Applying topical medication is paramount when treating ocular surface disease and can prove challenging in fractious dogs. In equine ophthalmology, the use of subpalpebral lavage systems is commonplace with a low risk of complications (Sweeney and Russell, 1997). The use of ocular lavage kits has since been described in people (Meallet, 2006), llamas and a harbour seal (Borkowski et al, 2007). However, to the author's knowledge the use of this drug delivery technique has not been reported in dogs. This case series will describe the use of subpalpebral lavage systems in dogs with special emphasis on the placement technique. Case descriptions
Case 1
A male neutered Springer spaniel aged 7 years 11 months old presented with a non-healing ulcer in the right eye of 3 weeks' duration. According to the history, the dog had undergone multiple cotton-bud debridements and a grid keratotomy before referral. A bandage lens had been placed by the referring vet and removed 2 weeks after the grid keratotomy. The referring vet's topical medical treatment plan included chloramphenicol four times a day and oral meloxicam once a day. Upon presentation, there was marked blepharospasm in the right eye, copious amounts of mucoid discharge from the medial canthus, enophthalmos and third eyelid protrusion. There was mild conjunctival hyperaemia and chemosis, mild pancorneal oedema and a central superficial corneal ulcer with no signs of stromal infiltration. The remaining posterior segment of the right eye and examination of the left eye were unremarkable.
Schirmer tear tests were not performed, due to the dog's temperament. Intraocular pressures read 10 mmHg in the right and 12 mmHg in the left eye, using rebound tonometry (Icare TONOVET). Cytology and culture samples were obtained, revealing no signs of bacterial growth and no evidence of infectious agents upon cytology. Since the ulcer appeared to be healing, medical treatment was continued for another week.
When the dog was re-examined 1 week later, the owners had stopped all topical medication 2 days before presentation, since the dog had become aggressive when manipulated around the facial area. An abbreviated conscious ophthalmic examination was performed because of the dog's temperament. The ophthalmic findings were similar to the previous examination. Eye drops could not be applied and a non-healing ulcer was present, so the owners opted for surgical treatment.
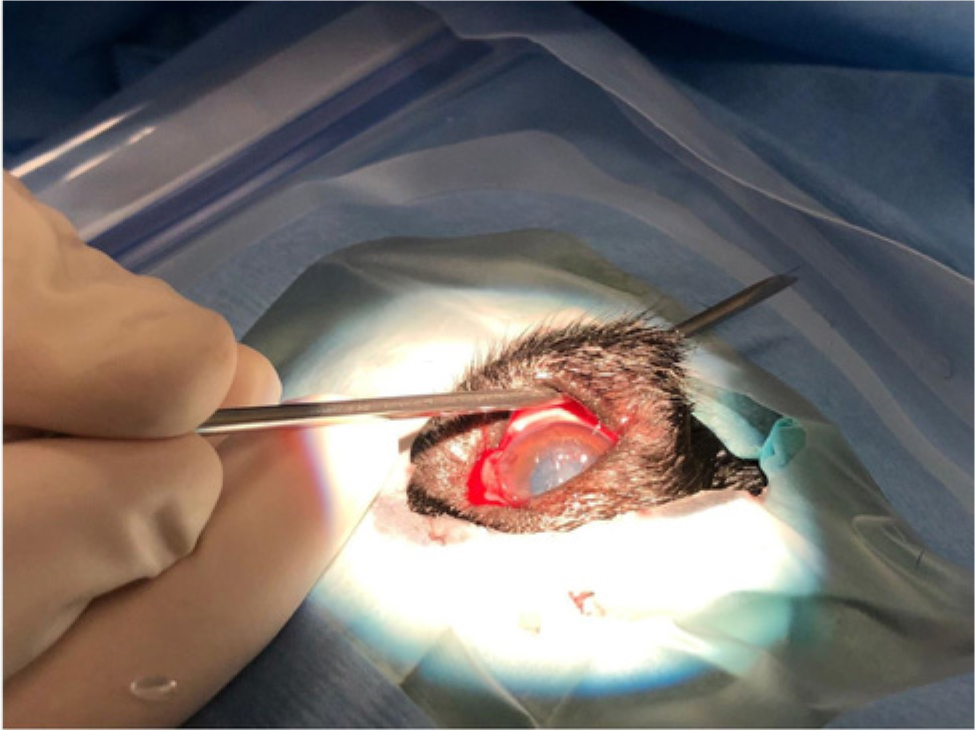
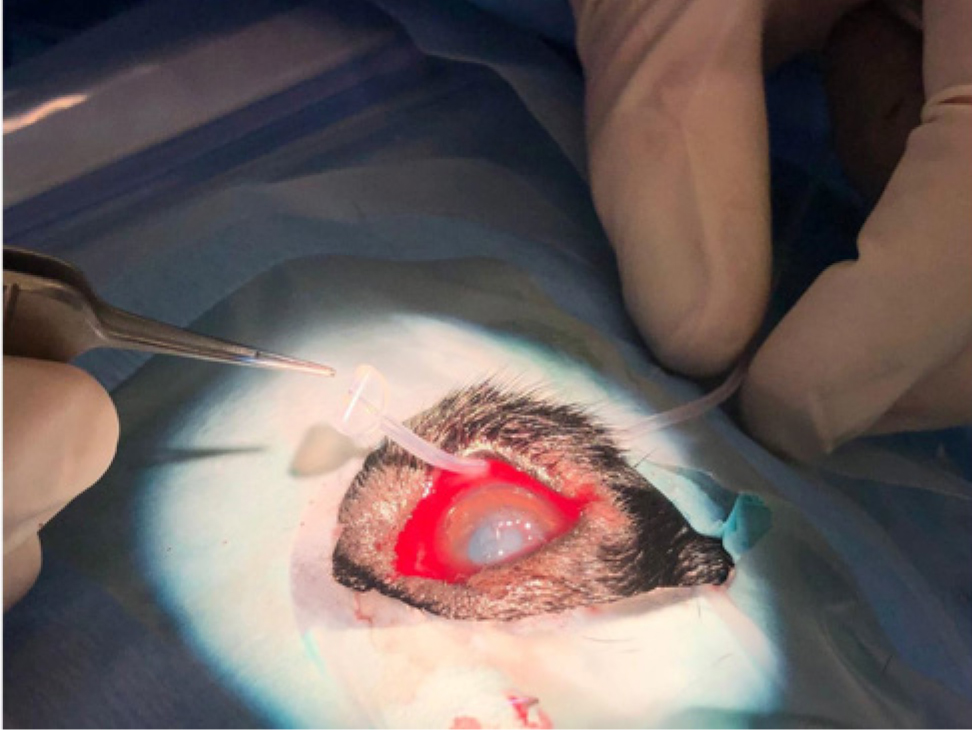
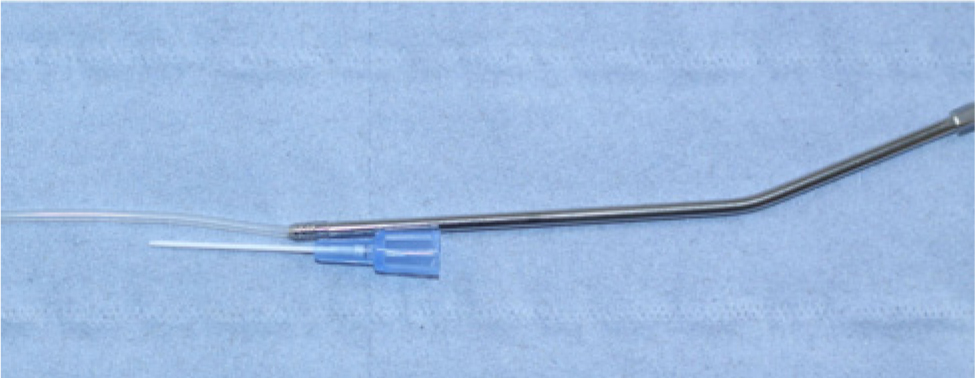
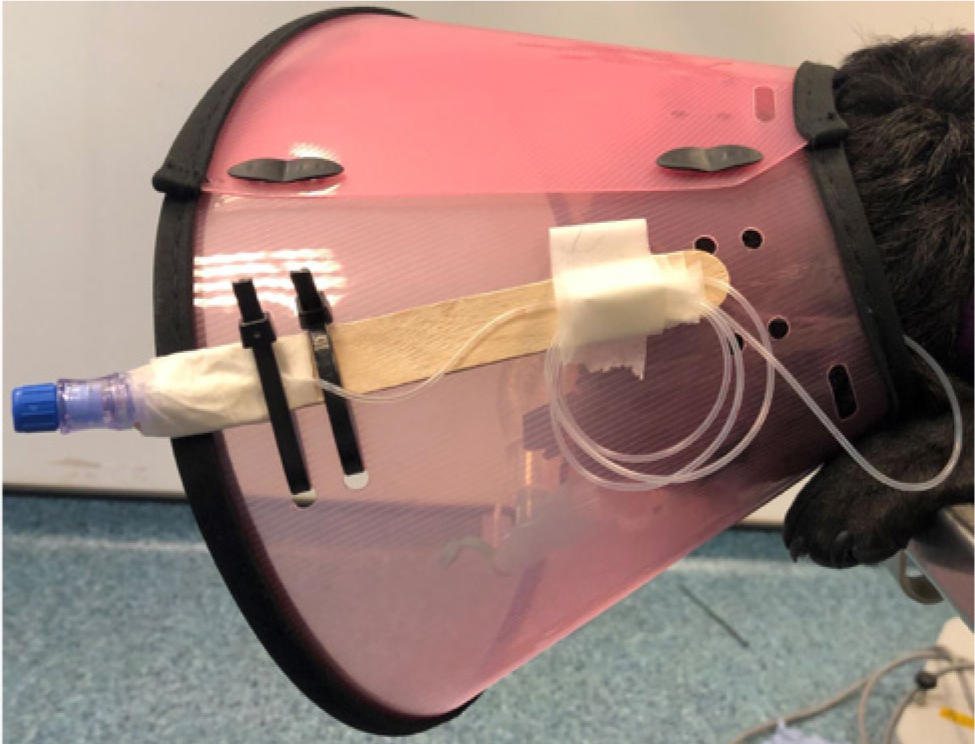
The ocular adnexa were explored under general anaesthetic. A small plant-based foreign body was identified deeply embedded behind the third eyelid. The foreign body was removed, a superficial keratectomy was performed and a bandage lens (PureVision, Bausch and Lomb, Ireland) was placed. An ocular subpalpebral lavage kit with a 10° angled trocar (EQUIVET Ocular Lavage 5 Fr, Denmark) was placed, with the footplate located in the dorsolateral conjunctival fornix (Figures 1and2). Care was taken to insert the lavage kit as deep in the conjunctival fornix and as close to the bony orbit as possible to reduce the risk of ocular surface irritation from the footplate. The tubing set was attached to the skin in three places (adjacent to the exit wound of the lavage kit through the conjunctival fornix, and along the dorsal skull) using 6/0 polyglycolic acid (PGA) suture (Optime 6/0, Péters Surgical) in a Chinese finger-trap technique. The trocar was removed from the silicone tube and a 22G intravenous cannula (Jelco Optiva IV Catheter, Smiths Medical International) was inserted at the distal end of the tube (Figure 3) and reinforced using micropore tape (Figure 4). The airlock-filter provided with the subpalpebral lavage kit was attached to the intravenous cannula to avoid contamination of the inside of the tubing set. The long end of the tubing set was attached to the Elizabethan collar (Smart Collar, MDC) using micropore tape and cable ties attahed to a wooden tongue depressor (Figure 5). A temporary tarsorrhaphy suture was placed in a cruciate pattern using 6/0 PGA (Optime 6/0, Péters Surgical).

FTopical medication was given via the subpalpebral lavage kit using 0.1 ml of the drug followed by 0.5 ml of air via a 1 ml syringe. Topical medication included chloramphenicol 0.5% (Ethypharm Group Company), heterologous serum and preservative free 0.4% sodium hyaluronate (Clinitas, Altacor) four times daily. Oral medication included oral 10 mg/kg doxycycline once a day (Ronaxan) and oral 0.2 mg/kg meloxicam once a day (Metacam, Boehringer).
The dog was hospitalised for 3 days post-surgery consecutively and a re-examination was performed under sedation 12 days after surgery. At re-examination the cornea had completely epithelialised and the eye was comfortably open. The remaining eye exam did not reveal any ocular abnormalities. The lavage kit was removed under sedation by cutting the silicone tube approximately 5 cm from the exit wound from the conjunctival fornix and carefully advancing the silicone tubing into the conjunctival fornix in a retrograde fashion. Once the footplate became visible, it was grasped and the remaining silicone tube removed.
Case 2
An eleven-month old male, intact Boston terrier presented with corneal ulceration in the right eye of one week's duration. It had already been treated with topical fusidic acid twice daily. Upon presentation the owners admitted that topical medical treatment was near impossible. An abbreviated ocular exam was performed due to the dog's reluctance to have its right eye manipulated. A paraxial midstromal ulcer with cellular infiltrate in the right eye was diagnosed. The rest of the examination was unremarkable apart from breed-related ocular brachycephalic syndrome. The left eye, was considered normal apart from breed-related brachycephalic ocular syndrome.
Cytology and culture samples of the corneal infiltrate were performed, confirming the presence of scant neutrophils and profuse growth of Enterobacteriaceae, which were sensitive to ofloxacin, chloramphenicol and neomycin but resistant to fusidic acid, flucloxacillin and oxytetracycline.
Due to the inability to apply intensive medical treatment in this fractious dog, it was decided to perform a keratectomy of the infected cornea surrounding the ulceration and repair the corneal ulcer via a corneoconjunctival transposition. Bilateral medial canthoplasties were performed at the same time to improve eyelid conformation and a subpalpebral lavage system (EQUIVET Ocular Lavage 5 Fr) was inserted in the ventrolateral conjunctival fornix to facilitate postoperative medical treatment of the cornea. A temporary tarsorrhaphy was placed to minimise eyelid movement and reduce the risk of irritation of the footplate of the ocular lavage system.
The lavage system was inserted in a similar fashion to Case 1 and attached to the Elizabethan collar (Smart Collar, MDC). Postoperative medical treatment included topical 0.3% ofloxacin (Exocin Allergan) four times a day, heterologous serum and preservative free 0.4% sodium hyaluronate (Clinitas, Altacor) four times a day in the right eye via the lavage kit and topical fusidic acid (Isathal 10 mg/g, Dechra Veterinary Products) twice daily, as well as direct application in the left eye of preservative-free 0.4% sodium hyaluronate (Clinitas, Altacor four times a day. Two days postoperatively the left eye had developed a superficial axial corneal ulcer in the left eye and cytology and culture samples revealed the same strain of Enterobacteriacae with similar culture sensitivity results. The topical treatment of the left eye was adapted to include 0.3% ofloxacin (Exocin Allergan) four times a day. The dog was amenable to treatment and manipulation around the left eye, so it was not thought necessary to place a lavage system and further intervene surgically.
Eight days after the initial surgery of the right eye, the corneal graft had integrated with no signs of cellular infiltrate or corneal malacia. The dog was anaesthetised to remove the subpalpebral lavage kit in the right eye (same procedure as in Case 1) and it was decided to perform a corneoconjunctival transposition in the left eye as corneal ulceration had progressed. The aftercare of the left eye was identical to the treatment of the right eye. Since directly applying eyedrops was still possible in the left eye, placing a lavage kit was not considered necessary. Twenty-two days after the initial operation, both corneal grafts had fully incorporated. Topical and systemic medication were discontinued.
A final re-examination was performed 2 months after the initial operation. At that point, both eyes were comfortably open and visual. The corneas of both eyes were given a corneal clarity score G4 (fine details of the fundic features are clearly visible with indirect ophthalmoscopy) (Sanchez et al, 2016). The remaining ocular exam was considered normal. The dog was signed off on prophylactic preservative-free 0.4% sodium hyaluronate (Clinitas, Altacor) twice a day in both eyes long term.
Case 3
A 2-year-old male neutered Lhasa Apso presented with corneal ulceration which had been present for a week in both eyes. The owners had been unable to apply topical medication. A complete ophthalmic examination could only be performed by sedating the dog because of its aggressive demeanour. Upon examination, bilateral brachycephalic ocular syndrome with medial entropion was present in both eyes. Both corneas had an axial midstromal ulcer with signs of cellular infiltrate. The remaining ocular examination was considered normal.
Schirmer tear tests (MSD Animal Health) under sedation read 12 mm/min and 13 mm/min and intraocular pressures measured using rebound tonometry (ICare, TONOVET) read 9 mmHg in the left eye and 13 mmHg in the right eye. Corneal cytology and culture samples were obtained from both corneal ulcers, revealing light growth of Staphylococcus species in both eyes, which were sensitive to chloramphenicol, ofloxacin and neomycin but resistant to fusidic acid and flucloxacillin.
Surgical repair of the corneal ulcers in both eyes via corneoconjunctival transposition was recommended and performed. Bilateral medial canthoplasties and insertion of subpalpebral lavage kits (EQUIVET Ocular Lavage 5 Fr Kit, Kruuse A/S) were performed at the same time. The lavage systems were inserted in a similar fashion to Case 1 and Case 2, exiting from the ventrolateral conjunctival fornix. However, the silicone tubes were not attached to the skin via a Chinese finger-trap suture technique. Instead, the lavage kit trocars were used to tunnel the skin in two areas (close to the exit wound from the ventrolateral eyelid and paraxial on the forehead) to reduce the risk of suture breakdown and migration of the lavage kit footplates (Figure 6).

Temporary tarsorrhaphy sutures were not placed. The remaining tubing set was attached to the Elizabethan collar (Smart Collar, MDC) in the same fashion as in Case 1. Postoperative treatment was the same as in Case 2. The dog was reviewed again 12 days after the initial surgery. The animal was sedated to have the lavage systems removed, and a complete ophthalmic examination of both eyes was performed. The lavage systems were removed in the same fashion as in Cases 1 and 2. At the ophthalmic examination, both corneal grafts had fully incorporated and there was evidence of pigment migration into the corneal part of the graft in both eyes. The remaining ocular exam was unremarkable.
Due to the dog's demeanour the owner was unable to apply topical ciclosporin to counteract pigmentation of the cornea and progression of the pigmentation was evident at the final follow-up appointment 1 month after the initial surgery. The dog was lost to further follow-up.
Case 4
A female neutered pug aged 4 years 5 months presented with ocular discomfort that had been present in the left eye for a day. It was impossible for the owner to approach the left eye. Upon ophthalmic examination there was significant blepharospasm in the left eye. Upon distant examination and a ‘hands-off’ detailed examination using a slit lamp biomicroscope (SL-17 slit lamp, Kowa Co) an axial pinpoint deep stromal ulcer with surrounding cellular infiltrate was noted in the left eye. Breed-related brachycephalic ocular syndrome with medial entropion was present in both eyes. The remaining ophthalmic examination was not possible due to the dog's aggressive behaviour. Topical medication could not be applied, so it was decided to surgically repair the stromal ulceration and place a subpalpebral lavage system at the same time.
Corneal repair was performed via a corneoconjunctival transposition. Bilateral medial canthoplasties were performed at the same time. Intraoperative cytology and culture samples of the corneal ulcer were obtained. There was no evidence of infectious agents and no growth upon culture. A subpalpebral lavage system (EQUIVET Ocular Lavage 5 Fr Kit, Kruuse A/S) was inserted into the left eye through the dorsolateral conjunctival fornix at the conclusion of the surgery. A lateral temporary tarsorrhaphy suture was placed at the same time to minimise eyelid movement and reduce the risk of corneal irritation due to the foot plate. The silicone tubing set was tunnelled through the skin in two locations using the same technique as in Case 3.
Postoperative medical treatment was the same as in Cases 2 and 3. The owner presented the dog 9 days after the initial surgery due to concerns regarding patency of the tubing set. At examination, both eyes were comfortably open. There were copious amounts of mucoid discharge from both eyes, as a result of the owner being unable to clean the periocular region. A detailed examination was performed while the dog was sedated. At examination, the lavage system was in place and patent. The graft had fully integrated into the surrounding cornea with minimal vascularisation. The lavage system and remaining eyelid sutures were removed. Topical ciclosporin treatment was recommended to avoid corneal pigmentation but it proved impossible for the owner to apply due to the dog's demeanour. The dog was lost to follow-up.
Discussion
Subpalpebral lavage systems are widely used in equine ophthalmology and considered a safe means of providing topical medication to the eye in horses that are otherwise resistant to direct application of eyedrops or have severely traumatised globes at risk of rupture (Dwyer, 2017). The tubing set is typically placed in sedation in standing horses after regional anaesthesia and eyelid akinesis, and can be placed in the upper or lower eyelid medially or laterally depending on the surgeon's preference (Dwyer, 2017).
Since its' original description, there have been reports of variations in the placement technique of the lavage system (Dennis et al, 2019; Giuliano et al, 2000). Although the use of subpalpebral lavage systems is generally considered safe, there is a large retrospective study of complications associated with this drug delivery technique in horses. In that study, 24% of 150 horses developed severe complications including corneal ulceration, eyelid infection and loss of the footplate in the eyelid. The main conclusion of that study was that special care and attention regarding the size of the footplate and placement of the lavage system can decrease the overall complication rate, but that minimal swelling of the eyelid within the first 48 hours after placement is expected (Sweeney and Russell, 1997). Since the first description of the use in horses, there have been case descriptions of subpalpebral lavage systems in humans (Meallet, 2006), llamas and a harbour seal (Borkowski et al, 2007). However, to the author's knowledge, this is the first case description of the use of this drug application technique in dogs.
There are various diameters and lengths of silicone tubes depending on the manufacturer and a variety of trocars available. The author prefers the lavage system used in this case description because of the diameter and length of the tubing set, as well as the curved trocar which reduces the risk of accidentally applying pressure to the globe during the insertion through the conjunctival fornix. To the author's knowledge there are no commercially available subpalpebral lavage systems dedicated for use in small animals to date.
Although all lavage systems were placed by the same surgeon, there was some variation in the placement technique. Based on the small case number it is impossible to statistically evaluate whether the lavage system is best placed in the dorsolateral or ventrolateral conjunctival fornix. The decision was made on a case by case basis to best suit the facial conformation of the dog (Figure 7). The mediodorsal and medioventral conjunctival fornix was not attempted because of close proximity with the nose, which rendered any attempt to insert the trocar through the fornix extremely challenging. Placement of a temporary tarsorrhaphy suture was performed on a case by case basis and included factors such as the surgical procedure which was performed, the facial conformation of the dog, as well as the ability to monitor the healing process once the dog had recovered from anaesthesia.

The decision to tunnel the silicone tubing through the skin in the latter cases was made, due to concerns about suture breakdown and loosening of the tubing set during the daily routine of active dogs. The author felt that dogs were more inclined to attempt to rub their heads against objects than horses, which could result in suture breakdown, requiring further sedation/anaesthesia before the lavage system could be removed.
The subdermal tunnel technique described here, did not result in any noticeable complications and the skin wounds healed uneventfully in all cases once the silicone tubing had been removed. However, further prospective studies on larger case numbers to determine the best placement technique, as well as the benefits of temporary tarsorraphies, are warranted.
In conclusion, to the author's knowledge this is the first case series describing the use of subpalpebral lavage systems in fractious dogs. No major complications were encountered and owners were able to apply medications via the lavage system in all cases.

