Cranial cruciate ligament disease is one of the most common causes of hindlimb lameness in dogs (Harasen, 2003; 2008; Roush, 2013; Dyall and Schmökel, 2017; Kowaleski et al, 2018). The condition is described as a degenerative and progressive weakening of the ligament, and the pathology behind the degeneration is not yet fully understood (Kowaleski et al, 2018). Several risk factors have been described in the development of cranial cruciate ligament disease, including breed predisposition, obesity and gender/neutering status, with neutered females of large breeds being over-represented (Vasseur et al, 1985). Studies have also found a correlation between a high tibial plateau angle and the development of cranial cruciate ligament disease (Macias et al, 2002; Cosenza et al, 2015). However, studies by Witte (2015) and Vedrine et al (2013) did not show such a correlation, signifying the unlikeliness of a high tibial plateau angle as the sole causative factor for cranial cruciate ligament rupture in small-breed dogs.
Evaluations of the biomechanical properties of intact cranial cruciate preparations have shown a decrease in physical properties, such as elasticity, maximum stress and strain energy, the ligament can withstand with age. Dogs with a body weight of over 15 kg showed these changes earlier in life compared to dog weighing less than 15 kg (Vasseur et al, 1985). The degenerative changes in the stifle joint develop at a slower rate and are less severe in small breed dogs, hence the age of presentation is usually middle age to older in these dogs (Whitehair et al, 1993; Harasen, 2008; Dyall and Schmökel, 2017).
Treatment options for cranial cruciate ligament insufficiency include conservative management, extracapsular stabilisation, cranial closing wedge ostectomy, triple tibial osteotomy, tibial plateau levelling osteotomy, centre of rotation of angulation-based levelling osteotomy, tibial tuberosity advancement and, if concurrent with severe osteoarthritis, total knee replacement (Bruce et al, 2007; Liska and Doyle, 2009; Kowaleski et al, 2018; Brioschi and Arthurs, 2021; Coskun and Viskjer, 2023).
While osteotomy procedures are common in large breeds of dog, conservative treatment and lateral fabellar suture for cranial cruciate ligament insufficiency in small breeds of dog has previously been the most common treatment; this is still the case according to some reports (Comerford et al, 2013; Duerr et al, 2014; Ferreira et al, 2019). Conservative management is likely to result in a prolonged average recovery time of approximately 4 months (Vasseur et al, 1985; Brioschi and Arthurs, 2021). This article will focus on the tibial tuberosity advancement as treatment for cranial cruciate ligament disease.
Tibial tuberosity advancement
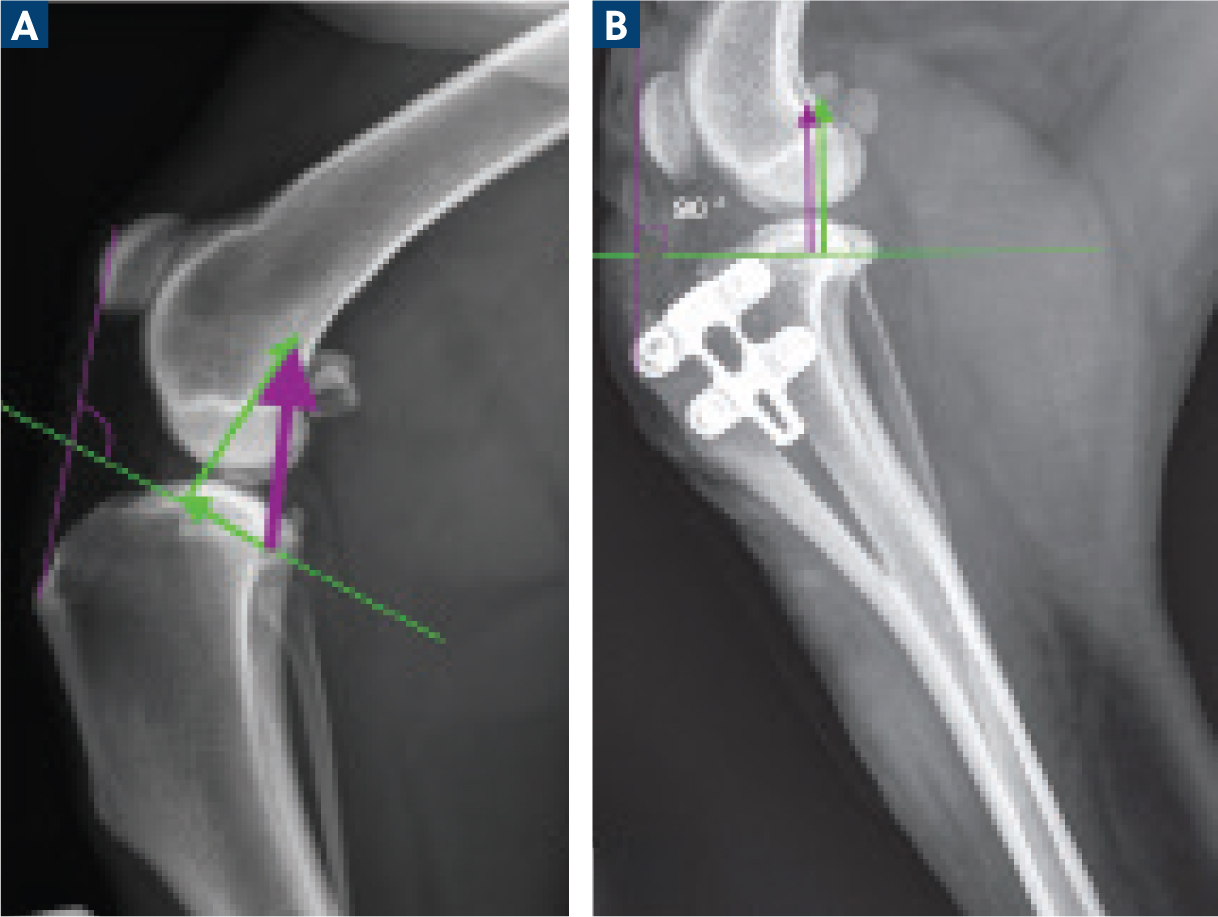
Tibial tuberosity advancement was developed and introduced by Montavon et al (2002). The concept behind the technique is to stabilise the joint during weight-bearing by neutralising the cranial tibial thrust, which is the force generated in the stifle during weight-bearing. In the Tepic biomechanical model of the stifle joint, the joint reaction force is approximately parallel to the patellar ligament. This force can be divided into shear forces; a cranially-directed force (resulting in cranial tibial thrust) and a joint compression force (Tepic et al, 2002). The tibial tuberosity advancement procedure aims to neutralise the cranially-directed shear force by performing a frontal plane osteotomy followed by cranial advancement of the tibial tuberosity to achieve a patellar tendon angle of 90° to the tibial plateau angle during weight-bearing (Figure 1). By doing so, one obtains a neutrally-or caudally-directed tibiofemoral shear force during ambulation which stabilises the joint (Montavon et al, 2002; Tepic et al, 2002; 2004; Apelt et al, 2007).
The tibial tuberosity advancement is fixed in position with a custom-designed tension band, plate and cage, or a tibial tuberosity advancement cage alone. Since the original tibial tuberosity advancement was described (using a cage and a separate plate), a number of different implants have been developed. These include the modified Maquet technique, tibial tuberosity advancement rapid, modified Maquet procedure, modified Maquet tibial tuberosity advancement, tibial tuberosity advancement with cranial fixation and porous tibial tuberosity advancement (Retallack and Daye, 2018; Zhalniarovich et al, 2018; Bernardi-Villavicencia et al, 2020; Aragosa et al, 2022).
One advantage of the tibial tuberosity advancement procedure is that it can be combined with a medial or lateral tibial tuberosity transposition in cases of concurrent patella luxation and cranial cruciate ligament disease, which is a common finding in small dogs. This is achieved by adding a washer of appropriate size along with the tibial tuberosity advancement implant, resulting in both a cranial advancement and lateral (or medial) transposition of the tibial crest (Rita Leibinger Medical; Germany) (Jerram and Walker, 2003).
Early outcomes and complications
Several published clinical studies reflect early experiences with this technique. Among them, the major complication rate has been estimated to be 2.3–26.1% with a reoperation rate of 9.8% (Lafaver et al, 2007; Stein and Schmoekel, 2008; Kemper et al, 2011; Kowaleski et al, 2018). Late meniscal injury was a commonly reported complication, followed by tibial tuberosity fissure or fracture, infection, medial patellar luxation and fracture of the tibia (Kowaleski et al, 2018). Insufficient advancement and improper osteotomy placement as a result of technical errors was the main cause of the related complications. Despite this, good to excellent overall function (outcome and lameness) was reported by the owners in more than 90% of the dogs (Kowaleski et al, 2018). However, the long-term follow ups were limited to an average of 8–9 months and lacked objective data (Hoffman et al, 2006; Stein and Schmoekel, 2008; Dyall and Schmökel, 2017). Entoft et al (2023) reported a good to excellent long term outcome (at an average of 18 months) based on objective date obtained from a pressure sensitive walkway (Tekscan animal walkway). At the long-term follow up, there was no significant difference in weight-bearing when the operated leg was compared to the non-operated leg or when compared with a healthy control group (Entoft et al, 2023).
Several studies have compared tibial tuberosity advancement to other osteotomy procedures including tibial plateau levelling osteotomy, a procedure that has increased in popularity over the last decades (Bergh et al, 2014; Moore et al, 2020; Wemmers et al, 2022). Some studies showed an increase in development of osteoarthritis, postliminary meniscal tears and cartilage erosion with tibial tuberosity advancement compared with tibial plateau levelling osteotomy (Bergh et al, 2014; Moore et al, 2020; Jeong et al 2021), while other studies report a higher osteoarthritis score (based on radiological evaluation) after tibial plateau levelling osteotomy compared to tibial tuberosity advancement (Wemmers et al, 2022). Unfortunately, most studies lack high quality evidence, are retrospective, lack detailed outcome description as well as low numbers of included patients, leading to inconsistent results and questionable comparability (Wemmers et al, 2022). Further research, with randomised, surgical clinical trials is required to compare surgical techniques for cranial cruciate ligament disease in a controlled and standardised setting.
Meniscal injury
The meniscal injury remains a debated issue. The original tibial tuberosity advancement was performed without meniscal release, but it has been suggested that a meniscal release might be indicated to decrease the risk of late meniscal injury (Lafaver et al, 2007; Stein and Schmoekel, 2008). Voss et al (2008) reported an incidence of postoperative secondary meniscus damage after traditional tibial tuberosity advancement of 10% and can be up to 20% without meniscal release (Lafaver et al, 2007). A meniscal release aims to eliminate the wedge effect of the caudal horn of the medial meniscus during femorotibial subluxation. Both in vivo and ex vivo studies have investigated biomechanical and biological effects of meniscal release on joint function (Kennedy et al, 2005; Pozzi et al, 2008; Luther et al, 2009; Pozzi et al, 2010). Meniscal release leads to altered meniscal load transmission, increased meniscal instability and disturbed cartilage loading, ultimately leading to osteoarthritis by causing an upregulation in synthesis and degradation of cartilage matrix (Pozzi et al, 2008; Kuroki et al, 2011). Research has not yet been conclusive as to whether the meniscal injury originates from a latent tear or postliminary tear of an intact meniscus. The later may indicate that a meniscal release is necessary.
Aragosa et al (2022) critically reviewed the new generation tibial tuberosity advancement techniques. Their collected data from previous studies showed a decrease of late meniscal injury to 4.28%, which is similar to the rate of 4.70% reported by Dyall and Schmökel (2017). One theory for this lower number of late meniscal injury is that the newer generation implants may create a greater stability by improved implant design with, for example cages placed within the gap, compared with the traditional implant or the fact that the number of technical errors (leading to instability) have decreased with operator experience since the procedure was first established (Aragosa et al, 2022).
Meniscal release was not performed in any of the studies (n=16) with recorded late meniscal injury in the review, except one (Roydev and Goranov, 2021). Further prospective, long-term, standardised studies are needed before definitive conclusions can be made whether or not meniscal release should be performed in conjunction with tibial tuberosity advancement.
It is debated whether the persistent instability is an outcome from the technique itself or the consequence of improper execution of the technique and the pre-operative planning (Skinner et al, 2013). The new generation of tibial tuberosity advancement methods have been developed to decrease technical errors, including the use of a saw guide. Simultaneously, new concerns have developed. Among them is the potential for fractures of the tibial bridge at the distal end of the osteotomy or fracture of the diaphysis of tibia (Figure 2). To avoid such major complications, suggestions have been made regarding the length, curvature and orientation of the osteotomy, newer saw guides, width of the cage and modifications and/or supplementation of the distal aspect of the osteotomy.

Intraoperative complications
Dyall and Schmökel (2017) reported tibial tuberosity advancement rapid (Rita Leibeinger Medical; Germany) performed in 48 stifles of small breed dogs, with a good to excellent midterm outcome. Intraoperative complications consisted of four osteotomy-related fissures through the cranial cortex; two complete fissures were stabilised with a screw and the other two healed without intervention.
Two major complications occurred post-operatively, consisting of tibial fractures and needed a second surgery. Two late meniscal injuries, diagnosed with arthroscopy, were reported, resulting in a late meniscal injury rate of 4.7%, which is consistent with the results from Aragosa et al (2022). Six weeks postoperatively, limb function was good to excellent in 43 dogs (94%); the midterm outcome was rated excellent by 88% of the clients and good by 7% (Dyall and Schmökel, 2017).
Since 2019, the tiny tibial tuberosity advancement rapid technique has been available, with a new geometry of the cages accommodating for the larger advancement often needed in dogs with a large tibial plateau angle (present in many small breed dogs), combined with a shorter osteotomy cut. In dogs with a large tibial plateau angle, a longer osteotomy is necessary to achieve the desired advancement. Therefore, the osteotomy reaches the diaphysis of the tibia distal to the tibial tuberosity, increasing the risk for tibial diaphyseal fractures (Dyall and Schmökel, 2017). Such observations have prompted the development of the new geometry of the tiny tibial tuberosity advancement cages, allowing the cage to fit with a significantly shorter osteotomy (Figure 3). Entoft et al (2023) reported complications and long-term outcome in 23 small breed dogs treated with the new tiny tibial tuberosity advancement implants using objective data from a pressure-sensitive walkway analysis and found a major complication rate of 3% and a minor complication rate of 48%. The major complication consisted of an intraoperative fracture of the distal tibial tuberosity attachment with complete detachment in conjunction with implant placement that needed additional surgery. The minor complications consisted of a small cranial cortical fissure at the distal tibial tuberosity attachment visible on the postoperative radiographs. These were subperiosteal and were left to heal without additional stabilisation. The results from the pressure-sensitive walkway during the long-term follow-up showed no difference in maximum force and impulses when compared with a healthy control group. The study concluded that overall clinical outcomes were good to excellent in small breed dogs treated with the tiny tibial tuberosity advancement technique (Entoft et al, 2023)
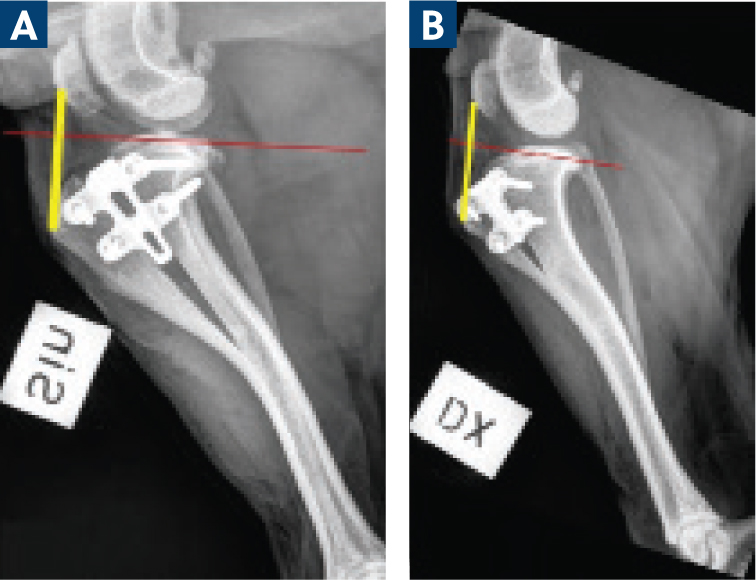
Results were similar in a prospective study evaluating short term outcome and complications in 65 cases treated with porous tibial tuberosity advancement with flange implant (Bernardi-Villavicencio et al, 2020). The study reported tibial tuberosity fracture and avulsion in 23 of the dogs, although none of them needed secondary surgical intervention. The reason for this was thought to be the fulfilling function of the flange, which minimised fragmental rotation and proximal displacement (Bernardi-Villavicencio et al, 2020).
Case selection
Suggestions for guidelines regarding case selection for the tibial tuberosity advancement procedure have been proposed, although no specific and universal guidelines exist. It has been proposed that the procedure is of advantage (theoretically) in preserving the proximal joint orientation line of the tibia (the tibial plateau). This has not been proven as an advantage post-operatively when compared to other surgical techniques for treatment of cranial cruciate ligament disease (Kowaleski et al, 2018). However, suggestions based on anatomical configurations have been made regarding when not to use the tibial tuberosity advancement technique. Anatomical configurations to be aware of in the decision making before a tibial tuberosity advancement surgery include a distal patellar ligament insertion point (short tibial tuberosity), an excessive tibial plateau angle and angular and/or torsional limb deformities (Boudrieau, 2009; Kowaleski et al, 2018). In these cases, the tibial tuberosity advancement procedure might not be the best option.
Distal patellar ligament insertion
Dogs of different breeds and sizes have different configuration of their tibial tuberosity. Individuals with a short tibial tuberosity tend to have a more distal insertion of the patellar ligament compared to dogs with a longer tibial tuberosity. With a distal patellar insertion point and short tibial tuberosity, a smaller size implant must be used compared to a high patellar insertion point and a larger tibial tuberosity. This could result in a less rigid construct, but no experimental or clinical studies support these assumptions (Boudrieau, 2009).
Excessive tibial plateau angle
Dogs with an excessive tibial plateau angle require a larger tibial tuberosity advancement to achieve a patellar tendon angle of 90°. A larger advancement requires a larger implant, which might not be possible to fit; many dogs with an excessive tibial plateau angle are small breed dogs (Selmi and Padilha Filho, 2001; Macias et al, 2002; Cosenza et al, 2015). Currently, the large advancement is limited to 18 mm (Rita Leibinger Medicals; Germany). However, the definition of an excessive tibial plateau angle in correlation with the tibial tuberosity advancement procedure is not defined. It has been proposed that dogs with a tibial plateau angle of >30° may not be good candidates for the tibial tuberosity advancement procedure (Boudrieau, 2009).
Angular limb deformities
Correction of angular and/or rotational limb deformities can be difficult in combination with the tibial tuberosity advancement procedure and is generally not recommended. This is because the tibial tuberosity advancement osteotomy is performed in the frontal plane, while corrections of tibial varus, valgus or torsion all require some form of transverse osteotomies. Therefore, a second transverse osteotomy is required in addition to the tibial tuberosity advancement. With the two different osteotomies, fixation techniques become challenging because both osteotomies must be secured; either an alternative fixation to secure the tibial tuberosity or a modification to the fixation across the transverse osteotomy is required (Kowaleski et al, 2018).
Since no definitive criteria of when the tibial tuberosity advancement procedure is recommended, a more appropriate approach in decision making is via case-by-case selection, ideally with the use of a digital template that can assist in planning the procedure based on the patients actual conformation and appropriate implant selection and position.
Conclusions
Tibial tuberosity advancement is a reasonable treatment option for cranial cruciate ligament repair, with expected good to excellent functional outcome in a variety of dogs provided the proper case selection.


