This self-assessment will consider a case of corneal ulceration to critically assess its progression over time, and understand how steps could have been performed differently to change the final outcome. I will provide the final outcome from the start: it is arguably easier to look at a case retrospectively, and by giving you the outcome, it will be possible to see if that changes your decision-making process as the case unfolds.
Patient outcome
The patient required surgical correction of the ulcer via a conjunctival flap. At the follow-up, 1 week after surgery, a Schirmer tear test (STT) was performed in the affected eye, and revealed a reading of 8 mm/min, confirming a diagnosis of kerato-conjunctivitis sicca (KCS) in this eye.
Initial assessment of the ulcer
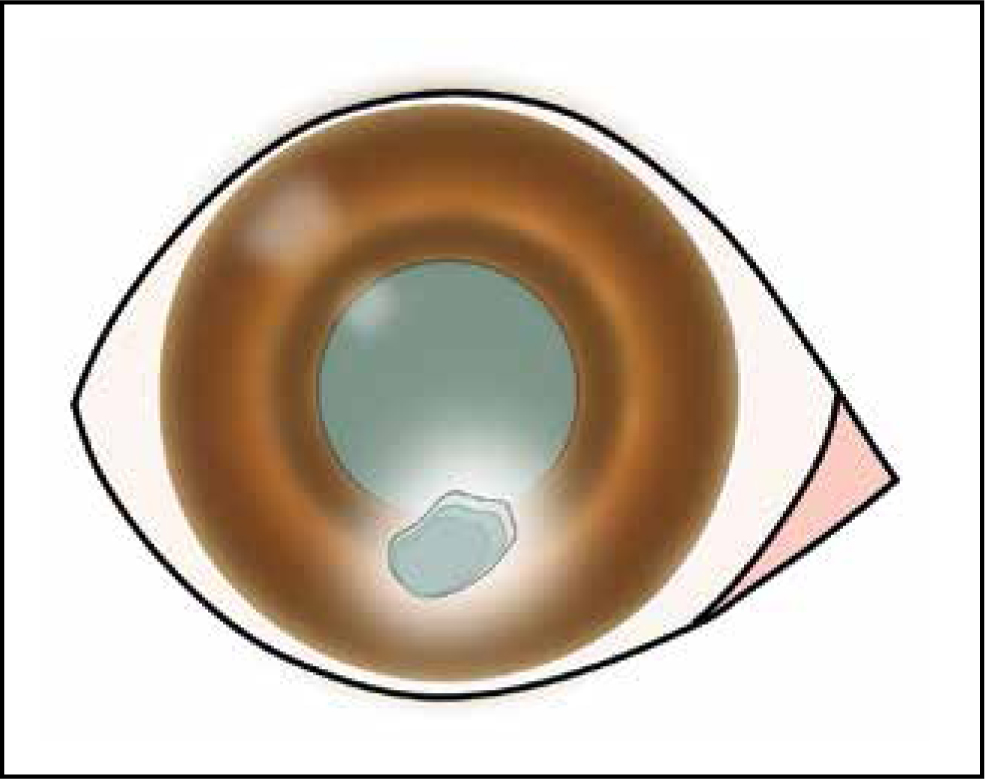
You are presented with an 8-year-old, female spayed, West Highland white terrier. Close examination of the right eye showed a superficial stromal corneal ulcer, approximately 5 × 3 mm on the ventral half of the cornea (Figure 1). There were no signs of foreign bodies, or abnormal hairs abrading the corneal surface. There was moderate corneal vascularisation and bulbar conjunctival hyperaemia, and mild peri-ocular mucoid discharge. Treatment with fusidic acid ointment (Isathal®, Dechra) was started twice daily to the affected eye, as well as oral meloxicam (Metacam®, Boehringer Ingelheim Animal Health) once daily per os (PO), and amoxicillin/clavulanic acid (Synulox®, Zoetis) twice daily PO.
Question 1 — Were all necessary diagnostic tests performed?
Answer — There are a few key tests missing. As we now know, the patient was later diagnosed with KCS. This highlights the importance of performing a STT before any other test (note: in addition to the affected eye, always perform the test on the contralateral ‘healthy’ eye to establish the pre-ulcerative baseline tear production). Additionally, any complicated ulcer (stromal ulcers, chronic ulcer, etc) should have, at the very least, a corneal cytology performed to guide the choice of antibiotic, and if possible, culture and sensitivity testing to confirm the chosen antibiotic.
Question 2 — Was the topical treatment appropriate?
Answer — In the UK, fusidic acid is approved for use in conjunctivitis in dogs, and therefore an appropriate first-line treatment according to the prescribing cascade. However, as mentioned above, corneal cytology or culture and sensitivity were not performed, and therefore, we do not know the most likely bacteria present in this ulcer (if any). As such, we do not actually know if this antibiotic is appropriate or not. Fusidic acid also has a limited spectrum of activity against most Gram-negative bacteria.
Question 3 — Was the oral treatment appropriate?
Answer — The microbial agents present in this case is not known. Additionally, this oral antibiotic has not been shown to achieve therapeutic concentrations in the tear-film, and consequently will not reach the ulcer. Therefore, use of oral antibiotics is not appropriate in this case, and may contribute to antibiotic resistance. The oral non-steroidal anti-inflammatory drug (NSAID) emloxicam, on the other hand, was absolutely appropriate, as these drugs will increase patient comfort, and improve any reflex uveitis, which may be present secondarily to the ulcer, while not affecting the re-epithelialisation process (unlike topical NSAIDs would).
Review one
The ulcer still remained fluorescein positive, despite the original treatment, so the decision was made to debride the ulcer, and change antibiotic treatment to ofloxacin eye drops (Exocin®, Allergan) four times daily to the affected eye, because the healing process had not progressed.
Question 4 — Why did the ulcer not improve?
Answer — It is crucial to try, as best as possible, to determine the cause of the ulcer, and target treatments accordingly. Inappropriate treatment can lead to delays in healing or even deterioration of the ulcer.
Here, the clinician attributed the lack of healing to an ineffective antibiotic. It is important to understand that antibiotics do not ‘heal’ ulcers; they prevent contamination of the exposed stroma, allowing the patient's normal healing processes to take place. Therefore, it is the patient that heals the ulcer, not the antibiotic. Bearing this in mind, in the present case we now know that the patient had KCS, severely impairing the patient's own mechanisms for ulcer re-epithelialisation. Thus, lack of improvement of the ulcer was not necessarily because of ineffective antibiotic treatment, but rather the lack of treatment directed to the inciting cause, KCS.
Question 5 — Was debridement a good choice to speed up healing?
Answer — Not in this case, no. There is a common misconception that debridement ‘speeds up healing’, a bit like debriding devitalised tissue at the edge of a soft tissue wound. However, the objective of corneal debridement is to improve the adhesion between the epithelium and anterior stroma specifically in cases of spontaneous chronic corneal epithelial deficits (or indolent ulcer), where this adhesion is abnormal. Debridement should therefore be reserved solely for these cases. In no situation is it used to simply ‘speed up the healing process’. In the current patient, the ulcer was not a spontaneous chronic corneal epithelial deficit, it was in fact a stromal ulcer, and therefore debridement of any form should be avoided at all costs.
Question 6 — Was the change in antibiotic appropriate in this case?
Answer — Often clinicians are tempted to change antibiotic, when improvement is not seen, for a ‘stronger antibiotic’. The most important factor to consider is: antibiotics do not vary in strength but in spectrum of activity. A change in antibiotic may very well improve the situation, although this may be because of a more appropriate cover, rather than the fact that it was ‘stronger’. Caution, if the change in antibiotic is not guided by culture and sensitivity testing, or at the very least by corneal cytology, it is a mere guessing game as to which antibiotic would be effective. Some bacteria may be resistant to antibiotics perceived as ‘stronger’, and in these cases a switch to these can lead to catastrophic outcomes for the cornea.
Review two
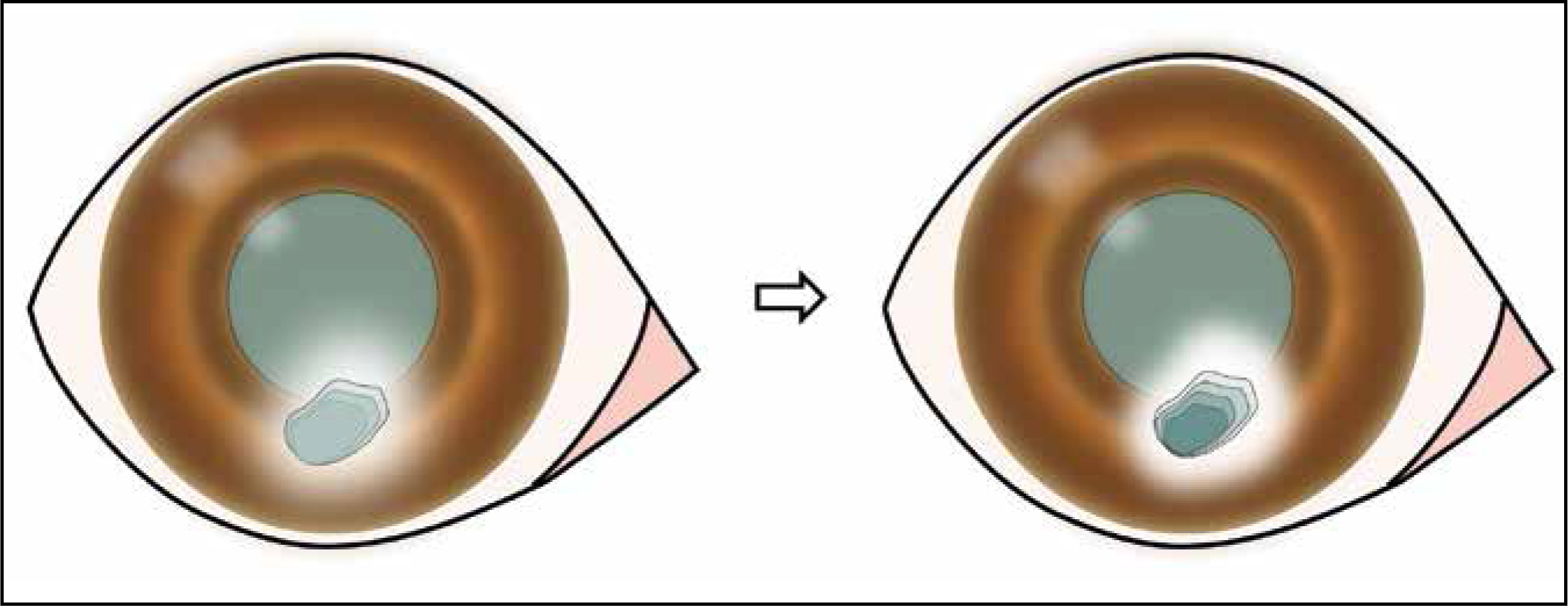
On the review that finally led to the decision for surgery, the following was seen. The ulcer had significantly deepened and was now mid-stromal (Figure 2). There was a surrounding gelatinous-looking cornea. The patient had marked blepharospasm and epiphora, and was very reluctant to handling around the affected eye. Diagnosis of a ‘melting’ corneal ulcer was made, and the patient was referred to surgery.
Question 7 — What could have caused the ‘melting’, or keratomalacia, surrounding the ulcer?
Answer — Keratomalacia is the loss of rigidity and structure of the corneal stroma. It is caused by collagenases produced by the host (neutrophils, keratocytes, corneal epithelial cells), and/or microorganisms.
Question 8 — Could this have been avoided? How?
Answer — As mentioned, there are intrinsic and extrinsic causes for melting. Unfortunately, even if the potential for melting is identified early on, and appropriate treatment started, melting can develop regardless. However, if prompt treatment is commenced, melting can be avoided or reduced in severity. Treatments include appropriate antibiotics to reduce extrinsic causes of melting (bacteria), and specific anticollagenase treatment such as serum, N-acetylcysteine, EDTA, tetracycline antibiotics.
Surgery
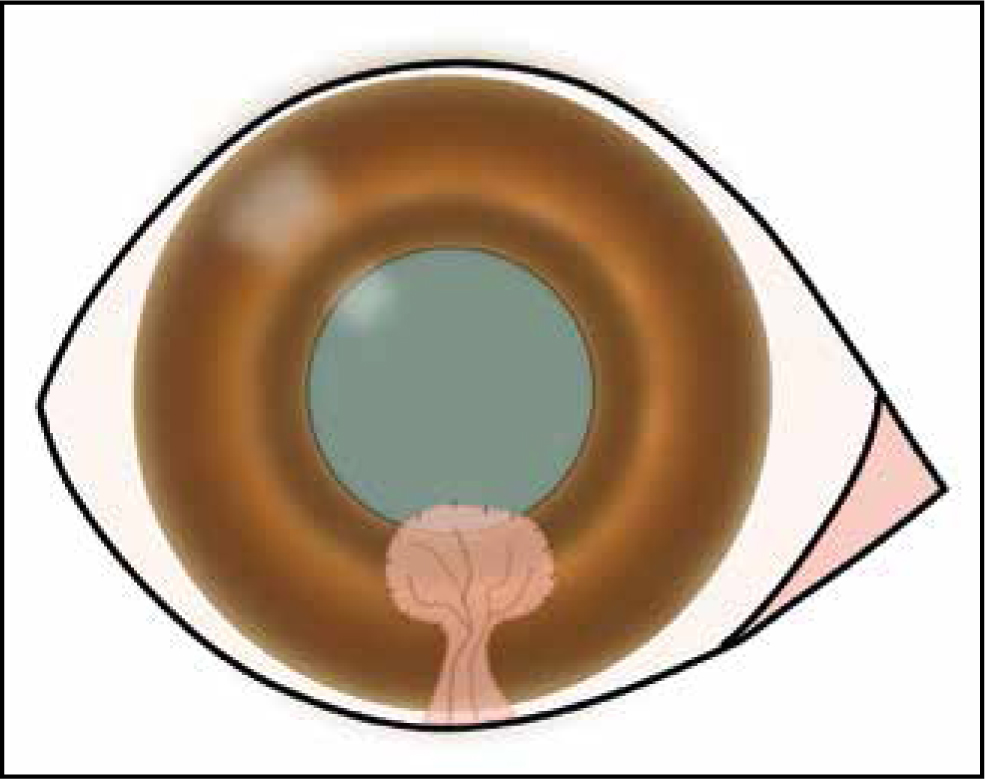
The area of ‘melting’ was surgically debrided, and a conjunctival flap placed over the deficit (Figure 3). The patient was discharged with ofloxacin three times daily to the affected eye, and meloxicam once daily PO.
Question 9 — Was the type of surgery performed the most indicated?
Answer — Selection of surgical technique is dependent on the type/location of the ulcer, but also very much on surgeon experience, confidence and available equipment. It is also very important to consider the postoperative outcome. Is the patient going to be able to see through the repair? What is the likelihood of success vs potential risks? We must think twice before performing a risky surgery if the patient will ultimately become blinded by a graft or scarring for example, or if there are significant expected complications such as endophthalmitis and glaucoma for perforated eyes.
In the present case, the ulcer was ventral, and mid-stromal. We also now know that the patient has KCS, so healing of the ulcer was certainly going to be delayed without surgical intervention. A conjunctival graft was selected as this would not interfere with the patient's visual axis, the ulcer did not require too much tectonic support (mid-stromal in depth), and this was the most familiar technique to the surgeon.
Taking the above into consideration, this was an appropriate technique to perform. However, collection of a sample for cytology and culture and sensitivity would again have been advised during surgery to confirm antibiotic choice.
Review three
At the postoperative review 1 week following surgery, as mentioned initially, a STT was performed in the affected eye and revealed a reading of 8 mm/min. The operated cornea was fluorescein negative. The medication was changed to cyclosporin twice daily to the affected eye, tear replacers ad lib, and the remainder of the medication was discontinued.
Question 10 — Would you have performed any further tests at this stage?
Answer — It is crucial to also check the contralateral ‘healthy’ eye when assessing STTs, as often KCS is a bilateral condition.
Question 11 — Do you agree with the medication change?
Answer — The change in medication was entirely appropriate, however it is possible that the contralateral eye may also require cyclosporin treatment and tear film supplementation.
Summary
On reflection, did knowing the outcome of the case change the way you approached this case? Would the patient have ended up going to surgery if we had diagnosed the KCS from the start? Is this something that you could take into practice the next time you see a patient with an ulcer? Table 1 summarises the approach that was originally taken, and the steps that could have instead been performed to improve the final outcome in this case.
Table 1. A summary of the dog's assessment and treatment
| Step | Original approach | Ideal approach |
|---|---|---|
| First assessment |
|
|
| Review 1 |
|
|
| Review 2 |
|
|
| Surgery |
|
|
| Review 3 |
|
|
Not all ulcers are caused by KCS, however this exercise does show the importance of considering all the differentials in the beginning of the case and how dramatically this can affect its outcome.


