Postoperative wound complications can take many different forms and range from mild inflammatory symptoms to severe disruption of the surgical incision site, where the normal healing process is affected and can lead to partial or complete wound dehiscence.
Surgical wound dehiscence (SWD) is defined as the partial or complete separation of the wound edges at the surgical incision site. This disruption of the healing process can occur due to various factors, including technical, mechanical, and patient-related issues.
Knowing how common SWD is can be challenging, as even on the human healthcare side, the reporting systems tend to be split into individual surgery categories and their complication rates. When surgical site infections (SSIs) are considered, these can contribute to SWD rates and may be reported through a separate system (Sandy-Hodgetts et al, 2023). Registered veterinary nurses (RVNs) can play a vital role in assessing, reporting and treating SWD and contributing to prevention methods.
As with most severe postoperative wound complications, SWD can negatively impact animal welfare and quality of life, the procedure cost, the client's impression of the veterinary establishment and the veterinary professionals' mental health involved in the case.
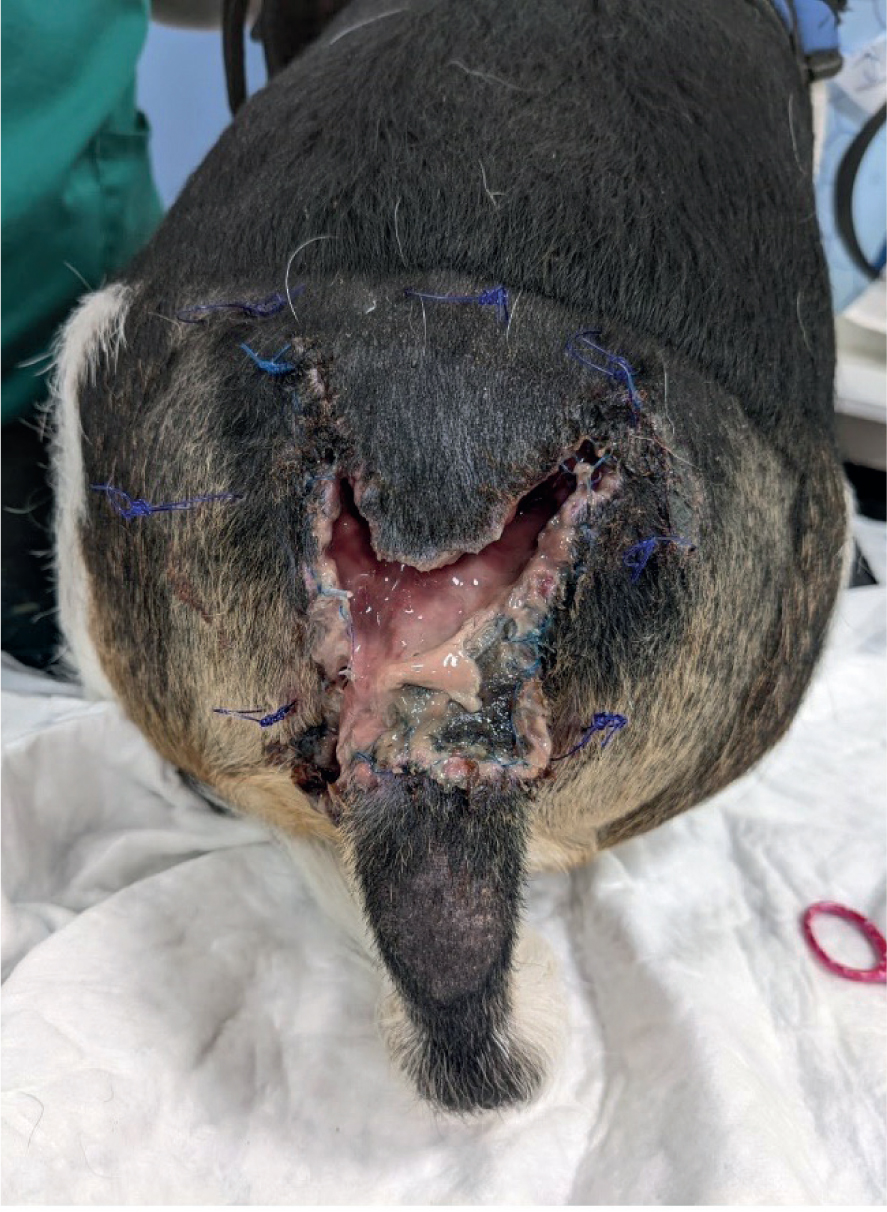
Treatment interventions will vary depending on the extent of the surgical incision site dehiscence; partial (Figure 1) or complete opening (Figure 2) of the surgical wound (Sandy-Hodgetts et al, 2023) can be seen. Once the surgical wound has dehisced, the treatment regimen implemented will follow typical wound management interventions: hair removal, debridement of non-viable tissue, wound cleansing using an appropriate solution and balancing moisture levels using a suitable dressing and fixation method. If an infectious process is suspected, primary closure should be avoided, as this can contribute to further delayed healing and an increased risk of repeated SWD (Wounds UK, 2020).

Causes of surgical wound dehiscence
To identify early if a surgical wound is at risk of postoperative complications, RVNs need to be aware of risk factors that can increase complication rates for the patient before any surgery is performed. Performing a risk assessment for each patient and their potential for postoperative wound complications could help mitigate some contributing factors to SWD.
The cause behind SWD is complicated and multifactorial. It is believed that technical, mechanical, patient-related and other factors that can contribute to delays in wound healing all play a role in the breakdown of surgical wounds. This article will discuss some of the common factors linked to SWD.
Technical stress
This relates to issues with the surgical closure method directly. When a surgical incision is created, the aim is to appose those skin edges to facilitate the wound-healing process postoperatively (World Union of Wound Healing Societies (WUWHS), 2018).
The apposition of the skin edges and the potential for increased tension can be affected by anatomical location, tissue availability, obesity, surgeon experience/preference with the closure method of choice and the materials used for closure. If one or more of these factors are an issue at closure, and the incision is under high tension, the wound-healing process can become disrupted and may fail to close (WUWHS, 2018).
Technical stress can disrupt the healing process by placing excessive tension on the wound edges, impairing blood supply and increasing the risk of infection. These factors contribute to dehiscence by compromising the integrity of the wound closure and delaying the healing process.
Mechanical stress
Mechanical stress disrupts the healing process by causing physical strain on the wound, leading to inflammation, impaired blood flow and tissue damage. These factors contribute to dehiscence by weakening the wound's ability to withstand tension and increasing the risk of infection.
Mechanical stress can also take the form of tension placed onto the incision site. In open traumatic wounds where there is a substantial tissue deficit, if these traumatic wounds are closed on presentation using simple apposition of the skin edges, with no consideration of tension and potential for increases in non-viable tissue or swelling, these patients may be at higher risk for SWD (WUWHS, 2018; Wound UK, 2020).
Other non-infectious processes can put surgical incisions at risk of mechanical stress, such as seromas or haematomas, which contribute to increasing tension from below the incision site (WUWHS, 2018).
An increased risk of SWD can be linked to rising intra-abdominal and intra-thoracic pressure if the animal vomits, retches or coughs postoperatively. Specific patient-related factors and poor client concordance with postoperative instructions can contribute to mechanical stress-related SWD, increasing exercise too soon following the surgery (WUWHS, 2018).
Disrupted healing
External forces that can disrupt the healing process include trauma, pressure and excessive movement. These forces can cause physical damage to the wound, disrupt the formation of new tissue and increase the risk of infection, ultimately leading to dehiscence.
During the normal surgical wound-healing process, the incision would show signs of re-epithelialisation as early as 1 to 3 days post-surgery, depending on the type and extent of surgery, but at this stage, the wound is still not protected from external forces (Wound UK, 2020).
Disruption of the normal phases of wound healing can be linked to multiple factors, including patient body condition score, infectious processes, ischaemia moisture levels, pre-existing conditions, age and medications (WUWHS, 2018). Therefore, a thorough preoperative assessment is vital in preventing SWD and postoperative wound complications, as some factors are more manageable than others, but pet owner expectations and potential for complications can be discussed following a full assessment.
Infection
Whether trying to prevent or treat SWD, a full assessment is required to explore the potential cause or risk factors that may contribute to the breakdown of the normal wound healing process. Although there are links between SSI and SWD, not every SWD is linked with infection, and not all SSIs will cause dehiscence (WUWHS, 2018).
To determine if an SSI is present, best practice dictates that clinical judgment should be used to identify the signs and symptoms of wound infection (Table 1) and can be paired with microbiological testing via swabbing, but the evidence for how useful a wound swab is at determining wound infection is insufficient (Sandy-Hodgetts et al, 2023).
| Localised signs of infection | Two or more of the following may be present: |
|
| Systemic signs of infection | Two or more of the following may be present: |
|
(Sandy-Hodgetts et al, 2024 & Wound UK, 2020)
If microbiological swabbing is indicated, the Levine method should be adopted, and the wound should always be debrided and cleansed using a sterile isotonic solution before collecting the sample (Hughes, 2021).
Debridement and cleansing of the wound before sample collection are essential to remove surface contaminants and debris, ensuring that the collected sample accurately reflects the microorganisms involved in the infection.
Identification of SWD
There is no pre-determined timeline when SWD can occur postoperatively, but signs are typically seen 4–20 days after surgery (WUWHS, 2018). This is important to note as postoperative wound checks in veterinary medicineare typically performed in on days 3–4, so unless early SWD is occurring veterinarians may be relying on pet owners to monitor and report signs of SWD back to surgery. This has the potential to increase the risk of infection if the owner has not been adequately educated or there are barriers to communication between them and the veterinary practice as they may delay seeking advice or reporting the complication until too late.
As with SSI, early identification of disruption of the healing process may help to mitigate SWD, but some do occur without any warning (WUWHS, 2018). Monitoring closely for signs of prolonged inflammation, classed as wound inflammatory signs that extend past days 5, 7 and 10 post-surgery, these signs may also be more exaggerated than expected (WUWHS, 2018). An increase in moisture being produced at the incision site can also be a warning of SWD; infectious fluid would be expected to have a malodour and purulent appearance, whereas serosanguinous fluid may indicate other causes for the potential impeding SWD (WUWHS, 2018).
A normally healing wound should exhibit progressive signs of re-epitheliasation minimal inflammation and serosanguinous exudate. The wound edges should be well-apposed and show no signs of tension or dehiscence.
The TIME framework (Table 2) can be applied to aid in assessing whether there is a disruption to the healing process; this considers the five key clinical areas that relate to wound healing: tissue, inflammation/infection, moisture and edge of wound (WUWHS, 2018).
| Early signs of impaired healing (days 1—4) | Late signs of impaired healing (days 5—15) | |||
|---|---|---|---|---|
| Tissue |
|
|
|
|
| Inflammation/infection |
|
|
|
|
| Moisture |
|
|
|
|
| Edge of wound |
|
|
|
|
(Wounds UK, 2020; Sandy-Hodgetts et al, 2024)
Prevention considerations
In humans, prevention and risk prediction for developing SWD is novel and still an emerging practice. As a result of the lack of defined reporting systems and the multifactorial causes of SWD, it is difficult to correlate a ‘one system fits all’, as different forms of surgery will also have unique challenges (Sandy-Hodgetts et al, 2023).
The early identification and prevention of SWD can be implemented throughout the perioperative journey, being able to highlight during the preoperative assessment process if a patient will be at higher risk postoperatively can help. American Society of Anesthesiologists anaesthetic grading can be paried alongside other known risk factors for postoperative wound complications to create an overall risk number for postoperative complications (Wounds UK, 2020; Sandy-Hodgetts et al, 2023).
This can be performed by a competent RVN in a preoperative assessment appointment. These appointments can be offered to all patients booked for surgery; ideally, they would take place before surgery so a full risk assessment can be performed and any interventions required can be put in place before the day of surgery.
Major perioperative risk factors
Body condition score
Obese or malnourished patients are potentially at higher risk for SWD. The veterinary team should be proactive about underweight or malnourished patients and ensure interventions are implemented to prevent the loss of vital nutrients and additional strain on healing because of a lack of nutritional resources (Wounds UK, 2020; Sandy-Hodgetts et al, 2023
Surgery type and duration
Certain surgery types are linked with an increased risk of postoperative complications (abdominal surgeries, amputations, emergency procedures); this should be accounted for when risk assessing to ensure care is taken during the postoperative period to increase monitoring interventions. Certain types of surgery are associated with a higher risk of postoperative complications. In veterinary medicine, surgical wound dehiscence (SWD) is a relatively under-researched area, with a primary focus on surgical site infections (SSIs). Research on SSI complications indicates that certain soft tissue surgeries and cutaneous skin wounds are more susceptible to SWD.
A prospective cohort study conducted in 2019 examined various soft tissue surgeries performed on 184 dogs between 2013 and 2014. The study found that 8.7% of the patients developed an SSI. The surgeries with the highest incidence of severe SSIs, which also have an increased potential for SWD, included procedures involving the abdomen, peritoneal area, and dermatological surgeries (Espinel-Rupérez et al, 2019).
The duration of surgery has been linked to an increased risk of SSI development and SWD; the longer the surgery time, particularly for surgery where body cavities are exposed, the higher the risk of aerosolised microbial contamination of that cavity.
Hypothermia
Hypothermia that occurs throughout the perioperative period can lead to complications postoperatively. Hypothermia begins to affect wound healing at temperatures below 36°C. Hypothermia leads to a reduction in the body's normal homeostatic mechanisms and has been shown to prolong anaesthetic recovery, by causing vasoconstriction leading to a reduction in blood supply to the incision site affecting wound healing (Wounds UK, 2020). Actions aimed at maintaining normothermia should be initiated from pre-medication administration; patient shivering should also not be ignored and again mitigated where possible; shivering causes an increase in muscle activity which increases oxygen consumption, up to five-fold, this can lead to negative effects in the patient such as hypoxemia, lactic acidosis and hypercarbia (Crossley, 1995)
Age and pre-existing conditions
Age may not directly affect SWD, but geriatric animals tend to have the potential for co-morbidities, such as diabetes, anaemia cardiovascular or pulmonary disease etc, that may affect their healing ability or immune response. Age and co-morbidities may not be manageable, but clear communication, guided by the veterinary surgeon, is essential for controlling the animal's current disease and medication regimen.
Environmental factors
The environment in which the animal is housed postoperatively may influence postoperative wound healing, including second- and third-hand smoke [AQ: any others? Provide referencing]. Third-hand smoking refers to the residue left on surfaces within the home environment. As animals spend much time in contact with floors and lower-down surfaces, they are more likely to sleep and rest in these areas, increasing the potential for contamination and contact with carcinogens and other harmful chemicals that have settled on surfaces (Centre for Tobacco and the Environment, 2024). The RVN's role is to facilitate communication with the pet owner and ensure education is provided on environmental risk factors that could contribute to healing delays or problems postoperatively.
Nursing care
Prevention of SWD is under-researched in veterinary medicine, and in some cases, even if prevention methods are adhered to, some surgical wounds will still occur. The RVN's role in the prevention of SWD involves educating the pet owner on minimising movement and avoiding excess strain or pressure on the wound. This could involve recommendations around patient exercise restrictions, types of bedding to minimise pressure and use of patient enrichment to aid with mental stimulation. In contrast, physical exercise may not be possible.
RVNs can support pet owners in the use of intervention methods to help prevent post-operative complications. The use of Elizabethan collars has been linked with reduced surgical site infections (SSIs) in veterinary medicine by preventing interference with the surgical wound (Espinel-Rupérez et al, 2019). There are a variety of intervention aids available, including Elizabethan collars and pet shirts. Determining the most suitable method requires an open discussion with the pet owner to assess the home environment and identify which aid will suit the animal and ensure adequate coverage of the surgical incision site.
The creation of a collaborative relationship with pet owners can be beneficial for gaining concordance, especially in cases where an Elizabethan collar or pet shirt is used. These aids are usually introduced only when a patient is discharged following surgery, and the patient may find it distressing to wear one, especially if they have not worn one before. This can potentially cause the owner stress, reduce compliance, and increase the risk of surgical wound dehiscence (SWD) (Curtis, 2024).
It may be beneficial to introduce animals to the selected intervention aid a few weeks before surgery. Discussing this with the pet owner can help them gradually acclimate the animal to the aid, thereby improving compliance after the surgery (Curtis, 2024). Additionally, pain management in the postoperative period is crucial. If the patient is interfering with their wound or showing signs of pain, an appropriate multimodal analgesic plan should be discussed with the overseeing veterinary surgeon.
Post-operative wound dressings can enhance the effectiveness of intervention aids and may be more suitable for certain species, such as exotics, where conventional aids are not as easily applied. The World Health Organization's guidelines for the prevention of SSIs recommend that a post-operative wound dressing is applied aseptically following surgery. When clinically indicated, this dressing should remain in place for up to 72 hours (Wounds UK, 2020).
Several factors determine the type of post-operative dressing used. For low-risk patients, a basic interactive dressing may suffice, but in certain cases, a more advanced dressing may be necessary. These advanced dressings can offer additional moisture management or possess antimicrobial properties (Wounds UK, 2020). An ideal interactive post-operative wound dressing should:
The dressing should provide flexibility without hindering the patient's movement, adhere to the skin in a skin-friendly manner, manage exudate or draining fluid, and be waterproof to prevent external contamination.
The duration for which a post-operative dressing remains in place depends on the surgical procedure and the clinical judgment of the supervising veterinary surgeon. Typically, the surgical incision will be evaluated about 2 to 4 days after the surgery. The decision to apply an additional dressing at this time should be based on the patient's risk factors and the condition of the wound.
If SWD has occurred, the management of this now open wound will involve standard strategies applicable to any open wound. This includes debridement, wound cleansing, and the use of appropriate dressings based on moisture levels. Additionally, it is important to secure the chosen dressings and to protect the surrounding peri-wound skin (Sandy-Hodgetts et al, 2023).
These wounds are typically at a higher risk for infection, so it is essential to follow good hand hygiene protocols while handling these patients. Also, monitor for signs of systemic infection, such as fever, lethargy, loss of appetite, redness around the wound, purulent discharge and pain (Sandy-Hodgetts et al, 2023).
Conclusions
Surgical wound dehiscence is an underreported and under-researched area of veterinary medicine. There are many other factors to consider when looking at the management and preventative measures required for these postoperative wound complications. Ideally, wider national reporting systems for submission by veterinary practices would aid in seeing trends in different surgeries and the causes behind surgical wound breakdown. RVNs can support can support the entire perioperative period to mitigate factors that may contribute to SWD and its negative impacts. This can take the form of preoperative patient assessments to create a risk factor grade and in the postoperative monitoring period. RVNs must also educate pet owners on the signs and symptoms they need to consider when the animal is at home and ensure they know when to ask for assistance between postoperative checks. RVNs also need to take charge of their personal knowledge of the signs and symptoms of different postoperative wound complications, as early identification relies on clinical judgment and intervention early on to mitigate the costly breakdown of a full or partial surgical incision site.


