Case presentation
A 12-year-old female bearded dragon that weighed 390 g presented at the clinic with anorexia, straining and lack of defaecation. The animal was housed on sand and had provision of both heat and UVB via lamps. The patient was alert during examination but showed discomfort during coelomic palpation. A hard 6–7 cm long, 2–3 cm wide mass could be palpated on the left side of the coelom. Dorsoventral whole body radiographic imaging showed large amounts of mineral opacity material in the intestines on the left side of the animal (Figure 1).

The diagnosis was consumption of substrate (sand) because of a low-calcium diet, with consequential gastrointestinal impaction. The animal was hospitalised and with bathing, enemas and vibration therapy (gentle vibrations transmitted via a vibrating surface), the large amount of sand was passed. Afterwards, a 4 cm wide soft mass could still be palpated in the mid-coelom. Ultrasound examination was recommended to the owner, but was declined at this stage. The animal started eating after 2 weeks and was active, but soon started to show signs of kyphosis (Figure 2).

The clinical signs progressed quickly, and the animal represented to the clinic. Faecal smears were unremarkable but the mass was still palpable, so examinations were undertaken to help diagnose the underlying cause and plan potential surgery if possible.
Diagnostic assessments
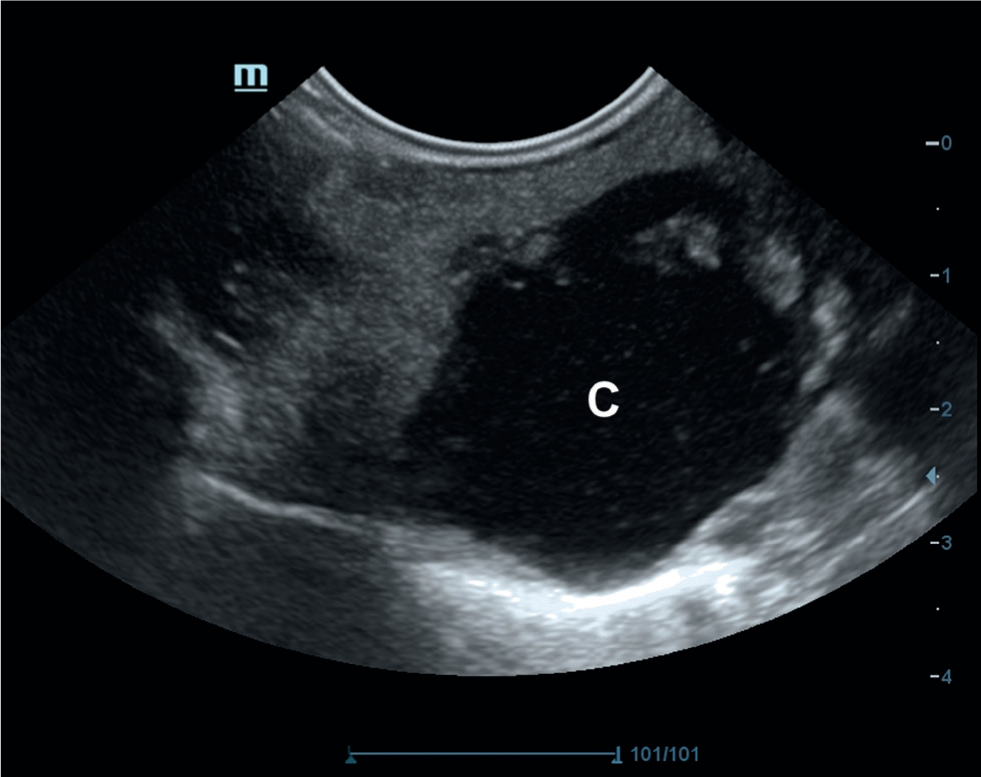
Coelomic ultrasound was performed using a linear 14Mhz and a microconvex 8 Mhz probe (Mindray DC 80A X-Insight machine). The ultrasound showed an enlarged liver with an abnormal form and contour. A fluid filled cyst, 4 cm in diameter, could be seen protruding from the right liver lobe and appeared to be connected to the liver tissue. The fluid was filled with echogenic particles. Cytological sample collection was not performed as there was concern the cyst may have been an abscess. The gallbladder was moderately full, more laterally placed and was not connected to the cyst. The other organs were deemed normal on examination (Figure 3).
Radiography was repeated with knowledge of the results of the ultrasonographic examination. A soft tissue opacity, approximately 4 cm in diameter, was observed on the right side of the coelom, in the area of the structure. This mass contained some small mineral opacity grains. Mineral opacity material was no longer present in the intestines, probably because of the sand substrate having been removed from the enclosure (Figure 4).

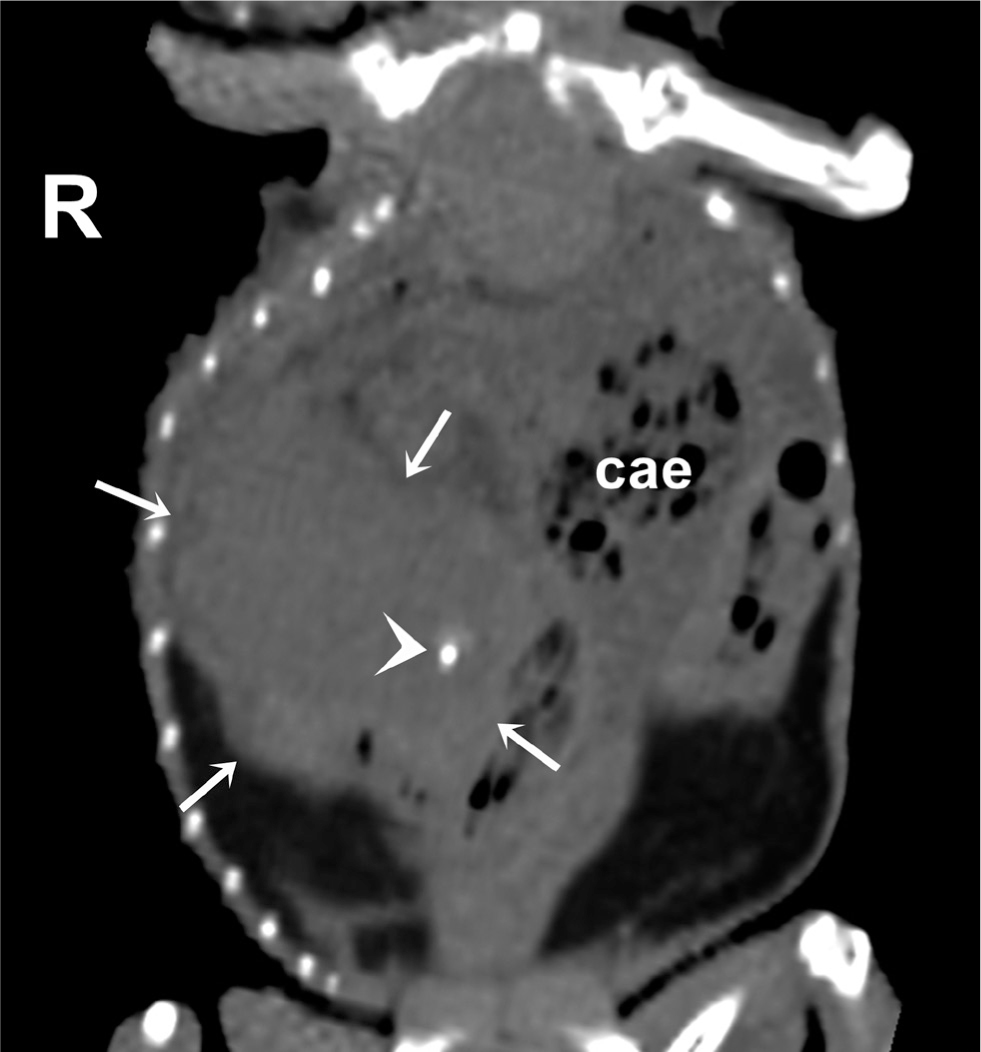
Non-contrast computed tomography was performed without general anaesthesia on a 16-slice computed tomography (CT) scanner (GE Revolution ACT, GE). Imaging parameters were sternal recumbency, helical acquisition, pitch 0.625, rotation speed 1s, 0.625 mm slice thickness, 120kVp, 50–80 mAs, and matrix 512 × 512 with the field of view adjusted for the animal size. CT images were displayed in a soft tissue window (Window width: +400; Window level: +40).
A 35x21x25 mm sized soft homogenous soft tissue structure was visible on the right side of the coelomic cavity, in contact with the coelomic wall. Inside the structure, a few 1–4 mm diameter mineral opacity granules were detected, with the highest density value of 1022 HU. The colon was dislocated to the left side. At the location of the gallbladder, an 18 mm diameter round hypoattenuating structure was visible, with two oval soft tissue structures inside that completely filled the lumen of the structure (Figure 5).
As the bearded dragon was showing signs of discomfort, and the diagnostic tests did not show any contraindication to surgery, an exploratory laparotomy was undertaken to remove the cyst.
Treatment
The animal was premedicated using 1 mg/kg meloxicam (Melosolute 5 mg/ml, CP-Pharma Handelsgesellshaft mbH) and 1 mg/kg butorphanol (Alvegesic 10mg/ml, ALVETRA u. WERFFT GmbH) both administered subcutaneously. A further 7 ml of 0.9% sodium-chloride (Fresenius infusion solution, Fresenius Kabi Deutschland GmbH), 1 ml of infusion containing amino acids, vitamins and electrolytes (Duphalyte, Pfizer Kft), and 0.5 ml of glucose (Glükóz 40% infusion, WERFFT-PHARMA Kft) were administered subcutaneously preoperatively. General anaesthesia was induced with 5 mg/kg of propofol (propofol 1% MCT/LCT, Fresenius Kabi Deutschland GmbH) administered intravenously. The animal was then intubated and then started on 5% volume-to-volume (v/v) isoflurane (Isoflutek, 1000mg/g, Laboratorois Karizoo), before being maintained with 2.5% v/v isoflurane using 100% oxygen at 1.5 litres flow. The animal was then placed in dorsal recumbency. The site was scrubbed with disinfectant liquid containing ethanol, alkyl dimethyl benzyl ammonium chloride, dodecyl dimethyl ammonium chloride, caprate and C8-C14 alkyl glucoside (Bradonett, Florin Zrt), treated with disinfectant containing ethyl-alcohol and alkyl dimethyl benzyl ammonium chloride (Bradoderm Soft, Florin Zrt.), then isolated using a sterile surgical drape. A paramedian coeliotomy was performed. The surgical incision was made where the coelomic wall was protruding because of the mass. A large fluid filled mass with an uneven surface became visible (Figure 6).

The mass was surrounded by the right liver lobe but was only connected to it via a small segment, which also contained smaller masses of about 1 cm in diameter. Another neighbouring segment of the liver also contained small masses. Both liver segments, as well as the lesion, were removed. These tissue samples were fixed in 4% buffered formaldehyde solution and sent for histopathology, along with a sample of fluid from the cyst for cytology. The partial lobectomy was performed using a guillotine method for blunt crushing of the tissues and ligation of the vessels with 4/0 polidioxanone (PDX, Vetsuture). A bipolar electrosurgical device (Eickemeyer radiofrequency electrosurgery unit) was used where larger vessels in the liver could be seen. Gelatine sponge (Spongostan Dental, Johnson and Johnson) was also applied to the site to decrease the chance of postoperative haemorrhage. Adhesions could be seen in the coelom, but other abnormalities were not visible. The coelom was closed in two layers. The muscles were sutured using a simple continuous suture pattern (4/0 PDX), and the skin using horizontal mattress sutures (4/0 PDX).
Postoperative management included subcutaneous injection of 1 mg/kg meloxicam daily for 2 weeks. This high dose of meloxicam was used because of the anticipated and observed signs of pain pre- and post-surgery. To try to mitigate the risks to the liver and kidneys, 10 ml 0.9% sodium-chloride was administered by subcutaneous infusion daily for 5 days. As a small amount of serous-bloody fluid was draining from the wound over the first 5 days, 10 mg/kg marbofloxacin (Marbocyl 100 mg/ml inj, Vetoquinol) was administered subcutaneous daily for 10 days.
Follow up
Blood was obtained for haematological and biochemical evaluation 5 days after surgery. Although not always reliable, even after such a large surgery involving the manipulation of the liver, bloods still give an indication of body processes. In this case the parameters, including hepatic and renal values, were all in normal range and showed no abnormalities.
The cytological sample obtained during surgery showed no cells in the fluid from the cyst, although some bile containing crystal-like structures was visible, with calcium carbonate-like material present (Figure 7).
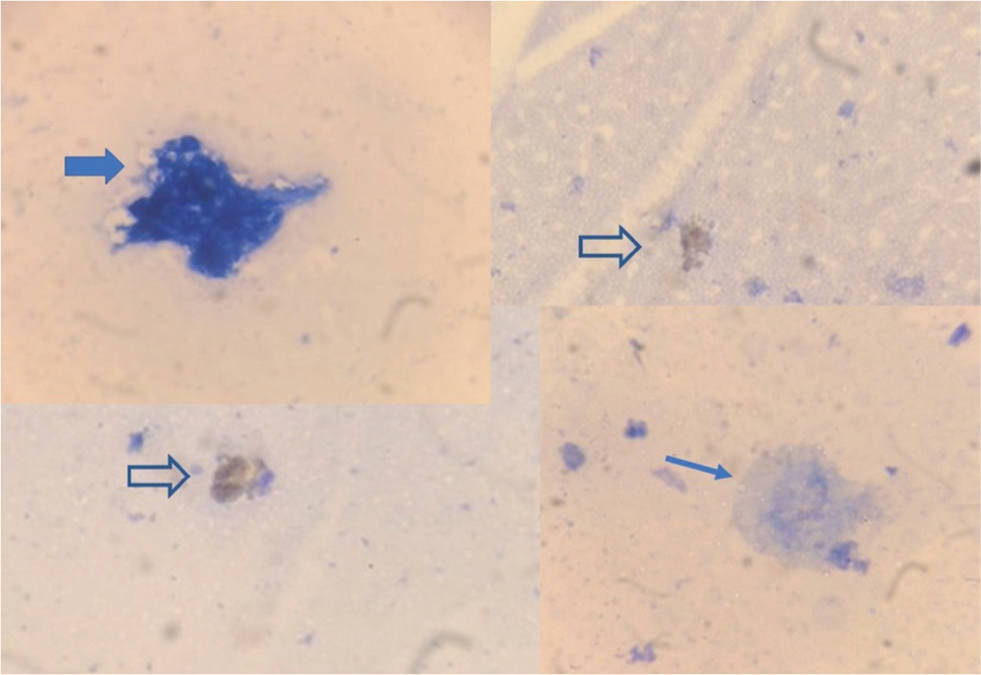
This latter showed bubble formation after dripping a 10% commercially available acetic acid solution on to it. This was visible during microscopic examination at 100 power using Nikon Eclipse E400 (Nikon Corporation, Tokyo, Japan).
Histopathological examination showed that the cyst contained condensed secretions on parts of the inner surface. The epithelial lining was intact with no pathological changes visible (Figure 8).
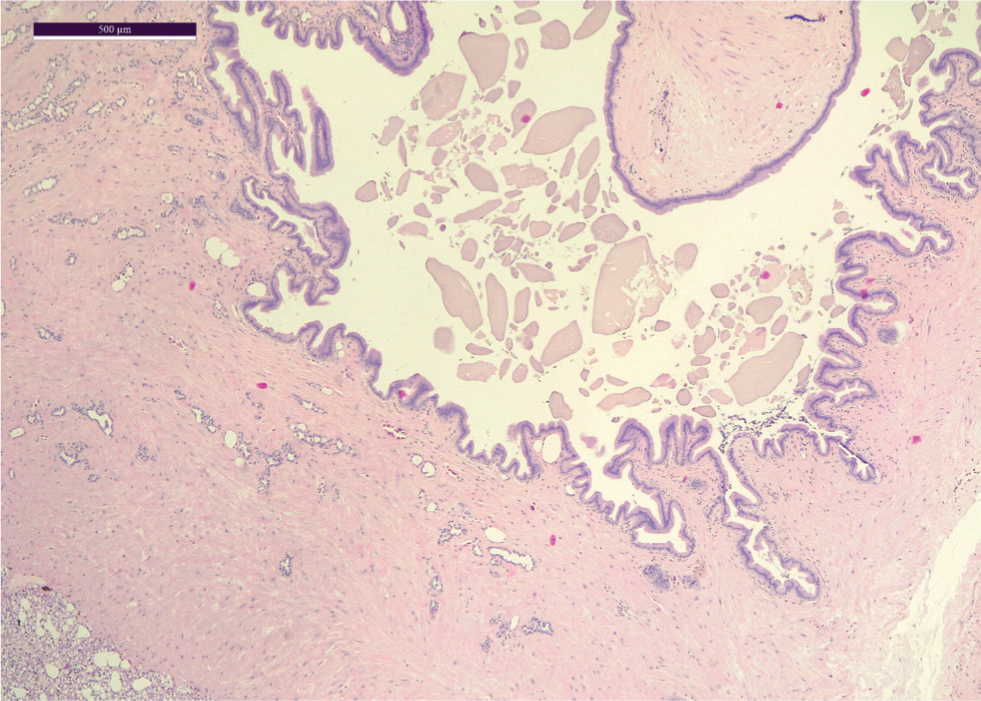
The hepatic tissue structure around the cyst was disintegrated, with signs of fresh bleeding and diffuse vacuolar degeneration. The hepatic cells, containing mostly one large vacuolum, were irregularly shaped and showed a messy diffuse proliferation, with portal areas recognisable in some. Melanin-containing cells were mostly present, but there were some well-defined foci where these were completely missing. Various sized regenerative nodules were present on the samples. No signs of neoplastic lesions or inflammation were present on either sample submitted. The samples showed bile-duct cysts with hepatic lipidosis, hepatocellular degeneration and secondary regenerative liver tissue foci.
Now 8 months post-surgery, the bearded dragon is active, eating and defaecating regularly. The coelom is not painful and no irregular structures can be palpated.
Diagnosis
The bearded dragon had idiopathic bile duct cysts, and the diagnosis was made with the help of the histopathological evaluation.
Discussion
The bearded dragon first presented with consequential impaction and constipation from ingestion of sand, which is a common problem in lizards on an inadequately low calcium diet or with inappropriate substrate (Nógrádi and Dunay, 2013). The authors used bathing and enemas to loosen the faeces, and vibration therapy to encourage the lizard to pass the sand more quickly. In more severe cases, parenteral fluid therapy can also be used. However, it is possible that the cyst, which was palpable after the impaction passed, contributed to the abnormal function of the gastrointestinal tract, owing to distension and compression of the coelomic contents. The authors opted for surgery, using both butorphanol and higher dose meloxicam to premedicate the animal. The use and effectiveness of opioids is an on-going area of research in reptiles, but in this instance butorphanol was used as no other opioid was available at the time and there was a need for sedation and pain relief. Fluid infusions were also given during the surgery as both anaesthesia and meloxicam can decrease the kidney function, particularly if blood pressure decreases. During surgery the presence of adhesions suggested a level of chronicity and coelomic inflammation, probably as a result of the presence of the cyst.
A distended coelom in lizards can have various causes. One such cause can be liver enlargement, which may be caused by hepatic lipidosis, granulomatous inflammation, bacterial or fungal granulomas, parasitic cysts, haematomas or neoplasia (Barten and Simpson, 2019; Komenda et al, 2020). Parasites in the liver and biliary tree are relatively common in reptiles, and though some parasites can cause high morbidity and mortality, they do not always cause disease and animals can appear healthy even with heavy infections and damage to the gallbladder epithelium (Lainson and Paperna, 1999; Schwartz et al, 2020). In the presented case, no macroscopic, cytological or histopathological signs of parasites were seen. No bacteria or fungi or any of the aforementioned lesions were seen upon gross, cytological or histopathological examination either. As a result, no culture was performed.
Lizards do have a gallbladder and even though they are not common, choleliths have been reported in them in the past, even in the bearded dragon (Frye, 1991; Diaz-Figueroa and Mitchell, 2006; Colon, 2013). The gallbladder was intact in the presented case. Secretion was visible in the removed cyst, but it crumbled upon manipulation and was not firm. Cholelithiasis was not the cause of the cyst in the presented case.
Caroli's disease in humans is a rare condition with the multifocal segmental dilatation of the intrahepatic bile ducts causing recurrent cholangitis. There is a simple form occurring alone and another with congenital hepatic fibrosis. In approximately 7% of cases, malignancy is present (Taylor and Palmer, 1998). Congenital dilation of the bile duct has been studied in various species, including dogs (Görlinger et al, 2003). The presented case also had dilated bile ducts, causing small masses and a large cyst of unknown developmental origin. However, there were no biochemical abnormalities, and no other clinical signs apart from kyphosis. As the bearded dragon in this case was an older individual, the disease was most probably not congenital. In this case, neither cytology, nor histopathology confirmed the lesions to be tumours.
As descriptions on hepatic lesions in bearded dragons found in the literature are scarce and mostly come from post-mortem analysis, the authors think it is important to address the clinical point of view of partial hepatectomy in the bearded dragon. The technique used in small animal medicine can be used just as well in these animals, and surgical management of hepatic lesions is possible. Their presence does not necessarily mean the animal needs to be euthanised. The case presented shows the clinical signs, diagnosis and surgical management of idiopathic bile duct cysts in a bearded dragon.
KEY POINTS
- Correct husbandry and care for exotic species is essential for good health and wellbeing. Substrate ingestion is common in reptiles and can cause impaction and constipation.
- Reptiles can get a coelomitis, similar to peritonitis, with resulting fluid, adhesions and inflammation.
- Liver disease is fairly common in reptiles and can have numerous causes.
- Diagnostics should be performed including bloods, ultrasound, radiographs and biopsies. It is important not to rely on one diagnostic tool alone as disease processes can easily be missed.
- Surgical techniques used in small animal medicine and surgery can be used and transferred when treating similar diseases in reptile patients.


