The use of peripheral nerve blocks in people is an effective technique to provide intraoperative and postoperative analgesia (Roberts and Cowen, 2016; Hutton et al, 2018). There are increasing numbers of publications detailing techniques for performing peripheral nerve blocks in dogs, specifically in comparison to other well-established locoregional anaesthesia techniques such as epidural anaesthesia (Campoy et al, 2012).
The pelvic limb is innervated by the lumbar and sacral plexuses, which in turn give rise to the femoral and sciatic nerve, respectively (Gurney and Leece, 2014). When a local anaesthetic is instilled around these nerves, analgesia can be provided to the majority of the pelvic limb (Dyce et al, 2010; Portela et al, 2018). Multiple approaches can be used to instil local anaesthetic around the sciatic nerve, which can affect the structures blocked. Overall, the sciatic nerve block performed by any technique should result in anaesthesia of the caudolateral stifle, some intra-articular structures, joint capsule, tibia, tarsus, metatarsus and digits. The lateral approach will also result in anaesthesia of the muscular branch. The transgluteal approach provides anaesthesia of the ischiotibial muscles and some sensory branches of the coxofemoral joint (Campoy and Mahler, 2013). The lateral pre-iliac approach to the psoas compartment should provide anaesthesia of the hemipelvis, femur, femorotibial joint, skin of the dorsomedial tarsus and first digit (Campoy and Mahler, 2013; Portela et al, 2013a, 2013b).
A large volume of literature detailing different approaches to the sciatic nerve block in dogs is available (Portela et al, 2018). There are currently no clinical studies directly comparing the different approaches.
The primary aim of this study was to determine if there were any clinically significant differences between the transgluteal and lateral approach to the sciatic nerve block in terms of postoperative analgesic requirements, when performed alongside a psoas compartment block. The secondary aim was to determine if there was any significant difference in ease of performing the nerve block. It was hypothesised that there would be no difference between approaches.
Methods
Animals
Ethical approval was obtained from the University of Bristol Animal Welfare and Ethical Review Body (VIN/17/045). The study was undertaken at Langford Vets Small Animal Referral Hospital between April 2018 and January 2019.
The study was a prospective, blinded, randomised, clinical trial involving client-owned dogs undergoing a unilateral tibial plateau levelling osteotomy. Dogs were eligible for inclusion if they were scored as American Society of Anaesthesiologist (ASA) category I-II. Exclusion criteria were dogs requiring systemic opioids for other reasons, those unable to receive non-steroidal anti-inflammatory drugs (NSAIDs), dogs where their body condition score (BCS) prevented palpation of anatomical landmarks and dogs whose temperament precluded safe handling. Written informed owner consent was obtained. The number of dogs included in this study was based on a study comparing epidural analgesia with peripheral nerve blocks (Campoy et al, 2012). No power calculation was performed because of a lack of available data.
Study protocol
The dogs were fasted overnight before anaesthesia, with water available until premedication. Dogs were randomly assigned to one of two groups by drawing paper out of an envelope. The envelope contained 42 strips of paper, 21 per group. Group A received a sciatic nerve block via the transgluteal approach (Mahler and Adogwa, 2008). Group B received a sciatic nerve block via the lateral approach (Campoy, 2010).
An intravenous catheter was placed before premedication. Premedication consisted of intravenous 0.3 mg/kg methadone (Comfortan® 10 mg/ml, Dechra, Netherlands) and 2.5 μg/kg dexmedetomidine (Dexdomitor® 0.5 mg/ml, Zoetis, USA). General anaesthesia was induced with alfaxalone (Alfaxan® 10 mg/ml, Jurox, Australia) IV to effect. Anaesthesia was maintained with isoflurane vaporised in oxygen.
All blocks were performed by one of two anaesthesia residents. This allowed continued enrolment of cases onto the study in the event that one resident was not in the clinic. Both residents were at the same stage in their residencies (second year) and had been trained to perform both blocks. The anaesthetist monitoring the anaesthetic was not present while the blocks were performed so they were blinded to treatment.
The psoas compartment block was performed under nerve stimulation using the lateral pre-iliac approach (Portela et al, 2013b). The sciatic nerve block was performed under nerve stimulation, using either the transgluteal or lateral approach, as described by Mahler and Adogwa (2008) and Campoy (2010), respectively. A lack of nerve stimulation at 0.3 milliamp (mA) was the lowest current used to perform the block, to reduce the chance of intraneural injection of bupivacaine. A total volume of 0.2 ml/kg bupivacaine 0.5% was used, divided equally between the injection sites. The number of attempts, total time from first penetration of the skin to injection of bupivacaine, and the minimum currents (mA) at which the injection was performed were recorded for the sciatic nerve block. When the time taken to perform the sciatic nerve block reached 5 minutes, the block was abandoned and recorded as a failure to perform the block.
The requirement for additional analgesia during surgery was left to the discretion of the anaesthetist monitoring the dog. If the anaesthetist deemed the patient to be responding to noxious stimulation, methadone 0.1 mg/kg was administered intravenously. Immediately following tracheal extubation, 0.2 mg/kg meloxicam (Metacam 5 mg/ml, Boehringer Ingelheim, Missouri) was administered intravenously. If the dog was already on an NSAID this was continued when the next dose was due.
Pain was scored using the Short-Form Glasgow Composite Measure Pain Scale (SF-CMPS) every 2 hours, starting 2 hours after tracheal extubation. Those performing pain assessment were blinded to the treatment group. If the score was greater than or equal to 5/20 or 6/24 (depending on whether the dog was ambulatory or not) methadone 0.2 mg/kg was administered intravenously. The dog's pain was reassessed 30 minutes later. A further 0.1 mg/kg methadone was given if the dog's pain was still over the threshold and then reassessed after a further 30 minutes. If the pain score was still over the threshold, the dog was removed from the study and an anaesthetist contacted regarding ongoing pain management.
The study ended 12 hours after extubation. Analgesia continued as deemed appropriate by the anaesthetist. The neurological function of the dog's limb was assessed 24 hours after the operation.
Statistical analysis
Statistical analysis was carried out using IBM SPSS Statistics 24. Categorical and count data are presented as the median and range. Continuous data are presented as the mean±standard deviation (SD) (range). Analysis of categorical data (BCS, sex, mA, methadone consumption intraoperatively and postoperatively, resident) and count data (number of attempts through skin) vs block performed was performed using a Pearson Chi-Squared test.
Absolute pain score was not analysed, as dogs were not always removed from their kennel. As such, pain scoring was used to determine whether methadone was required or not. This was analysed with a Pearson Chi-squared test. Analysis of continuous data such as age, bodyweight, time taken to perform the block were compared between groups by a bootstrapped independent t-test with equal variances.
Time to postoperative methadone administration was analysed using Cox-regression analysis, with the assumption all dogs dropped out at 12 hours (the end of the study). The 95% confidence intervals (CI) were calculated using a bootstrapped one-sample t-test.
Results
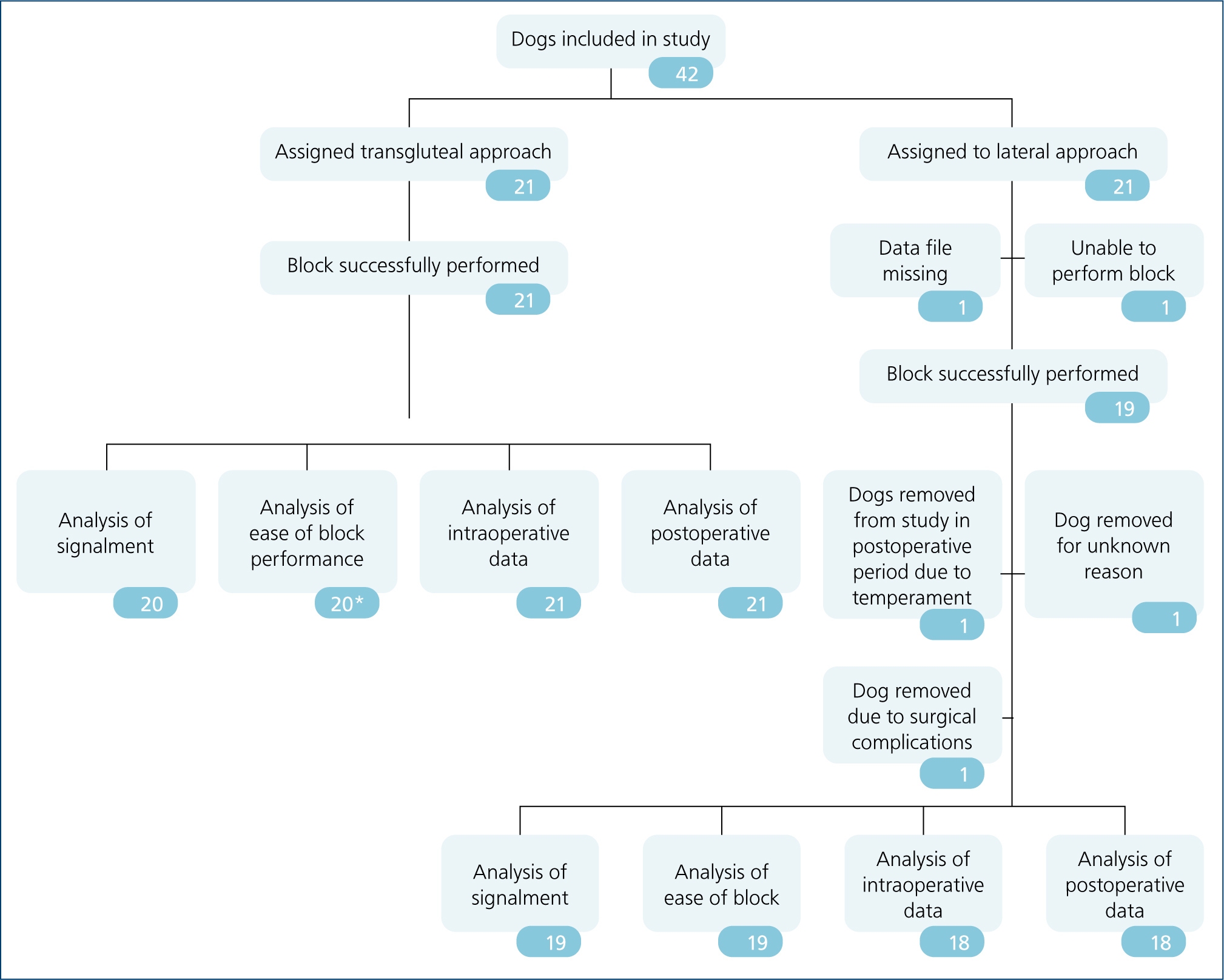
In total, 42 dogs were enrolled in the study, with six dogs being removed from the analysis. Figure 1 gives details.
Signalment
Of the 41 dogs with data available regarding signalment, 25 breeds were represented, with crossbreeds being most common (9/41, 22%). There were 12 neutered females, 1 entire female, 17 neutered males and 11 entire males. There was no significant difference between two groups (P=0.378). Table 1 presents remaining data. There was a significant difference between the residents that performed the blocks, with resident RT performing more in the lateral group and resident DLC performing more in the transgluteal group (P=0.008).
Table 1. Analysis of continuous data for signalment
| Group (number in group) | Range | Mean (±SD) or median | 95% confidence interval | P value |
|---|---|---|---|---|
| Age | ||||
| Overall (41) | 12–131 months | 68 (±30) | 58–77 | 0.008* |
| Transgluteal approach (21) | 12–88 months | 58 (±23) | 49–68 | |
| Lateral approach (20) | 20–131 months | 78 (±33) | 64–92 | |
| Weight (kg) | ||||
| Overall (41) | 5.2–86 kg | 29.3 (±18.6) | 24–35.4 | 0.080 |
| Transgluteal approach (21) | 6.7–54.3 kg | 24.5 (±13.6) | 18.8–30.8 | |
| Lateral approach (20) | 5.2–86 kg | 34.4 (±21.2) | 26.1–43.8 | |
| Body condition score out of 9 | ||||
| Overall (34) | 4–7.5 | 6 | NA | 0.765 |
| Transgluteal approach (19) | 4–7.5 | 5 | NA | |
| Lateral approach (15) | 4–7.5 | 6 | NA |
Intraoperative methadone
Methadone was required in 52% of dogs intraoperatively. There was no difference between groups (P=0.516).
Ease of needle placement
Table 2 shows information regarding the ease of needle placement. There was no difference between the groups for any parameter.
Table 2. Analyses of local anaesthetic block execution
| Group (number in group) | Range | Mean (±SD) or median | 95% confidence interval | P value |
|---|---|---|---|---|
| Time to perform block | ||||
| Overall (40) | 23–300 seconds | 59 (±71) | 65–111 | 0.814 |
| Transgluteal approach (20) | 23–300 seconds | 90 (±74) | 60–125 | |
| Lateral approach (20) | 27–240 seconds | 85 (±68) | 57–117 | |
| Currents | ||||
| Overall (40) | 0.3–0.7 mA | 0.5 | NA | 0.142 |
| Transgluteal approach (21) | 0.3–0.7 mA | 0.4 | NA | |
| Lateral approach (19) | 0.4–0.7 mA | 0.5 | NA | |
| Number of attempts through skin | ||||
| Overall (40) | 1–4 | 1 | NA | 0.506 |
| Transgluteal approach (20) | 1–3 | 1 | NA | |
| Lateral approach (20) | 1–4 | 1 | NA |
NA Not applicable
Postoperative data
Of the 40 dogs that had nerve blocks, three dogs were removed from the study postoperatively (one unamenable to pain scoring, one as a result of surgical complications, and one for unknown reasons). Of the remaining 37 dogs, 18.4% (n=7, 95% CI 7.8–31.6%) required one dose of methadone (transgluteal group: 23.8% (5/20, 95% CI 7–42%); lateral group: 12% (2/17, 95% CI−5 to 29%)). There was no difference between the groups (P=0.341).
The average time to methadone administration was not statistically different between groups; transgluteal 4.8 hours (range 2–10 hours, 95% CI 2.5–7.7 hours); lateral 3 hours (range 2–4 hours, 95% CI 2–4 hours), P=0.513. Cox regression analysis showed no difference in time to methadone administration between groups (P=0.381). There was no difference in postoperative methadone use based on the resident performing the block (P=0.65). No dogs were observed to have any neurological dysfunction 24 hours following the procedure.
Post-hoc sample size calculation
Using postoperative methadone requirement, a post-hoc sample size was calculated. Based on the standard deviation and mean methadone requirement of both groups, and a desired power of 0.95 and α of 0.05 an estimated 279 dogs would need to be included in each group to show a statistically significant difference in postoperative methadone requirement between groups.
Discussion
Overall, these findings show that there was no difference in postoperative analgesia requirement and ease of block placement between the lateral and transgluteal approach to the sciatic nerve block, when combined with a psoas compartment block, within this study population. This suggests that both approaches are appropriate as part of a multimodal analgesic approach during anaesthesia for a tibial plateau levelling osteotomy.
The decision to compare the lateral and transgluteal approaches was twofold. First, they were both used within the clinical setting at the referral hospital. Second, they were the most common approaches used in a survey of veterinary professionals (author's unpublished data). In this study, the difference in anatomical structures blocked by each approach did not have a clinically significant effect. This is likely a result of the considerable overlap of structures blocked by both approaches.
Block success is determined by the location of injection of the local anaesthetic in relation to the nerve. Ideally, the needle tip should be in close proximity to the nerve but not in the nerve itself. Portela et al (2013a) demonstrated that as the needle tip is moved towards the nerve, the current required to elicit a motor response decreases. When the needle was in contact with the nerve, a motor response was elicited at a current below 0.3 mA in 17.2% of patients. Other studies have shown that when the needle is in the correct position, a stimulating current of 0.2–0.5 mA can be used to elicit a motor response (Costa-Farre et al, 2011; Warrit et al, 2019). Voelckel et al (2015) demonstrated no inflammation of the nerve when a stimulating current of 0.3–0.5 mA was used. This suggests that while a lack of motor response at 0.3 mA does not rule out intraneural injection, it reduces the chance.
In this study, all blocks were performed at 0.3 mA or above, and none of the dogs had neurological deficits after 24 hours. In this study, the ability to reach an appropriate stimulating current was used as a method for determining ease of performance. There was no statistical significance between the lateral and transgluteal approaches, suggesting they were similar in ease of performance.
Methadone was required intraoperatively by 52% of dogs. This is considered a higher proportion than expected. While this may seem high given the presence of the blocks, similar intraoperative analgesia requirements have been reported. Boscan and Wennogle (2016) found that 46% of dogs required additional intraoperative analgesia, despite a peripheral nerve block. This is significantly less than those receiving no peripheral nerve block, with 98% requiring additional analgesia (Boscan and Wennogle, 2016). Warrit et al (2019) also demonstrated that those receiving a peripheral nerve block required less fentanyl than those not receiving a block; 90% of dogs not receiving a peripheral nerve block required fentanyl at the point of skin incision compared to 70% of those receiving a peripheral nerve block. In contrast, Bartel et al (2016) demonstrated that no dogs required additional intraoperative analgesia when receiving an ultrasound-guided femoral and sciatic block with bupivacaine in combination with dexmedetomidine.
In thie study, the requirement for intraoperative analgesia could have been in part due to inadequate depth of anaesthesia, complete block failure or only a partial block. As anaesthetic depth was not recorded, this cannot be excluded as a cause. Complete block failure seems unlikely as only seven patients required postoperative analgesia in the 12 hours following extubation. Incomplete blockade of the psoas compartment or sciatic nerve may have resulted in the requirement for additional analgesia. Cathasaigh et al (2018) used ultrasound to confirm the location of the needle tip in proximity to the sciatic nerve, in combination with nerve stimulation. They demonstrated that even when in the correct position, injectate did not distribute evenly around the nerve. In this study, ultrasound was not used to guide injection of bupivacaine and a smaller volume was used. As such the local anaesthetic may not have been deposited evenly around the nerve, affecting efficacy of the blocks.
A single individual was not able to assess every patient at each time point and multiple individuals were involved in patient assessment. While this may introduce some individual variation, all scorers were trained in using the SF-CMPS. By using a validated, objective, tested scoring system, individual variation and bias should have been reduced.
The time to the first dose of rescue methadone was not statistically different between groups. The average time to methadone was longer than the time to methadone reported in other studies. McCally et al (2015) demonstrated a mean time to first rescue analgesia of 2 hours. In the present study, a psoas compartment block was used (0.1 ml/kg 0.5% bupivacaine), whereas McCally et al (2015) used a femoral triangle block (0.2 ml/kg 0.5% bupivacaine). Both were combined with a sciatic nerve block. Therefore, the difference in time to methadone may be attributed to the difference in the block combined with the sciatic block. A retrospective study (Vettorato et al, 2012) analysed the difference between lumbar plexus blocks and a femoral nerve block when combined with a sciatic nerve block. They found that the success rate for the lumbar plexus block was 76% and for the femoral block 85%, based on intraoperative fentanyl consumption. In the present study, methadone was used intraoperatively as rescue analgesia. This could have also been a confounding factor as it may have lasted into the postoperative period and affected the pain scores. This could explain the increased length of time to methadone use in the postoperative period.
Bupivacaine was chosen as the local anaesthetic in this study. The onset time of bupivacaine is 20–30 minutes with a duration of action of 3–8 hours. Cathasaigh et al (2018) demonstrated sensory blockade of 10 hours with ultrasound guided sciatic nerve block, ranging from 4–12 hours, which is longer than the reported duration of action. The findings of our study agree with this study as only 18.4% of dogs required additional analgesia in the 12 hours following tracheal extubation. This suggests that bupivacaine may provide adequate postoperative analgesia for most dogs, based on pain score. However, because of the varying duration of action and the small number of patients that required additional analgesia in this study, assessment was important to ensure patients were not experiencing pain.
Limitations
There were several limitations to this study. The main limitation was the small sample size. No data were available to calculate a sample size, so a similar study was used as a basis for this study. A post-hoc sample size calculation was performed using postoperative methadone requirement. Over 270 dogs would be required per group to detect a difference. This suggests that the difference between the two blocks is small and the use of one technique over another is unlikely to contribute significantly to clinical outcome.
The second limitation was that the study did not assess the efficacy of the psoas compartment block. The analgesia provided by the peripheral nerve block should be the result of the psoas compartment block and the sciatic block combined. If the psoas compartment block was ineffective, this may have contributed to poorer analgesia being provided than if both blocks were effective. No test was used to specifically determine whether the psoas compartment block was effective in all cases before surgery began. This could have resulted in some dogs having an ineffective psoas compartment block, which would have affected the analgesia provided. This then might have affected the results of the sciatic nerve blocks. To minimise this, the same technique for the psoas compartment block was used in both groups and was performed by the same two residents performing the sciatic nerve blocks, who were also trained to perform a psoas compartment block.
A further limitation was the use of methadone intraoperatively. Methadone has a median duration of action of 4 hours in dogs (Murrell, 2011). If rescue analgesia was administered during the procedure, the effect of the methadone will have extended into the postoperative period. As the patients were pain scored for 10 hours following the end of surgery, the effect of methadone should have worn off within 6 hours, resulting in the later pain scores being recorded without any effect from the methadone.
The decision to use methadone was made as it reflected current clinical practice in the hospital. A shorter acting opioid, such as fentanyl, could have been used instead. Additionally, a standardised method was not used to determine whether methadone was required intraoperatively. An objective measure, such as a 10% increase in heart rate and/or blood pressure, could have been used to determine whether rescue analgesia was required. Clinically, this is not how the requirement for additional analgesia is currently made in the hospital, which is why the method was not used. Instead, the anaesthetist was allowed to provide analgesia based on their clinical judgement.
The final limitations were associated with the number of people involved in the study. For ease, the blocks were performed by one of two residents in veterinary anaesthesia and analgesia. This allowed data collection to be carried out continuously as one resident was always present in the clinics. Analysis of the data found that this did not have a significant impact on the effectiveness of the blocks, based on postoperative methadone consumption.
Conclusions
This is the first study directly comparing the lateral and transgluteal approaches to the sciatic nerve block in association with a psoas compartment block. This study found no difference in terms of intraoperative or postoperative analgesia requirement or ease of block performance. Postoperative opioid was required by 17% of dogs, suggesting that for the majority of dogs adequate analgesia is provided by peripheral nerve block and NSAID alone in the postoperative period. Further studies are required to compare other approaches with the sciatic nerve block.
KEY POINTS
- When combined with a psoas compartment block, both the lateral and transgluteal approach to the sciatic nerve block confer similar levels of analgesia both in the intraoperative and postoperative periods.
- Both blocks are suitable for use as part of a multimodal analgesic approach for dogs undergoing stifle surgery.
- When using local analgesic techniques, assessing pain in the postoperative period is essential because some dogs will require additional analgesia.
- In this study, the intraoperative methadone requirement was high (52%), but this was comparable to other studies. Appropriate monitoring during the anaesthetic is essential to ensure adequate intraoperative analgesia.
- The ease of performing the block, in terms of time taken to perform the block and number of attempts through the skin, was similar for the lateral and transgluteal approaches.

