Orthopaedic patients represent a moderate proportion of first opinion practice caseloads (Belshaw et al, 2020). To reach a diagnosis efficiently, clinicians need to appreciate the importance of obtaining an accurate history, observation of the standing animal, gait analysis, orthopaedic and neurological examination and how their findings influence the selection of appropriate diagnostic tests to confirm the suspected diagnosis. The methodical approach to every orthopaedic patient listed in this article will help clinicians in this process.
History
Taking the patient's history can be one of the most time-consuming and challenging parts of the orthopaedic examination. General questions should be followed by focused questions. The owner should be asked to provide information about signalment, diet, duration of ownership, vaccination status, the function of the patient (for example, working, competition or pet animal), current medications, previous injuries or illnesses, exercise regimen and travel history. Signalment is particularly important, as breed, sex and age can predispose to certain orthopaedic diseases, such as elbow dysplasia (Baers et al, 2019) and hip dysplasia (Lopez and Schachner, 2015). Similarly, a poorly balanced diet has been associated with rickets, hypervitaminosis A and hypervitaminosis D (Bennett, 1976).
The patient's intended use (working dog or a pet) is of high importance as it can influence the differential diagnoses and help to manage future expectations. Understanding the patient's current exercise regime is paramount, as the intensity of exercise or the extent to which the patient has been confined and restricted is relevant to the progression of many orthopaedic conditions. Certain conditions, such as septic arthritis, are more likely to occur in patients suffering from osteoarthritis (Phillips and Bleyaert, 2022), while many conditions, such as cranial cruciate ligament disease, can be bilateral, therefore information regarding previous and current disease status is necessary. Travel history should prompt the clinician to increase the list of differential diagnoses based on the location. Following completion of general questions, more targeted questions should be asked (Table 1).
Table 1. Lameness grading
| Grade | Description |
|---|---|
| 0 | No lameness is detected |
| 1 | Mild lameness is present that is only appreciated in trot |
| 2 | Mild to moderate lameness in present at walk and it deteriorates at trot |
| 3 | Moderate lameness is present in walk and trot |
| 4 | Moderate to severe lameness is present in walk and troot. Intermittent non-weight bearing |
| 5 | Non-weight bearing is present most or all of the time |
Observation
Observation of orthopaedic patients should begin as soon as they enter the consultation room, and can be aided by allowing patients to move freely around the room. Attention should be given to assessing whether the patient exhibits lameness, the symmetry of the patient when standing, and the weight distribution between the limbs. Abnormal positioning of a limb, angular limb deformity, joint hyperflexion or hyperextension, and marked muscle atrophy may be immediately apparent. Patients may offload a single limb, resulting in less ground contact and reduced splaying of the digits of that limb (Arthurs, 2011a). If bilaterally lame, patients may shift all of their weight forwards, resulting in an elongated neck and elbows pointing caudally, or backwards, resulting in a curved thoracolumbar spine and crouched stance. A positive sit test is when the patient sits with an extended stifle, which can indicate stifle pain (Scott, 2018).
Gait analysis
Gait analysis is a crucial part of every orthopaedic examination. Clinicians should be aware that the client's perception of lameness may differ significantly from their own. Assessment should start with 15 metres of slow walking and then trotting on a short lead in a straight line. It should be repeated as many times as needed. Generally, the hindlimbs are assessed when the patient is walking away, and the forelimbs are examined when the patient is walking towards the clinician. Mild lameness may be subtle during walking, but more apparent during trotting.
When assessing the patient's gait, the clinician should assess head nodding, stride length and duration, limb tracking and symmetry. Head nodding is the most indicative of forelimb lameness. It occurs when the patient attempts to reduce the forces being placed on a thoracic limb. The head is elevated when the affected limb is loaded and lowered when the non-affected limb is loaded (down on sound). Affected limbs usually exhibit a shorter stride length and a shorter stance time, resulting in a faster swing of the unaffected limb. Additional signs of pain include stiffness and decreased range of motion in certain joints, such as bunny hopping in patients with coxo-femoral pain (Lopez and Schachner, 2015). Limb tracking describes the position of the limb under the body (Scott, 2018). When the patient is trotting, the fore and hindlimbs should be straight and converge on a centre point under the patient's body (Scott, 2018).
Particular attention should be paid to circumduction of the limbs, symmetry of limb tracking, limbs crossing the centre line, and wide based limbs (Scott, 2018). Last, the patient should be walked in a circle in both directions. This test will increase forces placed on the limbs towards the centre of the circle, exaggerating any lameness. Lameness can be quantified with a grade from 0–5 (Table 2).
Table 2. List of specific orthopaedic questions
| In the owner's opinion, which limb is the patient lame on?Is the animal lame on any other limb?What is the duration of lameness?What is the severity of lameness?Did the lameness start acutely or is it chronic?What is the response to previous medication?Is the onset of lameness associated with trauma?Does the lameness fluctuate in severity?Does the lameness deteriorates following the rest?Does the lameness deteriorate following or during exercise?Is the lameness worse in the morning?Does the lameness deteriorate on the hard or irregular surface?Is there a change in pet activity level? |
Clinicians should be mindful of the potential for neurological lameness. Ataxia typically results in a wide based stance and uncoordinated limb movements, while paresis appears as weakness.
Orthopaedic examination
Orthopaedic examination is considered the most important part of the orthopaedic work up, as it dictates the selection of further diagnostic tests and treatment options (Arthurs, 2011a). Orthopaedic examination can be split into palpation and manipulation. Some clinicians prefer to palpate every limb before manipulation, while some prefer to palpate and manipulate simultaneously as they work through the limbs. Establishing a routine and working in the same direction will reduce the risk of missing parts of the examination. Special attention should be paid to a thorough palpation, especially for joint effusions, as it often provides the first clues to the localisation of the problem. Other palpable abnormalities include atrophy, hypertrophy, heat, swelling, oedema, thickening and hardening of tissues. The clinician should watch for a pain response when palpating both gently and firmly. When manipulating joints, the clinician should be assessing for crepitus, range of motion, instability and pain. If concerns arise, comparison to the contralateral limb is often helpful. The steps of a complete orthopaedic examination are summarised in Table 3 and 4.
Table 3. Summarised tests necessary to perform full orthopaedic examination of the thoracic limb
| Thoracic limb: palpation of shoulder musculature (supra- and infraspinatus) | |
|---|---|
| Pes |
|
| Carpus |
|
| Antebrachium |
|
| Elbow |
|
| Brachium |
|
| Shoulder |
|
| Scapulae |
|
Table 4. Summarised tests necessary to perform full orthopaedic examination of the pelvic limb
| Pelvic limb: palpation of pelvic and femur musculature (gluteal and quadriceps group) | |
|---|---|
| Pes |
|
| Tarsus |
|
| Crus |
|
| Stifle |
|
| Femur |
|
| Hip |
|
| Pelvis |
|
Thoracic limb
The examination of the thoracic limb should start by palpating the shoulder musculature for atrophy or hypertrophy. The scapular spine is a useful landmark to establish the position of the supraspinatus and infraspinatus muscles (Evans and Lahunta, 2013). Owing to the large size of these muscles, they are typically the first muscles to atrophy in chronic forelimb lameness (Arthurs, 2011a). Bilateral simultaneous palpation will help to detect subtle changes. Atrophy of just one of these muscles can indicate focal pathology, such as infraspinatus contracture (Pettit et al, 2008), rather than disuse atrophy of the limb.
Manus
Each joint of each digit is examined systematically to assess for swelling or effusion, flexion, extension and mediolateral stability. Interdigital skin and pads should be assessed for evidence of dermatitis, skin lacerations and foreign bodies. Particular attention should be paid to the pads in sighthound breeds which are prone to corns (Guilliard and Doughty, 2022). Claws and nailbeds should be assessed for normal growth, inflammation, pain and discharge. Clinicians should be aware of the importance of sesamoid bone palpation, especially in Rottweilers which are prone to sesamoid fracture (Read et al, 1992). The metacarpal bones should be assessed individually for evidence of pain, instability, thickening and soft tissue swelling.
Pes
Examination of the pes should be performed in a similar fashion to the manus.
The carpus
Proximally, the carpus consists of the radial carpal and ulnar carpal bones and distally, of the carpal bones I–IV (Evans and Lahunta, 2013). The carpus is a hinge joint with limited soft tissue coverage, so can be readily palpated (Scott, 2018). The majority of motion of the carpus arises from the antebrachiocarpal joint. Synovial effusion can be palpated between the distal radius and the proximal row of the carpal bones as an absence of the depression corresponding to the joint (Evans and de Lahunta, 2013) (Figure 1).

The carpus should be thoroughly palpated and the antebrachiocarpal joint should undergo flexion and extension to establish the carpal range of motion. The physiological antebrachiocarpal range of motion is 196° in extension and 32° in flexion and when fully flexed, the digital pads should contact the caudal surface of the antebrachium (Scott, 2018). Recognition of periarticular swelling should prompt assessment for hyperextension and hyperflexion, and the integrity of the collateral carpal ligaments should be assessed by stressing the carpus laterally and medially in extension.
Pain during direct palpation of the abductor policis longus tendon, in conjunction with joint flexion and swelling of the medial aspect of the carpal joint, may suggest stenosing tenosynovitis of the abductor pollicis longus (Grundmann and Montavon, 2001).
The accessory carpal bone is a truncated rod bone located on the palmar side of the ulnar carpal bone (Evans and Lahunta, 2013). It should be palpated for pain, instability and swelling. Accessory carpal bone fractures are particularly common in racing greyhounds (Johnson, 1987).
Antebrachium
Palpation of the antebrachium should start distally and progress proximally towards the elbow joint. Nearly the entire radius and ulna can be palpated. The extensor muscles of the carpus and digits are palpable on the craniolateral antebrachium and the flexor muscles on the caudomedial antebrachium (Arthurs, 2011a).
Elbow
The elbow joint is a complex hinged joint formed of the distal humerus, proximal radius and ulna (Samoy et al, 2006). The lateral and medial epicondyles and the olecranon are easily palpable (Samoy et al, 2006). Elbow effusion is palpable in a depression between the lateral epicondyle and the olecranon, at the level of the anconeus muscle (Arthurs, 2011a) (Figure 2). The physiological range of motion is 166° in extension and 36° in flexion (Scott, 2018). When fully flexed, the antebrachium contacts the cranial surface of the brachium. Manipulation of the elbow joint should include extension, flexion and flexion with supination of the antebrachium with the carpus flexed to 90°. The latter may identify medial compartment pain (Burton, 2018). Pain elicited on elbow extension may suggest elbow dysplasia or un-united anconeal process (Scott, 2018). Pain elicited by compressing the humeral condyle with simultaneous elbow extension may suggest humeral intercondylar fissure (Moores, 2021). Campbell's test should be performed to assess the competency of the collateral ligaments (Campbell, 1969). With the elbow and carpus at 90°, the elbow is pronated and supinated. In dogs, the average range of motion is 30° and 50° respectively (Scott, 2018).
Branchium
Only the proximal and distal humerus can be appreciated on palpation. The proximal humerus is a predilection site for osteosarcoma in large and giant breed dogs (Morello et al, 2011). Therefore, this region should be palpated specifically and if resentment is identified, this may be indicative of osteosarcoma (Morello et al, 2011). The triceps brachii is a large group of muscles on the caudal aspect of the brachium, inserting on the olecranon. The biceps brachii can be palpated at its insertion on the supraglenoid tubercle, running through the intertubercular groove medially, and inserting on the radial head and ulna.
Shoulder and scapula
The shoulder joint consists of a humeral head articulating within the glenoid cavity of the scapula (Evans and Lahunta, 2013). Palpable bone landmarks are the acromion, greater tubercle, intertubercular groove and scapular spine (Scott, 2018). The biceps brachii, supraspinatus and infraspinatus tendons, and brachial plexus should be palpated. Shoulder manipulation should include flexion, extension, abduction and adduction. Normal range of motion of the shoulder is 165° in extension and 57° in flexion (Scott, 2018). The biceps tendon test involves the flexion of the shoulder with the elbow in extension and with the application of focal pressure of the biceps tendon of origin (Bruce et al, 2000). Pain elicited during this test increases the probability of bicep tendonitis (Bruce et al, 2000). Shoulder abduction angles give an indication of shoulder instability, the patient should be sedated and positioned in lateral recumbency with both scapulae parallel to the table. With the elbow in extension, the brachium should be maximally abducted. The angle between the scapular spine and the lateral aspect of the brachium is measured with a goniometer (Cook et al, 2005). The average angle in normal dogs is approximately 32° (Cook et al, 2005). The cranial drawer test can be performed on a shoulder in a similar manner to the stifle (see later) and has been reported to be a consistent indicator of shoulder instability in dogs (Bardet, 1998).
The scapula should be thoroughly palpated. While relatively uncommon, scapula fractures are easily missed on clinical examination (Perry and Woods, 2017).
Examination of the pelvic limb
Examination of the pelvic limb should start with palpation of musculature. The clinician should assess the size of the quadriceps, hamstrings and gluteal muscles in both pelvic limbs (Evans and Lahunta, 2013). As in the thoracic limb, disuse muscle atrophy is frequently recognised in the proximal musculature, particularly the quadriceps. Simultaneous bilateral palpation will aid detection of subtle changes.
Tarsus
The tarsus is a complex hinge joint consisting of the talus, calcaneus, central tarsal bone, and tarsal bones I-IV. (Evans and Lahunta, 2013). The range of motion of the tarsus in flexion and extension is 38° and 165° respectively (Scott, 2018). The talocrural joint is responsible for approximately 85% of the movement of the tarsus (Scott, 2018). The medial and lateral malleoli, calcaneus and common calcaneal tendon can be easily palpated. Synovial effusion can be palpated in four pouches that are located dorsal and plantar to the medial and lateral malleoli (Arthurs, 2011b) (Figure 3). Palpation of the common calcaneal tendon is best performed during weight bearing (Scott, 2018). Recognition of periarticular swelling of the talocrural, intertarsal or tarsometatarsal joints should prompt thorough interrogation of the ligamentous stability at that level in all directions. Swelling and instability can also indicate fracture.

Manipulation of the talocrural joint should include flexion, extension, and mediolaterally stressing the collateral ligaments with the tarsus in extension and again in flexion. Complete rupture of the common calcaneal tendon will result in plantigrade stance (Harasen, 2006). The gastrocnemius tendon can be disrupted with the preservation of the superficial digital flexor tendon, leading to partial plantigrade stance with the digits flexed (Harasen, 2006). Common calcaneal tendinosis may cause pain and palpable thickening of the Achilles mechanism, but with no alteration in the joint posture (Pettitt et al, 2018). The ability to fully flex the hock, with the stifle maintained in extension, confirms insufficiency of the common calcaneal tendon (Scott, 2018). Luxation of the superficial digital flexor tendon from the calcaneal tuberosity can result in a popping sensation and the tendon will be palpated out of place, usually laterally (Jury, 2021).
Crus
The fibula can be palpated at the lateral malleolus and fibular head. The entire length of the tibia can be palpated medially and cranially. The gastrocnemius can be appreciated caudal to the proximal tibia and its tendon of insertion may be followed within the common calcaneal tendon to its insertion on the tuber calcanei (Scott, 2018).
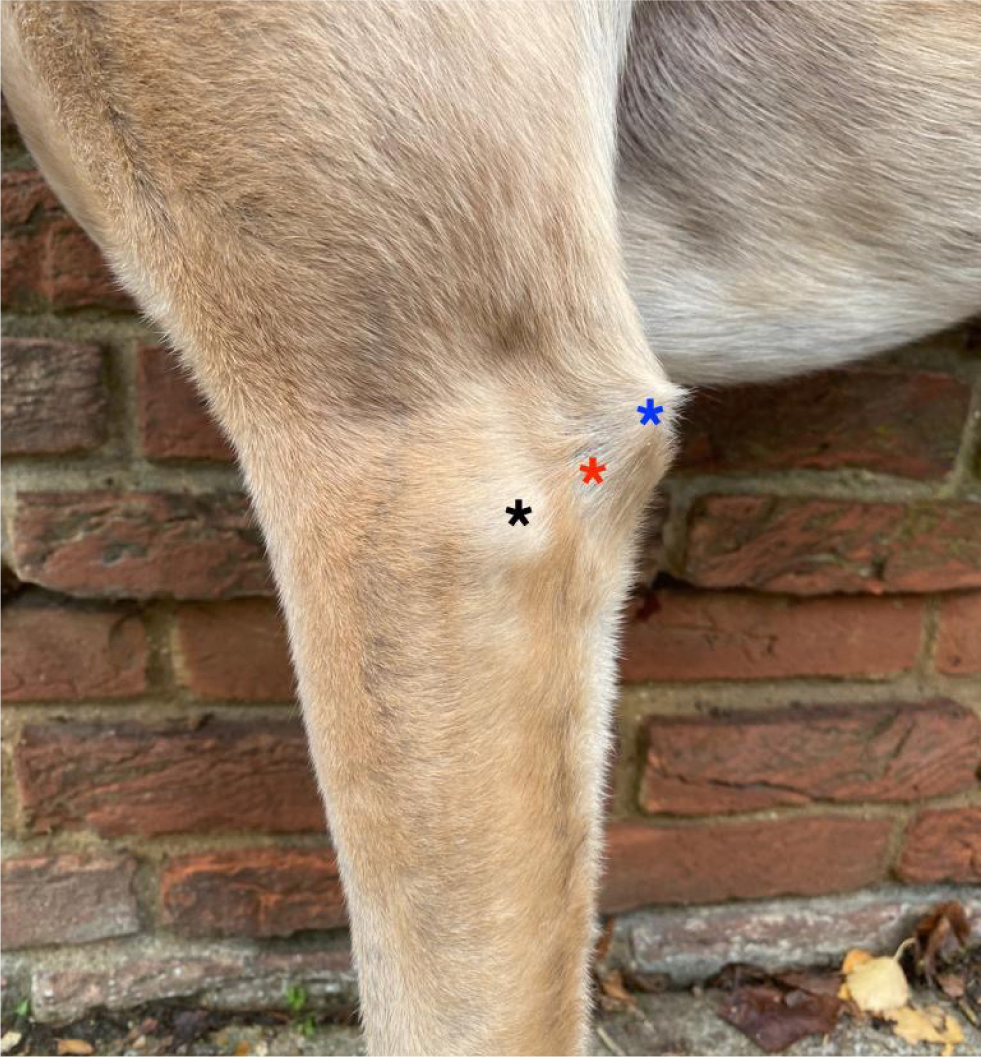
Stifle
The stifle is a complex hinge joint consisting of femorotibial and femoropatella articulation (Farrell, 2018). Palpable landmarks of the stifle joint are the patella, patella tendon, tibial tuberosity and femoral condyles. The fibular head is palpable as a bony structure located at the lateral aspect of the stifle joint. Proximally, the sesamoid of the gastrocnemius muscle may be appreciated. The stifle range of motion is 41° and 162° in flexion and extension respectively (Scott, 2018). The stifle joint is appreciated as a concave de-pression located on the medial and lateral aspect of the straight patella tendon (Evans and Lahunta, 2013). Stifle effusion presents as loss of the concave depression on either aspect of the patella tendon with indistinct margins of the tendon (Arthurs, 2011b) (Figure 4). Simultaneous bilateral palpation is helpful for appreciating stifle effusion. Presence of stifle effusion is highly suggestive of cranial cruciate ligament rupture (Gatineau et al, 2011).
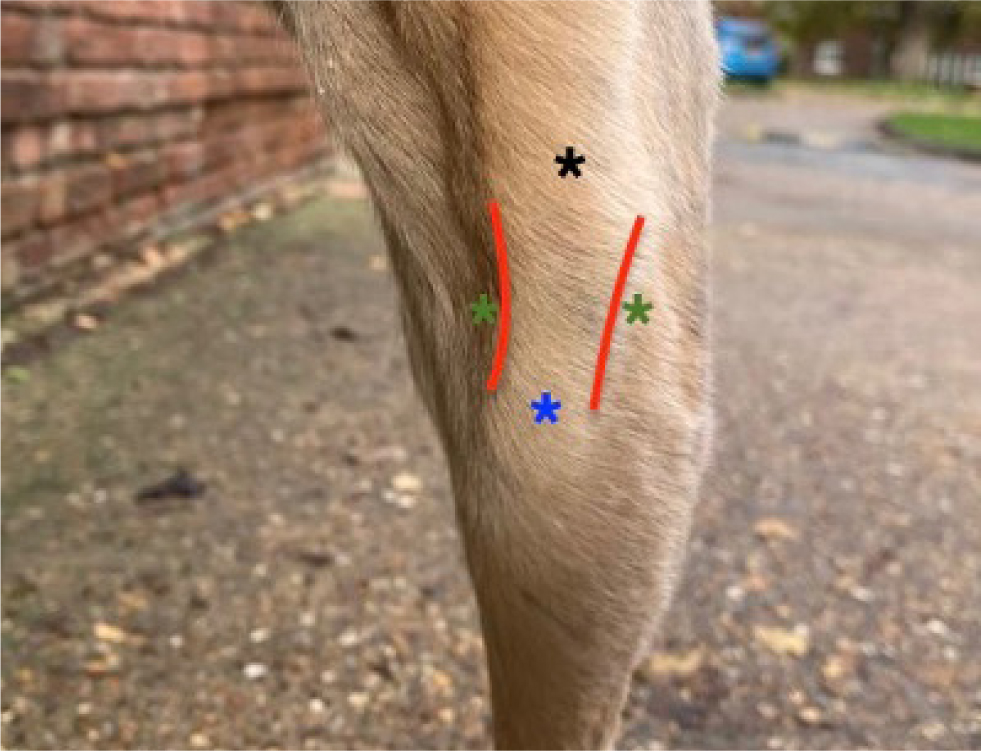
Clinicians should assess the patella tracking, first by flexing and extending the stifle while feeling for luxation, and then by applying lateral and medial force to the patella with the stifle in flexion and extension (Perry and Déjardin, 2021). Examination of the integrity of the cranial cruciate ligament is essential. Positive cranial drawer and tibial compression tests are pathognomonic for cranial cruciate disease (Taylor-Brown et al, 2015). Cranial drawer is performed by firmly gripping the femur with one hand with the index finger on the patella, and the tibia with the other hand with the index finger on the tibial tuberosity. With the femur and tibia grasped in this way, it is possible to assess the extent of cranio-caudal instability within the femoro-tibial joint by moving the two bones relative to one another. Tibial thrust is assessed by maintaining the position of the stifle with one hand with the index finger on the tibial tuberosity and flexing the hock with the other hand. A cranial shift of the tibia is a positive result for both tests. Both should be performed at multiple stifle angles.
The clinician should be aware of the increased degree of craniocaudal stifle laxity in normal young dogs (Scott, 2018). Meniscal tear is a common finding in dogs with cranial cruciate disease (Gleason et al, 2019). Clicking associated with stifle flexion and extension has been reported as specific, but not sensitive for meniscal pathology (Hadley et al, 2019). Medial buttress refers to palpable fibrotic tissue at the proximal medial tibia, and is a common finding in patients with chronic cranial cruciate ligament disease (Farell, 2018). The integrity of the caudal cruciate ligament can be assessed by performing caudal drawer (Scott, 2018). Finally, stifle collateral ligament integrity should be examined with the stifle in extension by applying lateral and medial force to the distal femur and proximal tibia (Arthurs, 2011b).
Femur
The greater trochanter and the femoral condyles are palpable. The quadriceps group cranial to the femur and the biceps femoris caudal to the femur are easily identifiable (Arthurs, 2011b). The adductor, gracilis and pectineus muscles are medial to the femur (Scott, 2018).
Hip
The hip joint is a ball-and-socket construct joint that enables a great range of movement (Evans and Lahunta, 2013). Coxofemoral joint flexion and extension are 50° and 162° respectively (Scott, 2018). The hip should be flexed, extended, abducted and adducted. Ortolani and Barden tests should be performed in patients with suspected hip dysplasia. For both tests, the patient is sedated and placed in lateral recumbency with the affected limb uppermost. The Ortolani test is performed by placing one hand on the stifle flexed at 90° while the other hand is placed on the dorsum. Proximally directed axial force is applied along the femur which causes subluxation of a dysplastic hip. While the axial force is maintained, the limb is abducted leading to a ‘clunk’ as the femoral head reduces. The subluxation is typically not appreciated, but if the reduction is felt this is a positive test (Gemmill and Oxley, 2018). To perform Barden's test, place one hand over the greater trochanter, and the second hand is used to grasp the femur and lift it laterally. Femoral head displacement greater than 0.5cm is considered as positive for hip laxity (Gemmill and Oxley, 2018).
Iliopsoas muscle strain is a common injury among working and sporting dogs (Cullen et al, 2017). Iliopsoas tendinopathy should be suspected when pain is elicited on hip extension, internal rotation or abduction of the hip, or on direct palpation of the muscle as it passes along the cranioventral aspect of the ilium and inserts on the lesser trochanter (Cullen et al, 2017).
Pelvis
The pelvis should be palpated for symmetry, stability, evidence of pain and muscle mass atrophy or hypertrophy. Landmarks that can be easily appreciated include the ischiatic tuberosity and cranial dorsal iliac spine (Arthurs, 2011b). The triangle formed by these landmarks and the greater trochanter of the femur is an important finding during orthopaedic examination, as if the patient suffers cranio-dorsal hip luxation the greater trochanter will be displaced proximally, leading to loss of the triangular shape (Gemmill and Oxley, 2018).
Neurological examination
Neurological examination of the orthopaedic patient should start with examination of postural reactions in all four limbs. Conscious proprioception can be assessed by flipping the foot and observing the amount of time that it takes the patient to right its position. In healthy dogs, the paw replacement reaction is immediate (Kerwin and Taylor, 2021). Hopping tests will also assess conscious proprioception and are performed by lifting one limb at a time, supporting the patient, and carefully pushing them away from the lifted limb. Withdrawal reflex can be assessed by pinching the interdigital skin of the digits. Withdrawal is an unconscious spinal cord reflex and the correct physiological response is withdrawal of the whole limb. As a very rough rule, an intact withdrawal reflex indicates flexor tone, while extensor tone can be confirmed by the patient's ability to stand. The patient's spine should be palpated, starting from the sacrum and gradually progressing to the neck. The neck should be manipulated into flexion, extension, lateral and medial direction. The tail test is performed by elevating the tail and pushing it cranially. A pain response is suggestive of lumbosacral disease (Arthurs, 2011a). Identification of abnormalities should prompt the completion of a more thorough neurological examination.
Diagnostic imaging
Choice of further investigations should be guided by orthopaedic examination findings. The presence of pain, swelling, effusion, deformity or ligamentous instability typically warrants radiography of that area. Chemical restraint should be utilised and radiographs must be positioned appropriately. Orthogonal views must always be obtained. When obtaining radiographs, the clinician should take advantage of an opportunity to repeat the examination on a sedated patient, where findings may become more obvious. When ligamentous instability is suspected, stressed radiographs are easily obtained. The region is simply stressed with ropes or tape in the direction of instability and then radiographed. Comparison to the contralateral limb is often useful. The presence of unexplained periarticular swelling or effusion warrants a thorough manual interrogation of the stability of the joint in all directions, followed by stressed radiographs. Where soft tissue pathology is suspected, such as shoulder tendinopathy, ultrasound by an experienced practitioner or occasionally magnetic resonance imaging are indicated. Computed tomography is most useful for identifying bone or joint pathology where radiographs are insufficient, for example in cases of elbow dysplasia. Magnetic resonance imaging and computed tomography should never be utilised without first considering the differential diagnoses based on examination findings along with the merits of each modality. It is the author's experience that embarking on diagnostic imaging in the absence of orthopaedic examination findings is challenging and frequently unrewarding.
Conclusions
Although orthopaedic patients can be challenging, a methodical approach will help practitioners to efficiently reach the correct diagnosis and avoid common mistakes. The importance of thoroughly palpating the patient must be stressed.
KEY POINTS
- The approach to orthopaedic patients should be divided into obtaining a history, observation, gait analysis, and orthopaedic and neurological examination, followed by selection of appropriate diagnostic tests.
- Following gait analysis, the patient's lameness can be scored from 0–5.
- Synovial effusions can be palpated on the dorsal aspect of the antebrachiocarpal joint, caudo-lateral aspect of the elbow, adjacent to the malleoli on the tarsus, and adjacent to the patella tendon on the stifle.
- Shoulder joint examination involves palpation of the shoulder musculature, flexion, extension, abduction and adduction of the shoulder joint, biceps test, cranial drawer and abduction angle measurements.
- A brief neurological examination is a crucial part of every orthopaedic examination. It involves the evaluation of conscious proprioception and withdrawal reflexes in all four limbs, spinal palpation and neck manipulation.


