreign body is present, a foreign body located completely within the anterior chamber should be removed from a site distant from the entrance wound to minimise scarring and damage to endothelial cells (Lit and Young, 2002). Saline or viscoelastics can be used to dislodge foreign bodies that are located near the iridocorneal angle (Hendrix, 2021). After foreign body removal, the remaining viscoelastic material will be flushed out in most cases via irrigation-aspiration (Michau, 2021). An anterior vitrectomy is indicated when the vitreous protrudes into the pupil or the anterior chamber during anterior segment surgery (Boevé and Stades, 2021). Although not ideal, small inert inorganic foreign bodies, such as lead, glass or plastic, may be left in place when finances are limited or restrictions do not allow for immediate surgical removal (Hendrix, 2021). All deep penetrating and perforating wounds to the eye should be considered infected and treated accordingly with topical and systemic medication (Hendrix, 2021).
Foreign material is rarely retained within the lens, but perforating foreign bodies may affect the lens integrity. Lens capsule rupture allows the release of lens proteins within the anterior chamber with secondary phacoclastic uveitis and glaucoma (Hendrix, 2021). Prophylactic lens removal has been widely advocated for in cases of lens capsule tears greater than 1.5mm, or with substantial disruption of the lens cortex (Davidson et al, 1991). However, a later retrospective study concluded that animals with lens capsule tears greater than 1.5mm had a better outcome with medical management alone than those that also underwent lens surgery following corneal repair (Paulsen and Kass, 2012).
Removal of a vitreal foreign body depends on whether the material is surgically accessible, as well as the type of material and its interactions with the intraocular tissues. Inert inorganic materials are best left in situ. Other materials, such as organic matter, iron and copper are poorly tolerated and can be removed via vitrectomy (Heinrich, 2014). Organic vitreal foreign bodies usually carry a grave prognosis. They are often associated with endophthalmitis and may progress to a vitreal abscess or panophthalmitis (Ofri, 2016).
It may be necessary to enucleate an eye if the globe has undergone extensive trauma and cannot be repaired successfully, and if there has been loss of intraocular tissues with chronic inflammation and blindness (Whitley and Hamor, 2021). In cases where a retrobulbar abscess occurs secondarily to an orbital foreign body, the first and most important step is drainage, which is performed under general anaesthesia. To prevent recurrence of the infection, the foreign material must be surgically removed. Advanced imaging may aid in its identification and localisation (Pot et al, 2021).
Surgical retrieval of an identified orbital foreign body could be successful via abscess drainage in some cases. In other cases, surgical exploration via orbitotomy and flushing of the retrobulbar space might be indicated (Tremolada et al, 2015).
Prognosis
Prognosis depends on many factors, including the type of foreign body, length of the wound, time between injury and repair, structures affected and whether the foreign body is retained. Small corneal injuries or large lacerations with minimal intraocular damage usually have a good prognosis following appropriate treatment. Large corneal or scleral tears with iris prolapse and the presence of vitreous or lens material within the wound, or on the ocular surface, indicates a poor prognosis (Pont et al, 2016). In a recent study, the nature of the trauma (cat scratch versus thorn injury) was not associated with vision loss (Braus et al, 2017).
In some cases, traumatic perforation of the ocular structures may lead to fulminant endophthalmitis and may result in globe loss. Lens injury with secondary phacoclastic uveitis or lens abscessation carries a grave prognosis, since it may be refractive to medical treatment, and secondary complications such as glaucoma or retinal detachment are not unusual (Hendrix, 2021). A particular condition termed ‘septic implantation syndrome’ results from traumatic inoculation of microorganisms into the lens cortex and may develop weeks to months after inoculation. In cases of a capsular tear, fibrinous exudate on the lens capsule associated with a focal cataract may be noticed (Bell et al, 2013). Late diagnosis of septic implantation syndrome carries a less favourable outcome, even following surgical lens extraction with intraocular and systemic antimicrobial therapy (Dubielzig and Pirie, 2005). Other potential complications of perforating trauma include optic nerve degeneration, glaucoma and retinal detachment (Hendrix, 2021).
Feline ocular post-traumatic sarcoma is a specific condition encountered in cats that is associated with perforating ocular trauma or severe intraocular disease (Dubielzig et al, 2010). Previous lens rupture is reported in most cases and these tumours are thought to have a lens epithelial origin (Zeiss et al, 2003). Lens epithelial cells may undergo transformation to spindle cells after traumatic or non-traumatic lens injury. The prognosis for this condition is poor. Regional lymph node dissemination and pulmonary metastasis are rare, but extension beyond the sclera and into the optic nerve is common (Dubielzig et al, 1990).
Conclusions
Foreign body injuries are common in small animals and the presentation, outcome, and prognosis varies. Animals presenting with such injuries should be treated as an emergency and undergo a complete ophthalmic examination as soon as possible. Young working breeds are typically more affected and organic materials tend to be less tolerated. Prognosis depends on the zone of injury, type and size of foreign body, and the subsequent complications. Increased awareness of the improved surgical techniques and the importance of prompt treatment could improve the outcomes of foreign body injuries.
KEY POINTS
- Foreign bodies affecting small animals more commonly consist of plant materials and are not well tolerated.
- The breed (English Springer Spaniels, Labrador Retrievers) and age (less than 5 years) are considered predisposing factors.
- Foreign bodies should be ruled out in cases of acute ocular discomfort, such as blepharospasm, enophthalmos, third eyelid protrusion, chemosis, conjunctival hyperaemia and lacrimation.
- The location, type, size, depth and angle of penetration of the foreign body can be determined using adequate magnification and the Seidel test.
- The prognosis largely depends upon multiple factors.
- Referral to an experienced ophthalmology specialist is necessary in difficult surgical cases.


