Urolithiasis refers to the identification of urinary calculi which can be located in the upper (nephroliths and ureteroliths) or the lower (cystoliths and urethroliths) urinary tract. The presence of nephroliths must be differentiated from mineralisation of renal parenchyma (nephrocalcinosis). It is currently unknown whether medullary mineralisation in cats is on a continuum with the future development of nephrolithiasis. Urolithiasis is a common clinical presentation, but differences exist in terms of calculi composition not only by location of the stones (upper versus lower) but also based on breed, sex, age and underlying disease conditions. A full evaluation of potential risk factors for the formation of uroliths together with diagnostic investigation to try and establish the likely stone type and burden is important, in order to optimise not only the initial management but also to facilitate prevention strategies to reduce the risk of recurrence.
Feline urolithiasis
Upper urinary tract uroliths
Upper urinary tract uroliths can be considered either obstructive or non-obstructive, and the degree of obstruction may be partial or complete; a differentiation that can be challenging to determine, and can occur at any level (for example, both in the renal pelvis and the ureter). Ureterolithiasis is the most common cause of upper urinary tract obstruction (82%; Berent et al, 2018) with the most common urolith type in the upper urinary tract of cats being calcium oxalate (>98%; Kyles et al, 2005). Other types of urolith are possible, but much less common (for example xanthine, urate, struvite, apatite, blood concretions) (Kyles et al, 2005). One of the difficulties in assessing the composition of uroliths from the upper urinary tract is that it is rare for them to be submitted for analysis, at least partly because management strategies (such as theplacement of subcutaneous ureteral bypass devices) do not require removal. Whilst all upper urinary tract uroliths will originate in the kidney, not all will migrate into the ureter. One study suggests that it is more common to localise ureteroliths to the proximal ureter than either the mid or distal ureter or ureterovesicular junction, and logically larger uroliths are more likely to cause obstruction proximally (Nesser et al, 2018).
The median age of cats affected by upper urinary tract uroliths has been reported to be 7 years but the range is wide (8 months to 16 years), with both male and female cats potentially affected (Kyles et al, 2005). It should be noted that this median age is younger than for those cats presenting with chronic kidney disease due to tubulointerstitial nephritis (Syme et al, 2006). A recent study (Geddes et al, 2023) based on data from a referral centre in the United Kingdom explored the concept that two populations of cats with upper urinary tract urolithiasis exist; a younger subset with a more aggressive phenotype likely to be associated with obstructive disease and an older subset with more benign disease. This study explored 521 cats with confirmed upper urinary tract uroliths, of which two-thirds had been referred for investigation of urolithiasis and/or azotaemia (Geddes et al, 2023). Key risk factors identified in this study for upper urinary tract uroliths included being female, over 4 years of age and being one of the following breeds; Ragdoll, Tonkinese, Persian, British shorthair and Burmese, while the Norwegian Forest cat was at reduced risk compared to nonpurebred cats (Geddes et al, 2023). The age bracket with the highest risk for identifying upper urinary tract calculi was 4–7.9 years (Geddes et al, 2023). Similarly, in a study from a Japanese referral centre exploring the prevalence of upper urinary tract uroliths in cats with chronic kidney disease, the median age was 5.6 years (Hsu et al, 2022). In the study by Geddes et al (2005), comparisons were drawn between cats with obstructive and non-obstructive upper urinary tract uroliths. Where uroliths were obstructive, cats were significantly younger (median age 7 years versus 10 years for non-obstructive uroliths), a greater proportion had evidence of hypercalcaemia (21% versus 11%), they were more likely to be female (61% versus 45%), had a previous diagnosis of chronic kidney disease (62.4% versus 39%) and were more likely to be fed only dry food (63.8% versus 27.5%) (Geddes et al, 2023).
Lower urinary tract uroliths
In contrast to the upper urinary tract, the most common uroliths identified from the lower urinary tract are calcium oxalate and struvite, with less frequent urolith types including urate, apatite, silica and cystine (Cannon et al, 2007; Houston et al, 2016). A recent study exploring 13 years of calculi submissions from the lower urinary tract suggested roughly equal proportions of uroliths are calcium oxalate (46%) compared to struvite (47%), but that overall there had been a significant decrease in calcium oxalate calculi (from 50% to 37%) and a significant increase in struvite calculi between 2005 and 2018 (from 41% to 54%) (Kopecny et al, 2021). Whilst for struvite calculi there was a similar distribution of male and female cats (53% versus 47%), for calcium oxalate calculi there was a predisposition for male cats (64% versus 26%) which is in contrast to the data on upper urinary tract uroliths (Kopecny et al, 2021). A greater proportion of cats with calcium oxalate (66%) in this study were 7–15 years old, whereas for struvite calculi a greater proportion were 4–10 years old (63%), suggesting that overall cats with struvite calculi tend to be slightly younger and calcium oxalate slightly over but with clear overlap possible (Kopecny et al, 2021). Certain types of urolith can have particular breed predispositions; for example Persian, Himalayan, Burmese have been shown to be over-represented for calcium oxalate uroliths and the Egyptian Mau and Ocicat predisposed to urate calculi (Cannon et al, 2007; Appel et al, 2010; Albasan et al, 2012; Houston et al, 2016; Kopecny et al, 2021). Reduced risk associations have been identified for Bengal, Ocicat and Persians for the formation of struvite uroliths when compared to domestic shorthairs (Kopecny et al, 2021).
Clinical presentation
Lower urinary tract uroliths
The clinical presentation of cats with urolithiasis is dependent on the location of the uroliths. Cats with cystoliths will typically present with clinical signs referable to the lower urinary tract (for example stranguria, dysuria, haematuria, pollakiuria, periuria) (Labato, 2017). However, urolithiasis is only the second most common cause of lower urinary tract signs (approximately 20%), while feline interstitial cystitis is considered the most common and other differentials like neoplastic disease and sporadic bacterial cystitis amongst others are possible (Kaul et al, 2020). The duration of clinical signs for cats with cystoliths can be very variable depending on the period of time from onset of signs to presentation for veterinary attention. Additionally, with a low stone burden, cystoliths can be an incidental finding – for example, when a cat is undergoing diagnostic investigations, such as ultrasound or radiographs, for another indication (Labato, 2016). On physical examination, key findings may include a small bladder if there is evidence of pollakiuria, although bladder size may also be normal. The bladder may be painful on palpation and there may be clinical suspicion of a thickened bladder wall due to chronic inflammation. However, physical examination can be unremarkable.
Where calculi become lodged in the urethra, clinical signs become more marked due to the obstruction (Cooper, 2015). Young to middle aged male cats are considered predisposed to urethral obstruction due to the narrow penile urethra, with urethral obstruction being rare in female cats. The presence of a urolith causing obstruction must be differentiated from other causes, like urethral plugs or urethral spasm (Cooper, 2015). In a recent study of 1293 male cats with urethral obstruction identified in first opinion practice, of which 305 had radiographic studies performed, approximately 10% had evidence of calculi but only 29% of these calculi were within the urethra at the time of investigation (Beeston et al, 2022).
Cats with urethral obstruction will typically present acutely (<48 hours) with classic lower urinary tract signs as previously described, but owners may also have noted non-productive straining in the litter tray. With time, secondary metabolic consequences of urinary tract obstruction are likely to manifest, for example progressive lethargy, depression to obtundation, reduced appetite, hypothermia, pale mucous membranes, nausea and vomiting (Bartges, 2017). The onset of these clinical signs typically marks the development of post-renal azotaemia, metabolic acidosis and the reduced capacity to excrete potassium leading to hyperkalaemia (Bartges and Callens, 2015; Cooper, 2015). On physical examination, the bladder is often large, distended and turgid depending on duration of obstruction and may be painful on palpation. There may be evidence of dehydration and where hyperkalaemia has developed, bradycardia may ensue and represents a life-threatening situation requiring prompt medical intervention (Jones et al, 2022). In cats with acute urethral obstruction due to urinary calculi, further probing of the full medical history may reveal more chronic lower urinary tract signs reflecting the previous or concurrent presence of cystoliths, the possibility of other lower urinary tract issues such as feline idiopathic cystitis or both.
Upper urinary tract uroliths
The clinical presentation of cats with upper urinary tract stones can also be very variable. Overall, clinical signs are dependent on whether there is evidence of unilateral or bilateral disease, the presence or absence of pre-existing chronic kidney disease or prior obstructive disease and whether any current obstruction is partial versus complete.
Cats with nephroliths that are non-obstructive may have no apparent clinical signs, or signs that may range from vague lethargy through to episodes of apparent discomfort or owners describing behaviours that are ‘not quite right’. Intermittent haematuria (either micro- or macroscopic) can also be an initial presenting complaint for cats with nephrolithiasis. Similarly, for cats that have initially normal renal function, unilateral partial or complete ureteral obstruction may not be clinically evident or may result in only a period of vague clinical signs that are easily missed (Kyles et al, 2005). Cats that are affected unilaterally with otherwise normal renal function are unlikely to be azotaemic and physical examination findings in these cats may be unremarkable. In a recent study, approximately one-third of cats where upper urinary tract calculi were identified were undergoing investigations for other reasons when the calculi were identified and as such this was an incidental finding and approximately 20% had unremarkable physical examination (Geddes et al, 2023). Previous studies have indicated that reduced appetite (approximately 45%), vomiting (approximately 30–40%), lethargy (approximately 30–35%), weight loss (approximately 22–27%) and polyuria or polydipsia (approximately 16–18%) were the most common clinical signs, with other clinical signs including stranguria and pollakiuria (presumably due to concurrent lower urinary tract disease), haematuria, abdominal discomfort, inappropriate urination, hypersalivation, obtundation and concurrent urethral obstruction also being reported (Kyles et al, 2005; Geddes et al, 2023).
However, complete acute unilateral obstruction due to either a nephrolith or ureterolith can result in the development of hydronephrosis and where this occurs, unilateral renomegaly may be detected, with the contralateral side being normal in size if unaffected by obstructive disease or chronic kidney disease. It is hypothesised that the longer-term consequence of obstruction can be that the affected kidney becomes small, atrophied and fibrotic with reduced contribution to total glomerular filtration rate and reliance on the remaining ‘normal’ kidney which may hypertrophy as a compensatory response (Wu et al, 2021). Therefore, on physical examination where a prior obstructive episode has not been noticed, renal asymmetry can sometimes be identified, with the smaller of the two kidneys being historically obstructed and the contralateral kidney being normal to mildly enlarged due to compensatory hypertrophy (Figure 1).

Nephro- and ureterolithiasis should always be considered to have the potential to be a bilateral disease process. Where there has been previous unilateral obstructive disease but the second initially ‘normal’ kidney subsequently becomes obstructed, renal asymmetry may be exacerbated and these cats will present with severe azotaemia and associated clinical signs (such as lethargy, polyuria polydipsia, hyporexia or anorexia, nausea, vomiting, halitosis) (Wu et al, 2021). Given the dependence of renal function in this scenario on the larger of the two kidneys, rapid intervention (medical management and subcutaneous ureteral bypass placement) is required in order to restore renal function. A similar clinical situation can be encountered in cats with pre-existing chronic kidney disease due to tubulointerstitial nephritis that also have evidence of obstructive nephrolithiasis, ureterolithiasis or both. Data suggest that about 17% of cats that have upper urinary tract calculi will have a previous diagnosis of chronic kidney disease (Geddes et al, 2023). Here, even the development of unilateral partial or complete ureteral obstruction can lead to an acute-on-chronic decline in renal function where the cat will present due to rapid clinical deterioration.
Finally, the development of acute onset bilateral ureteral obstruction, which occurs simultaneously, can lead to cats presenting as clinical emergencies with severe anuric acute kidney injury. In this scenario, cats will be severely azotaemic with associated clinical manifestations, develop severe metabolic acidosis and hyperkalaemia and require emergency management in order to restore urine flow (such as bilateral subcutaneous ureteral bypass device, interim nephrostomy tube placement) and manage the associated metabolic derangements (medical versus dialytic management). Physical examination may indicate bilateral normal to enlarged kidneys with associated renal pain and other attributes typically associated with acute renal failure.
In summary, the potential for upper urinary tract uroliths should always be considered in cats with vague clinical signs and particularly in those where renal asymmetry is identified on physical examination. Given the predisposition for calcium oxalate uroliths, evaluation for upper urinary tract uroliths should also be considered in cats with hypercalcemia. Furthermore, where azotaemia is identified in a cat that is younger than the typical age of presentation for chronic kidney disease due to tubulointerstitial nephritis, this should prompt diagnostic investigations to exclude upper urinary tract uroliths as a contributing cause.
Diagnostic tests
The diagnostic approach and the urgency of investigation of cats with suspected urolithiasis is dependent on their clinical presentation; with obvious requirement for urgency in any cat where obstructive disease is suspected. However, some key diagnostics will be important for most patients.
Evaluation of renal function
Whether dealing with upper or lower urinary tract uroliths, evaluation of renal function will be important and is typically assessed by the use of surrogate markers of glomerular filtration rate (for example urea, creatinine and symmetric dimethylarginine in combination with assessment of urine concentrating ability (urine specific gravity) (Labato, 2016; Bartges, 2017). For cats with cystoliths and no evidence of chronic kidney disease, these parameters are likely to be within reference interval. Similarly, where renal function is initially normal in both kidneys and unilateral obstruction occurs, markers of renal function may remain within reference interval due to their low sensitivity to detect even a 50% decline in renal function. However, where there is pre-existing chronic kidney disease, unilateral obstruction is likely to result in either new-onset or deterioration in azotaemia. Cats with bilateral ureteral obstruction are typically severely azotaemic from the outset and dependent on the duration of obstruction, and cats with urethral obstruction will also develop severe post-renal azotaemia (Kyles et al, 2005; Geddes et al, 2023). Some studies have suggested that symmetric dimethylarginine may be a more sensitive indicator of concern for upper urinary tract stones, although this requires further validation (Hall et al, 2017).
Cats with cystoliths at a young age often have very good urine concentrating ability (urine specific gravity >1.035) and indeed, concentrated urine may indicate an increase in urolith precursors contributing to the risk of development of calculi (Bartges, 2016). However, those cats with pre-existing chronic kidney disease are likely to demonstrate inadequate urine concentrating ability, with urine specific gravity <1.035. For cats with bilateral ureteral obstruction and anuria, it may not be possible to acquire a urine sample depending on the size of bladder at presentation. For all cats with obstructive disease, care should be taken if urine specific gravity is evaluated after de-obstruction, given the potential for a post-obstructive diuresis (Balsa et al, 2019; Muller et al, 2022). Any urine specific gravity interpretation must also take recent fluid administration into consideration.
Additional important laboratory diagnostics
For cats with lower urinary tract calculi, complete blood count may well be normal. For those patients where there has been evidence of marked haematuria, a minimum of packed cell volume, total solids and blood smear evaluation including assessment of thrombocytes is important. Data supports that, approximately 50% of cats presenting with upper urinary tract calculi are anaemic and in some cases, particularly where there may be pre-existing chronic kidney disease, blood transfusions are required (Kyles et al, 2005). Therefore complete blood count is advisable and blood typing may also be required if there is consideration for transfusion.
For those cats that are presenting acutely, an emergency venous blood gas and electrolyte assessment is of paramount importance in order to assess acid-base status and for evaluation of hyperkalaemia helping to facilitate immediate medical management (Jones et al, 2022). However, full serum biochemical profile is often a useful addition in cats with both upper and lower urinary tract calculi as a baseline to evaluate phosphate and ensure there is no evidence of concurrent disease that could be contributory to stone formation – for example, liver function, urate calculi, total hypercalcaemia and calcium oxalate calculi. Whilst total calcium is useful as an initial point of reference, ionised calcium assessment is preferable for those cats where calcium oxalate calculi are identified. Recent data indicates that approximately 11% of cats with upper urinary tract uroliths will show total hypercalcaemia and approximately 17% an ionised hypercalcemia (Geddes et al, 2023).
Together with the urine specific gravity previously mentioned, a full urinalysis is advisable to include pH and sediment evaluation which can be beneficial for review of crystalluria which may indicate potential calculi type. However, it should be remembered that crystalluria is not always present when calculi are identified and that even when identified, they do not always reflect the urolith composition. Compared to dogs, feline struvite uroliths are usually sterile but recognition that stones are struvite in composition is important due to the potential for dietary dissolution (Tefft et al, 2021). Urine culture is a sensible addition, where there is concern for lower urinary tract signs and evidence of bacteriuria on sediment examination or where concern is raised for concurrent pyelonephritis (for example, inflammatory leukogram, pyrexia, bacteriuria and ultrasound evaluation of kidneys).
Diagnostic imaging
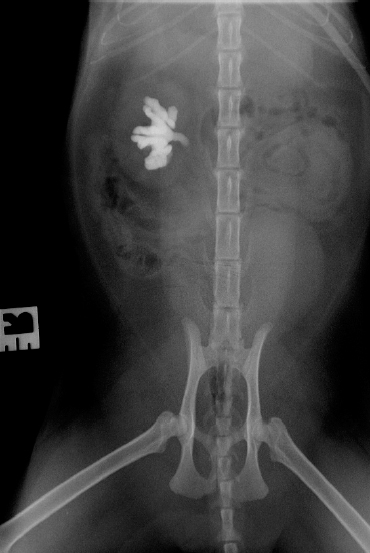
Diagnostic imaging is of great importance in the assessment of any cat with suspected urolithiasis as it provides important information on the location of stones and stone burden. Even if clinical presentation localises to upper versus lower, the entire urinary tract should be evaluated so that the full extent of urolith burden can be ascertained, as this will have potential impact on management and future risk. Radiographic studies may also be useful for characterisation of urolith type on the basis of size, shape and ra-dio-opacity, with the most common urolith types of both the upper and lower urinary tract being radio-opaque (calcium oxalate and struvite) (Kopecny et al, 2021). Plain radiography can therefore be a useful starting point for evaluation of both upper and lower urinary tract uroliths and is obviously a preferred modality when exploring the potential for uroliths causing urethral obstruction (Figure 2; Nesser et al, 2018). Care should be taken to ensure that uroliths are not confused for a feline os penis (Tobón Restrepo et al, 2020). Where radiolucent stones are suspected, positive contrast retrograde urethrocystography can be a useful addition.
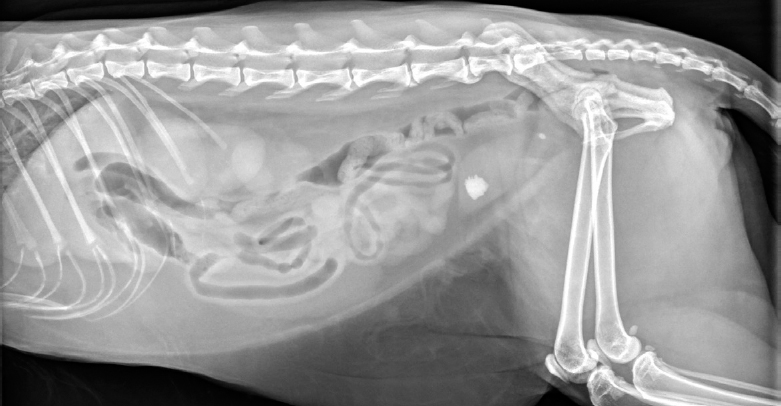
However, ultrasound is also commonly used for evaluation of the urinary tract, providing excellent information on renal size and architecture and allowing evaluation for evidence of renal pelvis dilation (pyelectasia; Figure 3) and identification of ultrasonographic changes that may be consistent with either pre-existing chronic kidney disease or acute kidney injury (Lamb, 1998; Lamb et al, 2018; Wormser et al, 2019). With skill, evaluation of the ureters with ultrasound is possible, particularly if there is evidence of ureteral dilation proximal to an obstructive ureterolith which is commonly identified as a hyperechoic structure with associated distal acoustic shadowing (Figure 4). Ultrasound evaluation of the bladder is useful in the recognition of cystoliths and sediment material, together with providing information on the presence of any concurrent cystitis and associated structural change in the bladder wall.
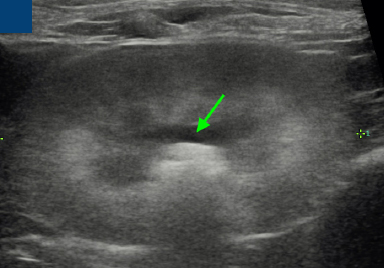

Where ultrasound and radiography have been combined, a 90% sensitivity has been reported for the detection of upper urinary tract uroliths (Kyles et al, 2005). However, determination of whether there is obstructive versus non-obstructive disease is frequently challenging and sometimes cannot be determined on the basis of ultrasound alone. Measurement of renal pelvis dilation can be informative but considerable overlap exists between the degree of pyelectasias that can be encountered with obstructive disease, chronic kidney disease and pyelonephritis (D'Anjou et al, 2011; Quimby et al, 2017). While renal pelvis dilation of greater than approximately 1 cm is highly likely to be associated with obstructive disease, a lesser degree of renal pelvis dilation does not preclude this (Quimby et al, 2017). Studies have suggested that antegrade pyelography, where positive contrast (iohexol) is placed with ultrasound guidance directly into the renal pelvis with serial radiographs or fluoroscopic evaluating movement of contrast down the ureter, can be useful for determining obstructive disease but this procedure is not without the potential for complications (Figure 5) (Adin et al, 2003; Etedali et al, 2019; Lemieux et al, 2021). In addition, it should be recognised that typically supraphysiological pressures are applied during the injection of contrast in this procedure and therefore it may not replicate the normal ureteral flow of urine. Antegrade pyelography is also performed with fluoroscopic guidance at the point of surgical intervention, such as for subcutaneous uretal bypass placement (Clarke, 2018). Another study has explored the utility of non-enhanced computed tomography for the detection of upper urinary tract uroliths and suggest that computed tomography may improve detection of ureteroliths, although is typically more expensive than the traditional combination of ultrasound and plain radiography (Testault et al, 2021). Computed tomography may also have potential utility in the characterisation of urolith composition (Bruwier et al, 2022).
Urolith analysis
It is valuable for any uroliths that are retrieved from the urinary tract to be submitted for urolith analysis in order to be certain about composition. Ideally, this will provide information about the nidus, body and shell of the urolith, particularly if there is concern for a composite urolith. Information on urolith analysis can be used to provide important information for long-term preventative management (Basiri et al, 2012). Where there is concern for concurrent urinary tract infection, submission of uroliths for culture can also be beneficial and should be considered at the time of urolith retrieval.
Conclusions
Ultimately, the combination of clinical signs, physical examination, laboratory evaluation and diagnostic imaging are used to provide a full clinical picture in any cat where there is suspicion for urolithiasis. The importance of ensuring a comprehensive assessment of the full urinary tract in any cat with urolithiasis cannot be over-emphasised. In recent years, there has been an apparent increase in the number of cats being recognised with upper urinary tract uroliths. These represent a complex group of patients both in terms of the requirement for careful historical assessment to try and elucidate the chronology of any obstructive process, together with any pre-existing chronic kidney disease and other contributing risk factors, but also in terms of options for long-term management and risk of acute and severe decompensation when the bilateral disease is present. Lower urinary tract uroliths remain a common presentation in clinical practice and should not be overlooked in cats presenting with lower urinary tract signs.
KEY POINTS
- Urolithiasis is a common presenting urinary condition in cats; the clinical signs and physical examination findings will be dependent on the location of uroliths.
- Clinical signs associated with upper urinary tract uroliths can range from unremarkable through to severe depending on the degree of obstruction, whether the process is unilateral or bilateral and the presence of pre-existing kidney disease.
- Lower urinary tract uroliths characteristically result in clinical signs and physical examination findings reflecting the lower urinary tract, but cystoliths can also be an incidental finding.
- Calcium oxalate uroliths are the most commonly identified urolith in the feline upper urinary tract whilst both calcium oxalate and struvite (sterile) uroliths are identified in the lower urinary tract.
- Diagnostic investigations in cats with urolithiasis should always include an evaluation of renal function but it should be remembered that, where underlying renal function is normal, and unilateral ureteral obstruction occurs, the cat may not demonstrate azotaemia.
- Diagnostic imaging of the urinary tract is crucial to the investigation of urolithiasis in cats and most commonly, the combination of plain radiography and ultrasound examination are performed and considered complimentary. It is vital that evaluation of the entire urinary tract is performed in order to understand the full extent of the urolith burden.


